Abstract
Background
Symphalangism is a rare congenital difference characterized by ankylosis of interphalangeal (IP) joints of the fingers and toes. In adults, there were several attempts to restore the stiff joints into mobile ones, but these treatment options resulted in poor outcomes and could not be applied to growing children. Here, we report our experiences on surgical treatment for children who had symphalangism of the hand.
Methods
We treated 36 joints in 17 children with symphalangism of the hand using dorsal capsulotomy and collateral ligament release. The diagnoses were based on history, physical examination, and simple radiographs. Affected fingers were classified according to our grading system. Simple compressive dressing was applied using Coban after surgery. Passive range of motion (ROM) exercise was started on day one or 2 postoperative, with the help of a hand therapist and patients' parents. The patients were prescribed passive ROM exercises for at least 2 hours a day over a period of 6 months.
Results
A single surgeon operated on 30 proximal IP joints, 3 distal IP joints, and 3 IP joints of the thumb. Twenty six joints were classified as grade I, and 10 as grade II. The ROM of affected joints, which was 7.8 ± 8.1 (mean ± SD) degrees preoperatively, increased to 46.8 ± 18.6 degrees at final follow-up. The final ROM was significantly better in grade I joints, especially when the children had operations at ages 24 months or younger.
Symphalangism is an uncommon condition characterized by fusion of the joints of the fingers or toes. There can be functional impairment in the grip and pinch actions of the affected hand, as well as unsightliness of the affected finger. The condition was first described by Harvey Cushing,1) who reported a family with hereditary fusion of the proximal interphalangeal (PIP) joints of the hand. The hallmark feature is longitudinal bony fusion across the joint. The PIP joint of the hand is the most common site of involvement. Symphalangism of the distal interphalangeal (DIP) joint can be seen in patients with symbrachydactyly. However, involvement of the metacarpophalangeal (MP) joint is extremely rare.2,3) Flatt and Wood3) classified symphalangism into 3 syndromes: true symphalangism in which involved digits have normal length; symbrachydactylism in which digits are short as well as stiff; and symphalangism with associated anomalies, such as Apert's syndrome or Poland's syndrome. The diagnosis is currently applied most oft en to congenital stiff ness of the finger joints with absence of transverse volar skin creases over those joints that are fused.3)
When complete fusion of the involved joint is observed in simple radiographs, there will be no dispute of diagnosis (Fig. 1D). When a child has a stiff finger with poorly discernible volar skin crease and showing a definite joint space of the involved joint in radiographs, there may be some confusion about diagnosis.
The symphalangeal joint may show definite joint space in radiographs when the child is very young, a volar skin crease may be absent or faint (Fig. 1B). This joint may have a very tight joint capsule and ligaments that show no active motion, with 10 to 20 degrees of passive motion of the affected joint. As the joint grows, fusion of the articular cartilage may develop and show definite joint space narrowing (Fig. 1C). Even at this stage, the affected joint may show a jerk of passive motion, because the cartilage mass is less stiff than bony mass. Later, the joint will develop into bony symphalangism (Fig. 1D). When the epiphyseal plate is not closed, there may be minor passive motion at the cartilaginous epiphyseal plate. Thus, the same joint can be classified as fibrous, cartilaginous, or bony symphalangism according to the child's age at diagnosis.
There have been several reports of surgical treatment to make symphalangeal joints into mobile ones, such as interposition arthroplasties with silicone cap,3) and silicone implant arthroplasties.4,5) The results of these operations were poor, and these types of operations were not applicable to growing children. Shaving of articular surfaces have failed and resulted in re-ankylosis.6)
The surgical outcome of pediatric symphalangeal joints, according to our classification system, is presented in this study.
This study was approved by the Institutional Review Board of Seoul National University Hospital. We explained the condition to the patients, the potential surgical outcomes, and potential disadvantages related to surgery. Informed consent was obtained from all parents prior to enrollment.
We treated 36 joints in 17 consecutive children that had symphalangism with dorsal capsulotomy and collateral ligament release all performed by a single surgeon (GHB). There were 7 boys and 10 girls with an average age at operation of 46.6 months (range, 15 to 113 months).
The diagnosis was made on the basis of history, physical examination, and simple radiographs. The patients showed congenitally stiff interphalangeal (IP) joint(s), without history of trauma. Volar skin crease of the affected joints was absent or hardly recognized. Bilateral simple radiographs of all fingers were taken to compare affected finger(s) with normal ones.
