Abstract
Background and Purpose
Methods
Results
Figures and Tables
Fig. 1
Numbers of eligible study patients in the TIMS-China registry. AP: antiplatelet, ICH: intracerebral hemorrhage, NIHSS: National Institutes of Health Stroke Scale, rt-PA: recombinant tissue plasminogen activator, sICH: symptomatic ICH, TIMS-China: Thrombolysis Implementation and Monitor of Acute Ischemic Stroke in China.

Fig. 2
Comparison of function in different types of THEPI in the AP group at the 7- and 90-day follow-ups in patients from TIMS-China. AP: antiplatelet, ICH: intracerebral hemorrhage, mRS: modified Rankin Scale, THEPI: thrombolytic-related hemorrhage without extensive parenchymal involvement, TIMS-China: Thrombolysis Implementation and Monitor of Acute Ischemic Stroke in China.

Fig. 3
Comparison of function in different types of THEPI in the AP-naïve group at the 7- and 90-day follow-ups in patients from TIMS-China. AP: antiplatelet, ICH: intracerebral hemorrhage, mRS: modified Rankin Scale, THEPI: thrombolytic-related hemorrhage without extensive parenchymal involvement, TIMS-China: Thrombolysis Implementation and Monitor of Acute Ischemic Stroke in China.
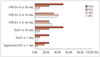
Table 1
Baseline characteristics of THEPI patients with (AP group) and without (AP-naïve group) AP therapy

The data are mean±SD or n (%) values.
AP: antiplatelet, ICA: internal carotid artery, MCA: middle cerebral artery, rt-PA: recombinant tissue plasminogen activator, THEPI: thrombolytic-related hemorrhage without extensive parenchymal involvement, TIA: transient ischemic attack, TOAST: Trial of Org 10172 in Acute Stroke Treatment.
Table 2
Functional outcomes for THEPI with and without postthrombolysis AP therapy

Adjusted covariates (logistic regression model): age, sex, baseline NIHSS score, and dose of rt-PA.
AP: antiplatelet, CI: confidence interval, NIHSS: National Institutes of Health Stroke Scale, OR: odds ratio, rt-PA: recombinant tissue plasminogen activator, THEPI: thrombolytic-related hemorrhage without extensive parenchymal involvement.
Table 3
Functional outcomes for THEPI subgroups (HT1+HT2+PH1) with and without AP therapy after thrombolysis

Except where stated otherwise, data are n (%) values. Adjusted covariates (logistic regression model): age, sex, baseline NIHSS score, and dose of rt-PA.
AP: antiplatelet, CI: confidence interval, NIHSS: National Institutes of Health Stroke Scale, OR: odds ratio, rt-PA: recombinant tissue plasminogen activator, THEPI: thrombolytic-related hemorrhage without extensive parenchymal involvement.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download