Abstract
Background
Minocycline-induced pigmentation of bone (black bone) is well described in tooth-bearing intra-oral bone, but is less known in periarticular bone in patients who have undergone total joint arthroplasty. On a retrospective basis, we investigated the short-term clinico-radiological results of total joint arthroplasties in which the patient developed minocycline-induced periarticular black bone.
Methods
We found 5 cases (0.08%), in 4 patients, of periarticular bone pigmentation revealed during total joint arthroplasties (2 hips, 2 knees, and 1 ankle) in our series of total joint surgeries (6,548 cases) over a 10-year time period in our 3 institutes. Their mean age was 56 years at surgery. All patients had received long-term minocycline treatment. Mean dosage and duration of minocycline was 160 mg/day and 2.2 years, respectively. Minocycline had been prescribed for reactive arthritis (one), rheumatoid arthritis (two) and late infection after total joint arthroplasty (two patients). Mean follow-up period was 3.4 years after the surgeries.
Results
All cases had black or brown pigmentation in the periarticular bones during the surgery. There was no pigmentation in the cartilage or soft tissues of the joints. The mean Japanese Orthopaedic Association (JOA) score or Japanese Society for Surgery of the Foot (JSSF) scale for rheumatoid arthritis foot and ankle joints at latest follow-up (case 1, 66; case 2, 87; case 3, 77; case 4, 77; case 5, 80) improved compared to those of pre-surgery (case 1, 47; case 2, 45; case 3, 55; case 4, 34; case 5, 55). No implant loosening was noted on radiographic examination during the follow-up period. No abnormal bone formation, bone necrosis, hemosiderin deposition, malignancy or metallic debris was found on histological examination.
Conclusions
No clinico-radiological symptoms of total joint arthroplasties showed in the patients with minocycline-induced periariticular black bone in the short-term. Systemic minocycline treatment has the potential to induce significant black pigmentation of many tissues. In particular, minocycline-induced pigmentation of periarticular bone may be accelerated by inflammation due to rheumatic or pyogenic arthritis. Surgeons should recognize the risk of bone pigmentation in inflamed joints due to the systemic treatment of minocycline and explore its influence on periarticular bone and total joint arthroplasty in the long-term.
Minocycline, 7-dimethylamino-6-demethyl-6-deoxytetracycline, a semi-synthetic broad-spectrum tetracycline antimicrobial agent, has been used since 1967.1) Because minocycline has distinct advantages over other tetracyclines because of its high lipid solubility, better absorption, minimal phototoxicity, and superior antimicrobial activity,1-4) minocycline has been used extensively in the treatment of acne rosacea, acne vulgaris, chronic respiratory diseases, and Gram-positive or -negative infections. Minocycline binds to the 30S subunits of bacterial ribosomes and specifically inhibits the binding of aminoacyl-tRNA to the ribosomal acceptor site, in this way inhibiting protein synthesis in susceptible microorganisms.5,6) In addition, this drug is used in the treatment of rheumatoid arthritis because of its potent anti-inflammatory properties.5,7) Although long-term minocycline therapy is safe for most patients, the most frequently reported adverse reaction is cutaneous pigmentation.8) Pigmentation caused by minocycline has been reported not only in the skin, but in other soft tissues including the thyroid gland, mucosa, and eyes;5,9-11) in the breast milk secretions,2) and in hard tissues, including teeth, nails and bones.2-5,8,10)
Over twenty published reports have described bone pigmentation and/or discoloration induced by minocycline in the oral cavity, variously calling it intra-oral "black bone" with "black or green roots" of the teeth.2,6) However, to our knowledge, there have been only 6 previous reports regarding minocycline-induced bone pigmentation that is not in the oral cavity. These have included one case of affected parietal bone and costal cartilage found at autopsy,10) one of the clavicle discovered during surgery to treat a bone cyst,12) one of the acromion during surgery for subacromial impingement,3) one of the thoracic vertebrae during surgery for sever lumbago,13) one of the ends of the femur and tibia at total knee arthroplasty (TKA) for osteoarthritis,14) and one of the diaphysis of the femur at revision surgery for late infection after primary surgical reduction of a fracture.4) In particular, only one case of periarticular bone pigmentation observed at the surgical site during total join arthroplasty has been reported and that follow-up period was one year after surgery.14) Although it is still unclear whether minocycline-induced pigmentation of periarticular bones have an effect on the clinical and/or radiological result of their total joint arthroplasties, minocycline, which is a semi-synthetic tetracycline, is known to cause dysosteogenesis of oral bone, in particular in children.2,6) They are expected to have a potent of effect to the bone around total joint arthroplasty like a effect for oral bone in children.
In this retrospective study on data from a 10-year period, we investigated minocycline-induced periarticular black bone and the short-term clinico-radiological results in our patients who had undergone total joint arthroplasty.
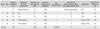