Affected fingers were classified according to our grading system (Table 1).
The inclusion criteria were: 1) symphalangism of IP joints without symbrachydactyly or associated anomalies, and 2) grade I or II. The exclusion criteria were: 1) symphalangism with symbrachydactyly or associated anomalies, 2) children whose parents did not agree with the operation, or 3) less than one year of postoperative follow-up.
After general anesthesia and pneumatic tourniquet application, a longitudinal or Z-plasty incision was made on the dorsum of the affected joint (Fig. 2). Extensor mechanism and joint capsule were identified (Fig. 3A) and dissected from subcutaneous tissue (Fig. 3B). A longitudinal incision was made on the midline of the extensor apparatus. The extensor tendon was carefully separated from underlying joint capsule and collateral ligaments. The dorsal half of the joint capsule was incised transversely, and then the dorsal half of both medial and lateral collateral ligaments were cut with a No. 11 blade (Fig. 3C). In grade I joints, gentle passive flexion of the affected joint can facilitate full flexion. In the alternative, more forceful passive flexion is needed in grade II joints. Sometimes release of the proximal part of volar plate is necessary when passive flexion is not enough. Split extensor apparatus was sutured with 5-0 Prolene, and the skin was sutured with 6-0 Nylon (Fig. 4). After surgery, a simple dressing using Coban was applied. One to 2 days after the surgery, passive range of motion (ROM) exercise was started by hand therapists and parents. The stitches were removed 2 to 3 weeks after the surgery. Passive ROM exercises were recommended for more than 2 hours a day over 6 months.
The average duration of postoperative follow-up was 29.5 months (range, 12 to 81 months). All the children were followed up at postoperative one week, 2 weeks, one month, 2 months, 3 months, 6 months, and 12 months. Yearly follow-up was performed thereafter. The ROM of affected joints was measured by senior author (GHB) with use of a goniometer.
The paired t-test was used to analyze differences between initial and final degrees of ROM in affected joints. The Mann-Whitney U-test was used to compare the postoperative ROM of 2 groups - one group whose age at the time of operation was less than 24 months, and the other group whose age was more than 24 months. The same test was used to compare the postoperative ROM between the grade I and grade II joints. Repeated measure analysis of variances followed by Bonferroni analysis used to determine the significance of change in the degree of ROM of the joint after the surgery. Statistical analysis was performed using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA). A p-value of < 0.05 was considered statistically significant.
None of the 17 children had a history of symphalangism. Sixteen joints were involved in right hand, and 20 joints in the left. The number of affected fingers were 3 (8.3%) in the thumb, 6 (16.7%) in index finger, 7 (19.4%) in the long finger, 7 (19.4%) in the ring finger, and 13 (36.1%) in the little finger. The affected joints were 30 at the PIP joints (83.3%), 3 at the DIP joints (8.3%), and 3 at the thumb IP joints (8.3%).
Patient details are described in Table 2. Twenty six joints in 13 children were classified as grade I, and 10 in 6 children grade II. Fifteen joints in 5 children were categorized as group 1 in that the age at the time of operation was less than 24 months. Twenty one joints in 12 children were categorized as group 2 in that the age at the time of operation was more than 24 months.
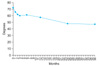
The ROM of affected joint was 9.9 ± 6.8 (mean ± SD) degrees preoperatively. This was increased to 46.8 ± 18.6 degrees at final follow-up (p < 0.001, paired t-test) (Fig. 5). In 26 grade I joints of 13 children, had passive motion preoperatively. The preoperative passive ROM of 5 joints was 5 degrees, 4 joints 10 degrees, 5 joints 15 degrees, 7 joints 20 degrees, respectively.
Repeated measures analysis of variances showed that there were significant differences over time among the mean ROM of affected joint (p = 0.042) (Fig. 6). Post hoc Bonferroni tests indicated that the mean ROM decreased significantly from 1 to 24 months after surgery (p < 0.05).
We compared the ROM of group 1 (those who had the operation at the age of less than 24 months) and group 2 (those who had the operation at the age of more than 24 months) by using the Mann-Whitney U-test. There was no difference in the preoperative ROM of the affected joint between the 2 groups (group 1, 12.0 ± 4.5 degrees; group 2, 8.3 ± 6.9 degrees; p = 0.260). However, the final ROM of affected joint after surgery was better in group 1 than in group 2 (group 1, 56.3 ± 10.4; group 2, 40.0 ± 20.3; p = 0.011).
