Abstract
Background
Although closed reduction and percutaneous pinning is accepted as the treatment of choice for displaced supracondylar fracture of the humerus, there are some debates on the pinning techniques, period of immobilization, elbow range of motion (ROM) exercise, and perceptions on the restoration of elbow ROM. This study was to investigate the consensus and different perspectives on the treatment of supracondylar fractures of the humerus in children.
Methods
A questionnaire was designed for this study, which included the choice of pinning technique, methods of elbow motion, and perception on the restoration of elbow ROM. Seventy-six orthopedic surgeons agreed to participate in the study and survey was performed by a direct interview manner in the annual meetings of Korean Pediatric Orthopedic Association and Korean Society for Surgery of the Hand. There were 17 pediatric orthopedic surgeons, 48 hand surgeons, and 11 general orthopedic surgeons.
Results
Ninety-six percent of the orthopedic surgeons agreed that closed reduction and percutaneous pinning was the treatment of choice for the displaced supracondylar fracture of the humerus in children. They showed significant difference in the choice of pin entry (lateral vs. crossed pinning, p = 0.017) between the three groups of orthopedic surgeons, but no significant difference was found in the number of pins, all favoring 2 pins over 3 pins. Most of the orthopedic surgeons used a removable splint during the ROM exercise period. Hand surgeons and general orthopedic surgeons tended to be more concerned about elbow stiffness after supracondylar fracture than pediatric orthopedic surgeons, and favored gentle passive ROM exercise as elbow motion. Pediatric orthopedic surgeons most frequently adopted active ROM exercise as the elbow motion method. Pediatric orthopedic surgeons and general orthopedic surgeons acknowledged that the patient's age was the most contributing factor to the restoration of elbow motion, whereas hand surgeons acknowledged the amount of injury to be the most contributing factor.
Supracondylar fractures of the humerus are the most common fractures in children1) and are managed frequently by orthopedic surgeons with other subspecialties than pediatric orthopedic surgery.2) Therefore, it may be difficult for orthopedic surgeons to reach a consensus on the treatment of supracondylar fractures of the humerus in children. However, no study has examined the consensus of treating orthopedic surgeons regarding the treatment strategy.
In medical research, it is important to develop better treatments, even though this is sometimes risky and uncertain. However, in clinical practice, it is safe, valuable and reasonable to take a consensus on a particular treatment based on current evidence or even insufficient evidence. Therefore, physicians need to have consensus on common diseases to avoid malpractice and medicolegal problems, particularly when they are managed by physicians with various subspecialties.
Although it appears that most orthopedic surgeons agree that the initial treatment for a displaced supracondylar fracture is a closed reduction and percutaneous pinning,1,3-8) there is some controversy or no evdidences regarding the pinning techniques,9) period of immobilization, postoperative rehabilitation and medication.10-13) These different strategies need to be highlighted for orthopedic surgeons to reach a consensus in clinical practice.
This study examined the different perspectives on fixation techniques and postoperative protocol in treating supracondylar fractures of the humerus in children using a specifically designed questionnaire.
This study was exempted from institutional review board approval at our hospital (a tertiary referral center for orthopedic surgery) because the study materials did not involve human subjects.
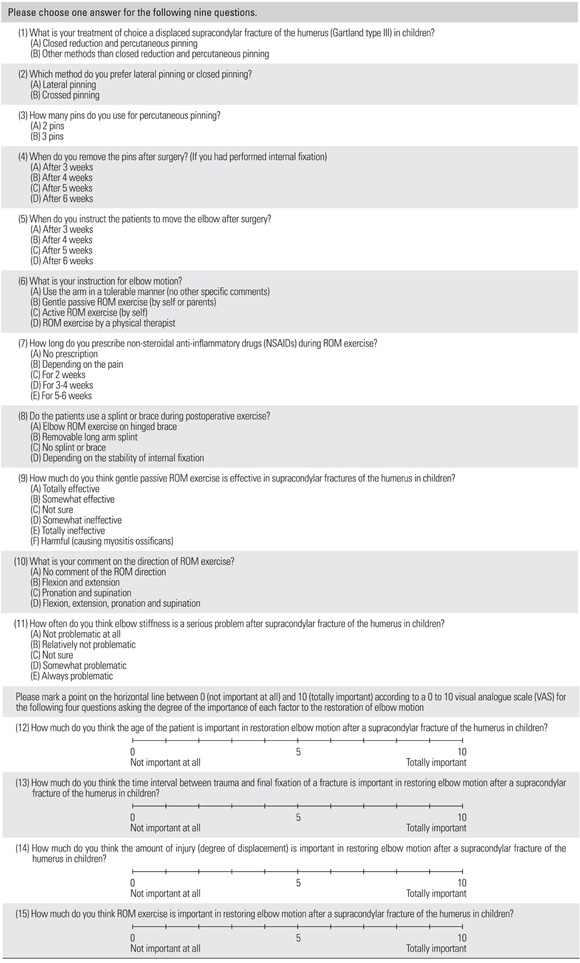
A 15-item questionnaire regarding the treatment of displaced supracondylar fractures of the humerus in children without neurovascular complication was designed by three pediatric orthopedic surgeons and one hand surgeon. The questionnaire was completed through direct interviewing by two orthopedic surgeons. The questionnaire survey was performed at the annual meetings of Korean Pediatric Orthopedic Association and Korean Society for Surgery of the Hand in 2010. The subspecialties of the participants were obtained and divided into three groups; 1) pediatric orthopedic surgeons, 2) hand surgeons, and 3) general orthopedic surgeons. Pediatric orthopedic surgeons had undergone at least one year of a pediatric orthopedic fellowship and more than 60% of their clinical practice was devoted to pediatric orthopedic surgery. Hand surgeons had undergone at least one year of hand surgery fellowship and more than 60% of their clinical practice involved hand surgery. General orthopedic surgeons were surgeons that had an orthopedic board certificate without any further subspecialty fellowship.