We investigated in our series of total joint arthroplasty (total 6,548 cases) patients of 10 years (2001-2010) that had been treated at one of our 3 institutions and found 5 cases (0.08%), in 4 patients, of minocycline-induced pigmentation of periarticular bone observed at the surgical site during one of the following surgeries summarized in Table 1: one total ankle arthroplasty (TAA; Fine total ankle, Nakashima, Okayama, Japan), one primary total hip arthroplasty (THA; ZCA cup, CPT Stem, Zimmer, Warsaw, IN, USA), one revision THA (KT-plate, JMM, Kyoto, Japan; ZCA cup, CPT Stem, Zimmer), one TKA (Vanguard, Biomet, Warsaw, IN, USA), and one revision TKA (NexGen LCCK, Zimmer). The primary disease was reactive arthritis (case 1), rheumatoid arthritis (RA, cases 2 and 3), sarcoidosis (case 4) and osteoarthritis (case 5). Minocycline had been prescribed for reactive arthritis (case 1), RA (cases 2 and 3) and late infection after total joint arthroplasty (cases 4 and 5). In case 1, the patient was prescribed low dose prednisolone combined with minocycline for reactive arthritis; in cases 2 and 3 in patients using combination therapy with methotrexate, salazosulfapyridine and prednisolone with minocycline for RA; in case 4, the patient was prescribed a moderate dose of prednisolone for his sarcoidosis.
For clinical estimation, the Japanese Orthopaedic Association (JOA) hip15) and knee16) scores, and Japanese Society for Surgery of the Foot (JSSF) scale for RA foot and ankle joints17) were analyzed at the preoperation and at latest follow-up. X-rays were estimated for radiological assessments at the preoperation and latest follow-up by two observers blindly. In addition, skin pigmentation by minocycline was investigated in each case. The mean follow-up period was 3.4 years (range, 2.0 to 4.6 years). We did not perform a statistical analysis because the numbers were very small in each category.
All cases were observed to have black or brown pigmentation in the periarticular anatomy during total joint arthroplasty. We show a representative example (case 1) who was affected on her right ankle by reactive arthritis, which included black pigmentation of the periarticular bone (Fig. 1A and 1C). No pigmentation was found in any other tissue, cartilage or soft tissues, such as the synovial tissue in the joint.
Radiographic examination showed no implant loosening and abnormal findings during the postoperative follow-up in all cases. We show the representative X-ray at the pre-surgery and the latest follow-up (case 1) (Fig. 1A and 1B).
All JOA scores, or JSSF scale scores, in each case at the last follow-up were compared to those of the pre-surgery. In case 1, the patient was able to walk, but was experiencing slight arthritic joint pain because of the arthritis in her ankle at the most recent follow-up. In cases 2, 3, and 4, they were able to walk and undertake daily activities with no hip or knee pain. In case 5, his JOA score was used for to estimate the necessity to be confinement to bed, because unfortunately the patient developed severe multiple cerebral infarctions and aspiration pneumonia, 24 months after the revision surgery.
Histological examination of the removed tissue at the operation revealed no bone necrosis, hemosiderin, malignancy, or other specific changes. No abnormal bone formation, bone necrosis, hemosiderin deposition, malignancy or metallic debris, were found on histological examination in all cases (Fig. 1D).
In this retrospective study, we presented the short-term clinico-radiological results of total joint arthroplasties in 5 cases, in which the patients had minocycline-induced periarticular black bone at the surgical site.
It is well known that periarticular bone pigmentation or discoloration in joints are caused by several pathological factors, including ochronosis,18) hemophilic arthropathy,19) pigmented villonodular synovitis,20) metallosis after joint arthroplasty,21) and rarely drugs, such as tetracycline antibiotics.6) Ochronosis, which is a result of deposition of black homogentisic acid in the bone, cartilage and synovial membrane of joints is most often associated with alkaptonuria, a recessive hereditary disease caused by a complete defect of homogentisic acid oxidase.18) In hemophilic arthropathy and pigmented villonodular synovitis, hemosiderin deposition causes brownish discoloration, the hemosiderin being derived from phagocytosis of red blood cells after joint hematomas caused by intra-articular bleeding.19,20) In metallosis, micro metallic abrasion after joint arthroplasty causes black discoloration of the bone surface, synovium, and articular cartilage in the joints.21) In fact, metallosis after joint arthroplasty dose not show pigmentation of internal bone, but only discoloration/pigmentation of bone surface and soft tissue in the joint, except occult massive osteolysis in acetabulum where titanium debris was carried into the cancellous structure, and remodeling of bone occur involving the small metal particle into the bone matrix.22,23) Tetracycline antibiotics were first found to cause intra-oral bone pigmentation and discoloration of teeth in the 1950s.6)
In 1979, Ragucci24) suggested the possibility that minocycline-caused pigmentation in alveolar bone. Fredrich and Brookes25) reported minocycline-induced black pigmentation of alveolar bone in 1984. Over 20 published reports have described pigmentation and discoloration induced by minocycline in intra-oral bone.2,6,7,24-26) However, to our knowledge, only 6 previous articles have reported minocycline-induced pigmentation of bone outside the oral cavity.3,4,10,12-14) In particular, only one case of periarticular bone pigmentation observed during total joint arthroplasty has previously been reported; in this case, black or green pigmentation was found in the distal end of the femur and proximal end of the tibia during TKA for osteoarthritis (Table 3)14).
