Abstract
Background
The assessment of the severity of psoriasis is often subjective because of the lack of quantitative laboratory diagnostic tools. Histopathological examination is the most commonly performed procedure for psoriasis diagnosis; however, it is usually descriptive. Thus, there is currently no quantitative method of determining psoriasis severity. The clinical types of psoriasis are correlated with the severity of the disease, and a lesional severity index, such as the psoriasis severity index (PSI), could be used as a quantitative tool for assessing gross severity.
Methods
Psoriatic lesions in 98 patients were evaluated. The lesions were classified into the guttate, papular, small plaque, and large plaque types according to morphology, and were scored according to the PSI. Ten common histopathological features of psoriasis were evaluated for correlation with gross severity.
Psoriasis is a common chronic inflammatory skin disorder that affects approximately 1%~2% of the Western population, and is characterized by variably sized, well-demarcated, dry plaques usually covered with layers of fine, silvery scales. Psoriatic lesions are classified into the guttate, plaque, pustular, and erythrodermic types according to clinical features, especially their size and distribution1.
Histopathological examination is the only method for confirming the diagnosis of psoriasis. Characteristic findings include uniform elongation of the rete ridges, dilated blood vessels, thinning of the suprapapillary plate, intermittent parakeratosis, perivascular infiltration of lymphocytes, and the presence of occasional neutrophil aggregates in the epidermis. The histopathological diagnosis is made by comprehensively evaluating these findings2. In most cases of inflammatory dermatoses, histopathological diagnoses were based on a qualitative decision, which means that the clinical diagnosis may be correct or incorrect. However, in some cases, the disease severity needs to be quantitatively assessed by investigating the correlation of histopathological findings with the clinical severity of the disease.
Dermatologists always focus on clinical severity assessment tools in diagnosing psoriasis. However, these tools, including the psoriasis area and severity index (PASI) score, involved body surface area, and physician's global assessment3,4,5, have their innate limitations as sole indicators. In this study, we investigated the correlation between quantitative histopathological grading systems and the clinical types of psoriasis, to determine whether histopathological grading could be used as a new tool for evaluating psoriasis severity. In addition, we intended to correlate the histopathological findings with the psoriasis severity index (PSI) score6,7, to elucidate whether the conventional clinical severity scoring tools could express histopathological severity so that evidence-based psoriasis severity assessment tools can be developed.
We retrospectively reviewed patients with psoriasis diagnosed both clinically and histopathologically through a skin biopsy. At the initial visits, a biopsy site was selected and the assessments of clinical severity with the PSI score of the site were documented in the electronic medical record. Photographs of the biopsy site were also taken. Only patients who had not received topical or systemic treatments, including topical vitamin D derivatives, topical corticosteroids, oral cyclosporine, oral vitamin A derivatives, or phototherapy, at 1 month before the visit were included in this study. Ethical approval for this study was obtained from the Seoul National University Bundang Hospital's institutional review board (IRB No. B-1005/099-301).
On the basis of the morphology of the lesions, the patients were individually classified into those having the guttate, papular, small plaque, and large plaque type. The guttate type was confirmed by the presence of eruptive small papules, usually accompanied by an acute infection such as streptococcal pharyngitis1. The papular type was defined as common papular psoriatic lesions <1 cm in diameter. Plaque-type psoriasis ranged from small plaques (mean diameter, <5 cm) to large plaques (mean diameter, >5 cm) to evaluate the effect of histopathological findings by lesion size. Pustular and erythrodermic psoriasis types were not included in the analysis. A single dermatologist with specialized experience in psoriasis clinically assessed the lesion severity at the biopsy site by using the PSI score to grade the erythema (PSI-E), induration (PSI-T), and scaliness (PSI-S) on a five-point scale: 0, none; 1, mild; 2, moderate; 3, severe; and 4, very severe.
The specimens were obtained by means of a 4-mm punch biopsy, and stained with hematoxylin-eosin (H&E). Histopathological findings of 10 representative features of psoriasis were investigated on each slide: regular elongation of the rete ridges, elongation of the dermal papillae, edema of the dermal papillae, dilated blood vessels, thinning of the suprapapillary plate, intermittent parakeratosis, absence of a granular layer, perivascular and dermal infiltrates of lymphocytes, spongiform pustules of Kogoj, and occasional neutrophil aggregates in the stratum corneum (Munro's microabscess). These 10 histopathological features were graded on a five-point scale according to their prominence: 0, none; 1, slight; 2, moderate; 3, marked; and 4, very marked. The sum of 10 grading scores per sample was defined as the psoriasis histopathologic score (PHS). Histopathological differences were analyzed according to the clinical type of psoriasis by using two measures: (i) the mean grade and overall frequency of each of the 10 histopathological findings and (ii) the PHS. We also performed a correlation analysis between the grading scores of each histopathological feature and the PSI scores.
The differences in clinical and histopathological findings according to the clinical types of psoriasis were analyzed by using one-way analysis of variance. The relation between the histopathological features and the PSI score was assessed with the Pearson's correlation test. Data were analyzed using SPSS software version 12.0 (SPSS Inc., Chicago, IL, USA) with a significance level of p<0.05.
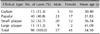
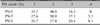
Ninety-eight lesions in 98 patients (57 men, 41 women; mean age, 34.1 years) were analyzed, which were categorized into the guttate (15.3%), papular (40.8%), small plaque (32.7%), and large plaque (11.2%) clinical types of psoriasis. Representative subjects of the four clinical types and their corresponding histopathology are shown in Fig. 1. The demographic information and details of each type are summarized in Table 1, and the patient distribution according to the PSI score is shown in Table 2.
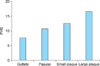
The mean values for each score of PSI-E, PSI-T, and PSI-S were calculated according to each morphologic type of psoriasis (Fig. 2). There were statistically significant differences in the mean scores for PSI-T and PSI-S among the four types of psoriasis, with a trend of increasing scores from the guttate type to the papular type to the plaque type. PSI-E showed no statistical difference.