The participants were asked to answer the first nine questions in a single choice manner, which included choice of pinning techniques, methods of range of motion (ROM) exercise, immobilization during ROM exercise, medication, and the perception on the ROM exercise and elbow stiffness. An additional four questions were asked regarding the contributing factors to the restoration of the ROM after a supracondylar fracture of the humerus. For these questions, the participants were instructed to answer according to a 0 to 10 visual analogue scale (VAS) (Appendix I).
Statistical analysis was performed using SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA). All frequencies are expressed as a percentage. The averaged values are expressed as the mean and standard deviation. The chi-square test was performed for the choice of treatment strategies. The data normality was tested using a Kolmogorov-Smirnov test, and the three groups were compared using Kruskal-Wallis test. A p < 0.05 was considered significant.
Of the 130 orthopedic surgeons invited, a total of 76 orthopedic surgeons agreed to participate (response rate 58%). Of these, 17 were pediatric orthopedic surgeons, 48 were hand surgeons, and 11 were general orthopedic surgeons.
Most orthopedic surgeons (96%) agreed that the treatment of choice for displaced supracondylar fractures of the humerus in children is closed reduction and percutaneous pinning. Three orthopedic surgeons chose other methods than closed reduction and percutaneous pinning, all of whom were hand surgeons. There was significant difference in the choice of entry of pinning (lateral pinning and crossed pinning) between the three groups (p = 0.017) (Fig. 1). General orthopedic surgeons tended to prefer lateral pinning technique to crossed pinning technique, and no significant difference was found between the pediatric orthopedic surgeons and hand surgeons in the choice between lateral and crossed pinning techniques (p = 0.279). There was no significant difference in the number of pins between the three groups (p = 0.157), all favoring the use of 2 pins over three pins. Combining the entry of pinning and pin numbers, lateral 2 pins was the most favored method in pediatric orthopedic surgeons and general orthopedic surgeons (41% and 73%, respectively) while crossed 3 pins was the most preferred method in the hand surgeons (46%).
The pins were removed most frequently after 4 weeks in all three groups of orthopedic surgeons. Most pediatric and general orthopedic surgeons (75%) instructed the patients to move their elbow after postoperative 3 to 4 weeks, whereas 33% of hand surgeons instructed their patients to move their elbow after 5 weeks (p = 0.446). Pediatric orthopedic surgeons most frequently favored active ROM exercise, but hand surgeons and general orthopedic surgeons favored gentle passive ROM exercise (Fig. 2). However, the three groups did not show significant difference in the choice of elbow motion (p = 0.600). Most surgeons did not prescribe non-steroidal anti-inflammatory drugs or prescribed them according to the patients' pain, and a removable splint was the most preferred immobilization during the exercise period in all three groups. Pediatric orthopedic surgeons answered most frequently that gentle passive ROM exercise after supracondylar fracture of the humerus in children would be harmful, and hand surgeons and general orthopedic surgeons answered most frequently that they were unsure of the effect of elbow ROM exercise (Fig. 3). However, they did not showed significant difference in their responses between the groups (p = 0.605). The majority of orthopedic surgeons recommended pronation and supination as well as flexion and extension when they instructed their patients to move their arms in all three groups. Pediatric orthopedic surgeons most frequently answered that elbow stiffness after a supracondylar fracture of the humerus in children is 'not problematic at all', whereas hand surgeons and general orthopedic surgeons were more conservative in that elbow stiffness is 'relatively not problematic' (p = 0.05) (Fig. 4).
The most contributing factor to restoring the elbow ROM after a supracondylar fracture in children was the patient's age, followed by the interval between trauma and final fixation, ROM exercise, and the amount of injury in terms of pediatric orthopedic surgeons and general orthopedic surgeons' perspectives. On the other hand, most contributing factor to restoring the elbow ROM was the amount of injury, followed by ROM exercise, the patient's age, and the interval between the trauma and final fixation in the hand surgeon group. However, there were no significant differences of VAS scores in the four factors between the three groups (p = 0.063, p = 0.585, p = 0.155, and p = 0.533 for patient's age, interval between the trauma and final fixation, amount of injury, and ROM exercise, respectively) (Fig. 5).