Black pigmentation of bone by minocycline is thought to occur through ferric iron being bound to the oxidized drug in developing bone, and via the accumulation of insoluble quinine from degradation of the aromatic ring of the drug in mature bone.1,7,27) However, deposition of iron and/or hemosiderin has not been observed in all cases. In the present study, common histological examination of the removed tissue at the surgery revealed no evidence of bone necrosis, hemosiderin, malignancy, or other specific changes, but some authors have elicited fluorescence, indicating the presence of minocycline-stained bone, by ultraviolet microscopy.3,26) One author has reported pigmentation of cartilage,10) however no discoloration of cartilage or soft tissue in the joints was observed in our cases. The mechanism of black bone pigmentation is not yet completely understood.3,7,14)
Minocycline-induced pigmentation in skin is considered to be dose-dependent, the reported incidence being 2% in patients taking the drug over 2 months, 10% over one year, and 20% over 2 years.2,26) In addition, the incidence of skin pigmentation in patients treated for rheumatoid arthritis (range, 40% to 70%) is reportedly higher than that in patients treated for acne (range, 0.4% to 15%).7,28) In our 5 cases, the bone pigmentation was seen during surgery on joints where there was active inflammation due to rheumatic or pyogenic arthritis. This suggests that pigmentation of bone is influenced by inflammation in joints, such inflammation possibly accelerating the oxidization of minocycline, the process that is believed to cause skin pigmentation.1,7,27) In addition, in 4 of our cases (80%) skin pigmentation had been observed for a mean duration of 13 months (range, 2 to 22 months) after receiving minocycline. In previous reports regarding minocycline-induced pigmentation of bone outside the oral cavity, associated skin pigmentation was observed in 5 of the cases (83%). The occurrence of skin pigmentation might be strongly correlated with that of bone pigmentation. If so, it would allow prediction of bone pigmentation prior to surgery.
On the other hand, the time to resolution of black pigmentation and/or discoloration of bone after discontinuation of the drug is unknown. Most reported cases of minocycline/tetracycline-induced black pigmentation or discoloration of intra-oral bone have failed to resolve.6,7,26) In an animal model, Bowels29) demonstrated that an antioxidant, such as ascorbic acid (vitamin C), can inhibit minocycline-induced pigment deposition.
To our knowledge, there have been no reports describing the prevalence of minocycline induced-black bone and its potential adverse events with/without any implants in the long-term. McCleskey and Littleton14) reported good physiological and radiographic results of TKA one year after surgery for osteoarthritis in a patient who had taken minocycline for 2 years to treat acne rosacea. With the exception of case 5, who had severe multiple cerebral infarctions and aspiration pneumonia after his surgery, our 4 cases had satisfactory results from total joint arthroplasty, their clinical results (JSSF scale and JOA score) being improved and their implants being stable on radiographic examination at the most recent follow-up. However, our study population is extremely small (5 cases) and the mean duration of postoperative follow-up was only 3.4 years (range, 2.0 to 4.6 years). The large cases are needed with paired-matched control group for a long duration and statistical analysis in the next study. In addition, tetracycline is contraindicated in children because it causes dysosteogenesis and enamel hypoplasia; these adverse events occur with minocycline, which is a semi-synthetic tetracycline.2,6,26) It is speculated minocycline has potent influence on the clinical and/or radiological result of the bone around total joint arthroplasty. The adverse effects of minocycline-induced bone pigmentation and/or discoloration in regard to loosening of implants should be carefully assessed in the long term and patients informed of this adverse effect of minocycline before they receive the drug, because the influence of minocycline on bone quality and bone metabolism in vivo is still unknown in long term. We believe that not only rheumatologists, but orthopedic surgeons should know about black bone and minocycline-induced bone discoloration/pigmentation in the joint. It would be possible that surgeons may encounter metallic debris deposition combined with minocycline-induced bone discoloration/pigmentation, struggle to determine the degree to which the area should be removed during revision surgery.
In conclusion, we have presented the short-term results of total joint surgeries in 5 cases that had minocycline-induced black pigmentation of the periarticular bone. In cases with minocycline-induced bone pigmentation, surgeons should examine carefully for implant loosening and adverse effects of bone quality around implants in the long term.
Figures and Tables
Fig. 1
Case 1: A 75-year-old woman had received 200 mg/day minocycline for 2 years to treat reactive arthritis. (A) Anteroposterior radiographic views of the right ankle preoperatively and (B) at the last follow-up. Preoperatively, her right ankle shows end-stage osteoarthritic changes. (C) Black pigmentation and discoloration of the distal part of the tibia and talus (indicated by arrows) were observed during total ankle arthroplasty; this was due to long-term minocycline medication. (D) Hematoxylin-eosin-stained microphotograph of the black bone removed from the distal end of the tibia shows normal bone structure; there were no bone necrosis, deposition of hemosiderin, malignancy, or abnormalities of bone matrix (×200).