The frequencies of each histopathological finding were investigated for all types of psoriasis and for each clinical type (Table 3). Overall, perivascular and dermal inflammatory cell infiltration was the most common finding (99%), followed by vascular dilatation (97%), absent granular layer (96%), regular elongation of the rete ridge (93%), elongation of the dermal papillae (93%), parakeratosis (93%), suprapapillary thinning (90%), spongiform pustules of Kogoj (55%), Munro's microabscess (54%), and edema of the dermal papillae (37%). The order of frequency remained similar when the analysis was performed separately for each type of psoriasis.
In the severity grading of histopathological findings, seven criteria, excluding spongiform pustules of Kogoj, Munro's microabscess, and inflammatory cell infiltration, were significantly different within the clinical types of psoriasis (Fig. 3). In the findings with significant differences, the mean PHSs were higher in the order from the large plaque type to the small plaque, papular, and guttate types. PHS was significantly higher in the order from the large plaque type (16.6±1.92) to the small plaque (12.5±3.03), papular (10.7±4.18), and guttate (7.6±3.81) types (Fig. 4).
No correlation was observed between histopathological severity grading and gross severity. We could not find a significant correlation of histopathological findings with PSI-E, PSI-T, or PSI-S.
No significant correlation was observed in the analysis between PSI scores and PHS (data not shown).
Conventional skin biopsy with H&E staining may provide the best qualitative microscopic information that could be used for evidence-based assessment. Some histopathological studies of psoriasis have examined the differences in histopathological findings before and after treatment8,9, the changes in histopathological findings according to the evolution of psoriatic lesions10,11,12, and the clinical types of psoriasis13. The information from these studies was limited because they were not designed for the quantitative grading of psoriasis severity based on histopathology. Newly developed noninvasive in vivo histological assessments such as reflectance confocal microscopy14, optical coherence tomography15,16, and sonography17 were also designed for descriptive diagnosis, not for quantitative assessment.
To our knowledge, this is the first study to attempt to correlate the histopathological findings of psoriasis with a psoriasis severity scoring system. PASI, which is an extension of PSI that includes body surface area factors, is a commonly used clinical severity assessment tool. However, PASI has always been criticized for its subjectivity and difficulty of use. PSI, which we have used in our study, is a psoriasis severity assessment method that comprises grading for erythema, thickness, and scaliness. Its grading scale is the same as that of PASI. PSI can be used only to describe the severity of the assessed lesion. Only one biopsy specimen from the patient is used for the diagnosis. However, in terms of the quantitative assessment of disease severity, the specimen only represents the severity of the analyzed lesion. Thus, we used the PSI score instead of the well-known PASI score to evaluate the correlations between gross and histopathological severity.
In our study, the histopathological findings of psoriasis showed substantial differences according to each clinical type. Seven of the 10 well-known psoriasis findings were present in >90% of the patients. When these histopathological findings were analyzed in terms of clinical types, most of the features, except Munro's microabscess, were more commonly noticed in the order from large plaque, small plaque, papular, to guttate types. Additionally, the number of positive findings within each sample significantly increased as the lesion size increased. Dermal inflammatory infiltrates and vascular dilatation were the most common findings; however, these are not specific for psoriasis. The loss of a granular layer, parakeratosis, regular elongation of the rete ridge, and elongation of the dermal papillae were the second most frequent findings. These are more specific findings and are more frequent in larger clinical types, as previously mentioned. Munro's microabscess and spongiform pustules of Kogoj are pathognomonic findings of psoriasis; however, these were relatively less frequent. Specifically, Munro's microabscess was found irrespective of the lesion size. This is because Munro's microabscess and spongiform pustules of Kogoj are not continuously located in the psoriatic epidermis. The reviewed biopsy section may not contain these findings even if the whole biopsy specimen contained these two findings. Conversely, the other more frequent findings are commonly found anywhere in the psoriatic epidermis and dermal papillae; thus, the frequencies of these findings were surely increased in larger lesions.
Regrettably, the PSI score components showed no statistical correlation with the histopathological grading. Nevertheless, even this negative result was also meaningful because we learned that a commonly used gross severity assessment tool such as PSI has its innate limitations when combined with histological findings. Both the arbitrariness and the crudeness of a discontinuous grading system in the five-point-scale PSI score and the five-point-scale histopathological grading system might be the main causes of these statistically non-significant differences. Additionally, PSI is a subjective grading system that inevitably has inaccuracies. To improve the statistical power, both PSI scores and histopathological grading should be upgraded to more precise, detailed, and continuous numerical parameters. Some studies have used objective bioengineering measurements to overcome the subjectivity of the PSI score6,7. Measurements of color, elasticity, and scale could be good substitutes for the PSI score without inter- or intra-rater variability. Additionally, adopting an objective image analysis of histological findings to quantitate the histopathological severity would be helpful to elucidate the clinical-histopathological severity correlation in an objective manner.
In conclusion, quantitative grading of histopathological features could reflect the clinical types of the biopsied site. Conversely, it could not represent a gross severity score of psoriasis. Thus, in this digital era, we need more objective, convenient, and less time-consuming tools that could better reflect the clinical-histopathological assessment of psoriasis severity than does PSI. Bioengineering measurements in combination with computer-aided image analysis will be at the forefront of this change.
Figures and Tables
Fig. 1
Classification of the clinical types and histopathological features of the corresponding psoriatic lesions (H&E, ×100). (A) Guttate type, (B) papular type, (C) small plaque type, and (D) large plaque type.