This study examined the current consensus on treating displaced supracondylar fractures of the humerus in children. Orthopedic surgeons were found to accept closed reduction and percutaneous pinning as the initial treatment for a displaced supracondylar fracture of the humerus in children, even though there were some differences in the choice of pinning techniques. Most of the orthopedic surgeons used a removable splint during the ROM exercise period, and did not prescribe non-steroidal anti-inflammatory drugs (NSAIDs) routinely. Pediatric orthopedic surgeons tend to remove the pins and begin elbow movement earlier than hand surgeons and general orthopedic surgeons tended to be more concerned about elbow stiffness after supracondylar fracture than pediatric orthopedic surgeons, and favored gentle passive ROM exercise as elbow motion. Pediatric orthopedic surgeons most frequently adopted active ROM exercise as the elbow motion method. Pediatric orthopedic surgeons and general orthopedic surgeons acknowledged that the patient's age was the most contributing factor to the restoration of elbow motion, whereas hand surgeons acknowledged the amount of injury to be the most contributing factor.
This study has some limitations. First, the overall orthopedic surgeons perspectives were not provided because the majority of participants were hand surgeons and the overall orthopedic surgeons' results would be similar. Second, the questionnaire designed for this study was not validated. However, the authors could reduce the possible bias by interviewing the orthopedic surgeons directly. Third, majority of the supracondylar fracture of the humerus in children are treated by pediatric orthopedic surgeons and hand surgeons in our country. Therefore, the study results may not be applicable to other countries with different clinical situation.
General orthopedic surgeon tended to favor lateral entry more than the pediatric orthopedic surgeons and hand surgeons in terms of pin entry. Combining pin entry and pin number, hand surgeons preferred the more stable pinning technique using 3 crossed pins, whereas pediatric orthopedic surgeons and general orthopedic surgeons appeared to prefer a safer pinning technique using 2 lateral pins. It was reported that crossed pinning was biomechanically more stable but carried a higher risk of iatrogenic ulnar nerve palsy than the lateral pinning technique.9,14) Even though 3 lateral pins was reported in a previous study,15) none of the participants preferred the method in our study. The choice of pinning technique is still inconclusive and controversial, and requires further investigation.
A previous study reported that physical therapy (passive and active ROM exercise) after an open reduction and internal fixation could accelerate the restoration of elbow ROM but could not affect the final ROM at postoperative 1 year.11) Only 12% of the orthopedic surgeons referred the pediatric patients to physical therapists following supracondylar fractures of the humerus in our study. Pediatric orthopedic surgeons answered most frequently that the effect of gentle passive ROM exercise was harmful, followed by uncertain, somewhat effective, and totally effective. Hand surgeons and general orthopedic surgeons answered most frequently that the effect of gentle passive ROM exercise was uncertain, followed by somewhat effective. However, to our knowledge, there is little evidence regarding the effect of physical therapy after a closed reduction and pinning of a supracondylar fracture of the humerus in children.
This study sheds light on the current consensus and different perspectives on displaced supracondylar fractures of the humerus in children according to the different subspecialties of orthopedic surgeons. Elbow stiffness and other complications, such as, fixation loss and iatrogenic nerve palsy, could be problematic following operative treatment of displaced supracondylar humeral fractures in children, and often cause medicolegal issues particularly when there are insufficient published evidences. In such cases, taking consensus among physicians could protect themselves from the unnecessary legal issues. We believe that the results of this study could provide useful information in that point of view. However, more evidences and communication will be needed to reach a better consensus between the different subspecialties of orthopedic surgeons at the same time through further investigation.
Figures and Tables
Fig. 2
Preferred methods of range of motion (ROM) exercise after supracondylar fracture of the humerus in children.