Fig. 2
Case 4: A 33-year-old man had received 200 mg/day minocycline for 7 months for infection of his total hip arthroplasty. Photographic views of minocycline-induced skin hyperpigmentation on the lower legs (A) at pre-revision surgery and (B) 37 months after discontinuing minocycline. Note the resolution of skin pigmentation after discontinuation of minocycline.

ACKNOWLEDGEMENTS
We sincerely thank a lot Ms. Eiko Saito and Dr. Taku Nakajima for their skilful technical support in histological analysis and clinical data gathering. Yuya Takakubo was supported by the Excellent Young Researchers Overseas Visit Program, the Japan Society for the Promotion of Science (21-8117).
References
1. Kelly RG, Kanegis LA. Metabolism and tissue distribution of radioisotopically labelled minocycline. Toxicol Appl Pharmacol. 1967. 11(1):171–183.
2. Eisen D, Hakim MD. Minocycline-induced pigmentation. Incidence, prevention and management. Drug Saf. 1998. 18(6):431–440.
3. Pandit S, Hadden W. Black pigmentation of bone due to long-term minocycline use. Surgeon. 2004. 2(4):236–237.
4. Hepburn MJ, Dooley DP, Hayda RA. Minocycline-induced black bone disease. Orthopedics. 2005. 28(5):501–502.