In addition, we compared the ROM of affected joints between grade I and grade II. The ROM of grade I joints at last follow-up was significantly larger than those of grade II (grade I, 54.0 ± 11.4; grade II, 28.0 ± 21.0; p < 0.001). Three joints in 2 children were completely fused at 2 years and 3 years after the surgery (Fig. 7). Their ages at the time of surgery were 51 months and 91 months, respectively.
Symphalangism is congenital stiffness of the digits. Cushing published a paper introduced the term "symphalangism" to describe a family that had 84 involved members.1) The largest pedigree in the genetic literature is the Talbot family.7) Thus, the term symphalangism was initially used to describe an autosomal dominant disorder affecting PIP joints of the fingers.1,8-10) However, many authors included congenitally stiff DIP and MP joints with symphalangism. Drug-induced symphlangism, such as thalidomide, was also reported. The non-hereditary symphalangism, often seen with symbrachydactyly, are reported as sporadic.2) In our series, grade I symphalangism was 72.2%, which no included with symphalangism previously. In addition, there may be a racial difference in inheritance. Thus, there was no typical hereditary symphalangism in our series. Grade II cartilaginous symphalangism may develop into grade III bony symphalangism as the affected children grow, because cartilaginous portions will eventually be ossified. Grade I fibrous symphalangism, however, may not always develop into grades II and III. Some of grade I symphalangism may remain as stiff , but have little motion. Certain types of grade I had as much as 20 degrees of passive motion, preoperatively. We do not know the natural history of these cases. These conditions may not be true symphalangism, and may be considered incomplete symphalangism. We found slit-like joint space in grade I symphalangism during the operation. When we performed dorsal capsulotomy and collateral ligaments release, the joint was easily flexed passively (Fig. 4). In grade II symphalangism, we found only cartilaginous mass without any joint space in the affected joint. Cautious shaving of cartilaginous mass was performed to make phalangeal head and base of adjacent phalanges. Gentle gradual passive flexion of the joint was tried. Surgical outcome of these grade II fingers was worse than that of grade I, however, we could obtain reasonable ROM when the operations were done before two years of age.
Most cases of symphalangism are related with mutations of the NOG gene or noggin gene.11,12) Recently, mutations in another protein, growth and differentiation factor 5 (GDF 5) have also been associated with symphalangism.13)
Magnetic resonance images (MRI) were taken in early series of children to evaluate the joint status. However, the MRIs were not clear enough to evaluate the small IP joints of small children. More advanced MRI with high resolution power may be helpful to diagnose the grading of symphlangism in the near future.
Many surgical treatments to achieve the functional motion of stiff joint were performed.3-5,14) However, surgical mobilization has been reported to yield unsatisfactory functional results.2,5) A vascularized toe joint transfer to 4th PIP joint was performed in 6-year-old children and a reasonable range of motion was achieved at 4 years and one month follow-up,6) however there has not been a follow-up report.
Upton2) suggested early release may be worthwhile, when a symphalangeal joint of the finger showed an apparent "joint space" on plain radiography. Although Upton did not mention his own clinical case, his description might be our grade I condition. Our surgical technique was targeting soft tissue release, dorsal capsulotomy, and incision of the dorsal half of both collateral ligaments. The functional motion after surgery was good. However, we could find the ROM of affected joint decreased over the course of 2 years after surgery, although the slope was very slow (Fig. 6). The ROM was maintained, thereafter. Long-term follow-up until skeletal maturity will answer the final results.
The age of the children at the time of surgery is very important. Upton2) suggested soft tissue release was useful in children younger than 2 or 3 years. We think that the earlier the operation is performed, the better the results.
In conclusions, dorsal capsulotomy and release of the dorsal half of collateral ligaments of affected joints can make symphalangeal joints into mobile ones in grade I and II symphalangism of interphalangeal joints of the hand. A long-term follow-up study is very necessary to evaluate the consequences of this operation.
Figures and Tables
Fig. 1
Grade of symphalangism in simple radiographs. (A) Normal joint. (B) Grade I: fibrous symphalangism - mild joint space narrowing in distal interphalangeal joint. (C) Grade II: cartilaginous symphalangism - only slit of joint space is observed. (D) Grade III: bony symphalangism.
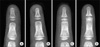
Fig. 2
Skin incision. (A) Longitudinal incision was preferred when the dorsal skin was sufficient. (B) Z-plasty incision was done when the dorsal skin of the affected joint was tight.