Fig. 3
Orthopedic surgeons' perception on the effect of range of motion exercise after supracondylar fracture of the humerus in children.

References
1. Beaty JH, Kasser JR, Skaggs DL, Flynn JM, Waters PM. Rockwood and Wilkins' fractures in children. 2007. 7th ed. Philadelphia: Lippincott Williams & Wilkins.
2. Farley FA, Patel P, Craig CL, et al. Pediatric supracondylar humerus fractures: treatment by type of orthopedic surgeon. J Child Orthop. 2008. 2(2):91–95.

3. Zamzam MM, Bakarman KA. Treatment of displaced supracondylar humeral fractures among children: crossed versus lateral pinning. Injury. 2009. 40(6):625–630.

4. Zionts LE, Woodson CJ, Manjra N, Zalavras C. Time of return of elbow motion after percutaneous pinning of pediatric supracondylar humerus fractures. Clin Orthop Relat Res. 2009. 467(8):2007–2010.

5. Iobst CA, Spurdle C, King WF, Lopez M. Percutaneous pinning of pediatric supracondylar humerus fractures with the semisterile technique: the Miami experience. J Pediatr Orthop. 2007. 27(1):17–22.

6. Ponce BA, Hedequist DJ, Zurakowski D, Atkinson CC, Waters PM. Complications and timing of follow-up after closed reduction and percutaneous pinning of supracondylar humerus fractures: follow-up after percutaneous pinning of supracondylar humerus fractures. J Pediatr Orthop. 2004. 24(6):610–614.

7. Flynn JM, Sarwark JF, Waters PM, Bae DS, Lemke LP. The surgical management of pediatric fractures of the upper extremity. Instr Course Lect. 2003. 52:635–645.
8. Nacht JL, Ecker ML, Chung SM, Lotke PA, Das M. Supracondylar fractures of the humerus in children treated by closed reduction and percutaneous pinning. Clin Orthop Relat Res. 1983. (177):203–209.

9. Brauer CA, Lee BM, Bae DS, Waters PM, Kocher MS. A systematic review of medial and lateral entry pinning versus lateral entry pinning for supracondylar fractures of the humerus. J Pediatr Orthop. 2007. 27(2):181–186.

10. Murtezani A, Pustina A, Bytyci C, Hundozi H. Rehabilitation of children after elbow injuries. Niger J Med. 2007. 16(2):138–142.

11. Keppler P, Salem K, Schwarting B, Kinzl L. The effectiveness of physiotherapy after operative treatment of supracondylar humeral fractures in children. J Pediatr Orthop. 2005. 25(3):314–316.

12. Reitman RD, Waters P, Millis M. Open reduction and internal fixation for supracondylar humerus fractures in children. J Pediatr Orthop. 2001. 21(2):157–161.

13. Otsuka NY, Kasser JR. Supracondylar fractures of the humerus in children. J Am Acad Orthop Surg. 1997. 5(1):19–26.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download