5. Treister NS, Magalnick D, Woo SB. Oral mucosal pigmentation secondary to minocycline therapy: report of two cases and a review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004. 97(6):718–725.

6. Sanchez AR, Rogers RS 3rd, Sheridan PJ. Tetracycline and other tetracycline-derivative staining of the teeth and oral cavity. Int J Dermatol. 2004. 43(10):709–715.

7. LaPorta VN, Nikitakis NG, Sindler AJ, Reynolds MA. Minocycline-associated intra-oral soft-tissue pigmentation: clinicopathologic correlations and review. J Clin Periodontol. 2005. 32(2):119–122.

8. Angeloni VL, Salasche SJ, Ortiz R. Nail, skin, and scleral pigmentation induced by minocycline. Cutis. 1987. 40(3):229–233.

9. Benitz KF, Roberts GK, Yusa A. Morphologic effects of minocycline in laboratory animals. Toxicol Appl Pharmacol. 1967. 11(1):150–170.

10. Attwood HD, Dennett X. A black thyroid and minocycline treatment. Br Med J. 1976. 2(6044):1109–1110.
11. Sabroe RA, Archer CB, Harlow D, Bradfield JW, Peachey RD. Minocycline-induced discolouration of the sclerae. Br J Dermatol. 1996. 135(2):314–316.
12. Wolfe ID, Reichmister J. Minocycline hyperpigmentation: skin, tooth, nail, and bone involvement. Cutis. 1984. 33(5):457–458.

13. Rumbak MJ, Pitcock JA, Palmieri GM, Robertson JT. Black bones following long-term minocycline treatment. Arch Pathol Lab Med. 1991. 115(9):939–941.

14. McCleskey PE, Littleton KH. Minocycline-induced blue-green discoloration of bone: a case report. J Bone Joint Surg Am. 2004. 86(1):146–148.

15. Ueno R. Staging of osteoarthritis of the hip joint according to the roentgenographic findings. J Jpn Orthop Assoc. 1971. 45(10):826–828.

16. Koshino T. Japanese Orthopaedic Association knee scoring system. J Jpn Orthop Assoc. 1988. 62(8):900–902.

17. Niki H, Aoki H, Inokuchi S, et al. Development and reliability of a standard rating system for outcome measurement of foot and ankle disorders II: interclinician and intraclinician reliability and validity of the newly established standard rating scales and Japanese Orthopaedic Association rating scale. J Orthop Sci. 2005. 10(5):466–474.

18. Takagi M, Ida H, Kobayashi S, Ishii M, Osanai T, Konttinen YT. Ochronotic spondylarthropathy: two case reports of progressive destructive changes in the hip. Mod Rhumatol. 2003. 13(1):81–86.
19. Kelley SS, Lachiewicz PF, Gilbert MS, Bolander ME, Jankiewicz JJ. Hip arthroplasty in hemophilic arthropathy. J Bone Joint Surg Am. 1995. 77(6):828–834.
20. Goldman AB, DiCarlo EF. Pigmented villonodular synovitis: diagnosis and differential diagnosis. Radiol Clin North Am. 1988. 26(6):1327–1347.

21. Iida H, Kaneda E, Takada H, Uchida K, Kawanabe K, Nakamura T. Metallosis due to impingement between the socket and the femoral neck in a metal-on-metal bearing total hip prosthesis: a case report. J Bone Joint Surg Am. 1999. 81(3):400–403.

22. Khan RJ, Wimhurst J, Foroughi S, Toms A. The natural history of metallosis from catastrophic failure of a polyethylene liner in a total hip. J Arthroplasty. 2009. 24(7):1144.e1–1144.e4.

23. Huber M, Reinisch G, Zenz P, Zweymuller K, Lintner F. Postmortem study of femoral osteolysis associated with metal-on-metal articulation in total hip replacement: an analysis of nine cases. J Bone Joint Surg Am. 2010. 92(8):1720–1731.

25. Fendrich P, Brooke RI. An unusual case of oral pigmentation. Oral Surg Oral Med Oral Pathol. 1984. 58(3):288–289.

26. Westbury LW, Najera A. Minocycline-induced intraoral pharmacogenic pigmentation: case reports and review of the literature. J Periodontol. 1997. 68(1):84–91.
27. Cockings JM, Savage NW. Minocycline and oral pigmentation. Aust Dent J. 1998. 43(1):14–16.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download