Fig. 2
Mean psoriasis severity index (PSI) scores in each clinical type of psoriasis, and comparisons according to the clinical types. Thickness and scale parameters showed statistically significant increases according to the gross morphological severity. Erythema showed no statistical significance. *p<0.05.

Fig. 3
Mean of histologic grades according to the clinical types of psoriasis. Most of the histologic findings showed significant change as the gross lesion size increased. *p<0.05.

Fig. 4
Psoriasis histopathologic score (PHS) according to the clinical types of psoriasis. Significant differences were found in different types of psoriasis (p<0.05).
References
1. Gudjonsson JE, Elder JT. Psoriasis. In : Goldsmith LA, Katz SI, Gilcrest BA, Paller AS, Leffell DJ, Wolff K, editors. Fitzpatrick's dermatology in general medicine. 8th ed. New York: McGraw-Hill;2012. p. 197–231.
2. Mobini N, Toussant S, Kamino H. Noninfectious erythematous, papular, and squamous diseases. In : Elder DE, editor. Lever's histopathology of skin. 10th ed. Philadelphia: Lippincott Williams & Wilkins;2009. p. 169–203.
3. Puzenat E, Bronsard V, Prey S, Gourraud PA, Aractingi S, Bagot M, et al. What are the best outcome measures for assessing plaque psoriasis severity? A systematic review of the literature. J Eur Acad Dermatol Venereol. 2010; 24:Suppl 2. 10–16.

4. Garduno J, Bhosle MJ, Balkrishnan R, Feldman SR. Measures used in specifying psoriasis lesion(s), global disease and quality of life: a systematic review. J Dermatolog Treat. 2007; 18:223–242.

5. Spuls PI, Lecluse LL, Poulsen ML, Bos JD, Stern RS, Nijsten T. How good are clinical severity and outcome measures for psoriasis?: quantitative evaluation in a systematic review. J Invest Dermatol. 2010; 130:933–943.

6. Kim JH, Kim BY, Choi JW, Kim SO, Lee HS, Park KC, et al. The objective evaluation of the severity of psoriatic scales with desquamation collecting tapes and image analysis. Skin Res Technol. 2012; 18:143–150.

7. Choi JW, Kwon SH, Youn JI, Youn SW. Objective measurements of erythema, elasticity and scale could overcome the inter- and intra-observer variations of subjective evaluations for psoriasis severity. Eur J Dermatol. 2013; 23:224–229.

8. Cox AJ, Watson W. Histological variations in lesions of psoriasis. Arch Dermatol. 1972; 106:503–506.

9. Griffin TD, Lattanand A, VanScott EJ. Clinical and histologic heterogeneity of psoriatic plaques. Therapeutic relevance. Arch Dermatol. 1988; 124:216–220.

10. Beek CH, van Reede EC. The nature and frequency of thehistological changes found in psoriasis vulgaris. Arch Dermatol Res. 1977; 257:255–264.

12. Ragaz A, Ackerman AB. Evolution, maturation, and regression of lesions of psoriasis. New observations and correlation of clinical and histologic findings. Am J Dermatopathol. 1979; 1:199–214.
13. Murphy M, Kerr P, Grant-Kels JM. The histopathologic spectrum of psoriasis. Clin Dermatol. 2007; 25:524–528.

14. Ardigo M, Cota C, Berardesca E, González S. Concordance between in vivo reflectance confocal microscopy and histology in the evaluation of plaque psoriasis. J Eur Acad Dermatol Venereol. 2009; 23:660–667.

15. Morsy H, Kamp S, Thrane L, Behrendt N, Saunder B, Zayan H, et al. Optical coherence tomography imaging of psoriasis vulgaris: correlation with histology and disease severity. Arch Dermatol Res. 2010; 302:105–111.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download