Fig. 3
Operative procedures. (A) After skin incision, extensor apparatus was exposed. (B) Extensor apparatus and joint capsule were separated from subcutaneous tissue. (C) Dorsal capsulotomy followed by release of dorsal half of both collateral ligaments were performed with a No. 11 blade, after longitudinal incision of extensor apparatus.

Fig. 4
Intraoperative passive motion before (A, C) and after (B, D) surgical release. (A, B) Full range of passive flexion were observed in 4th proximal interphalangeal (PIP) joint, and (C, D) 5th PIP joint.

Fig. 5
(A, B) There was no motion at proximal interphalangeal joint preoperatively. (C, D) The child had an operation at 17 months of age. Good range of motion was maintained at postoperative 34 months.

References
1. Cushing H. Hereditary anchylosis of the proximal phalangeal joints (symphalangism). Genetics. 1916. 1(1):90–106.

2. Upton J. Mathes SJ, editor. Failure of differentiation and overgrowth. Plastic surgery. 2005. 2nd ed. Philadelphia: Saunders Elsevier;265–322.
4. Palmieri TJ. The use of silicone rubber implant arthroplasty in treatment of true symphalangism. J Hand Surg Am. 1980. 5(3):242–244.

5. Dobyns J. Green DP, Hotchkiss RN, Pederson WC, editors. Symphalangism. Green's operative hand surgery. 1999. 4th ed. New York: Churchill Livingstone;470–473.
6. Shibata M. Gupta A, Kay SP, Scheker LR, editors. Symphalangism. The growing hand. 2000. 1st ed. London: Mosby;289–292.
7. Elkington SG, Huntsman RG. The Talbot fingers: a study in symphalangism. Br Med J. 1967. 1(5537):407–411.

8. Strasburger AK, Hawkins MR, Eldridge R, Hargrave RL, McKusick VA. Symphalangism: genetic and clinical aspects. Bull Johns Hopkins Hosp. 1965. 117:108–127.
9. Castle JE, Bass S, Kanat IO. Hereditary symphalangism with associated tarsal synostosis and hypophalangism. J Am Podiatr Med Assoc. 1993. 83(1):1–9.

10. Gaal SA, Doyle JR, Larsen IJ. Symphalangism in Hawaii: a study of three distinct ethnic pedigrees. J Hand Surg Am. 1988. 13(5):783–787.

11. Polymeropoulos MH, Poush J, Rubenstein JR, Francomano CA. Localization of the gene (SYM1) for proximal symphalangism to human chromosome 17q21-q22. Genomics. 1995. 27(2):225–229.

12. Takahashi T, Takahashi I, Komatsu M, et al. Mutations of the NOG gene in individuals with proximal symphalangism and multiple synostosis syndrome. Clin Genet. 2001. 60(6):447–451.

13. Seemann P, Schwappacher R, Kjaer KW, et al. Activating and deactivating mutations in the receptor interaction site of GDF5 cause symphalangism or brachydactyly type A2. J Clin Invest. 2005. 115(9):2373–2381.

14. Upton J, Sohn SA, Glowacki J. Neocartilage derived from transplanted perichondrium: what is it? Plast Reconstr Surg. 1981. 68(2):166–174.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download