This article has been corrected. See "Erratum: Neutrophilic Dermatosis Confined to the Lymphedematous Area" in Volume 29 on page 134.
Dear Editor:
Lymphedema is a common sequelae after cancer surgery with lymph node dissection1. A lymphedematous limb, which is prone to the development of infections or tumors, suggests an alteration in regional immune competence2. Neutrophilic dermatosis on postmastectomy lymphedema (NDPL) is a newly suggested disease by Demitsu and Tadaki3 It is also referred to as localized Sweet's syndrome (SS) because of the histological similarities between the two conditions4. Herein, we report additional cases of neutrophilic dermatosis confined within a lymphedematous site and a review of the disease entity.
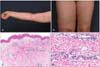
All three cases involved female patients, two of whom were breast cancer patients who underwent modified radical mastectomy with axillary lymph node dissections (Table 1). The third patient had undergone radical hysterectomy with pelvic lymph node dissection for cervical cancer. Lymphedema was confined to the lymphnode-dissected limb developed in all three patients after the surgery. All of them rapidly developed erythematous rashes on their lymphedematous limb (Fig. 1A, B). Skin biopsy revealed marked papillary dermal edema and dense dermal neutrophil infiltrates, consistent with the histopathologic features of SS (Fig. 1C, D). The laboratory findings, including white blood cell count, percentage of neutrophils, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP), were within the normal ranges, except in case 3 (ESR: 35 mm/h; CRP: 4.09 mg/dl). Each case was treated with topical or oral corticosteroid, or oral antibiotics. In case 3, the lesion recurred rapidly after initially being treated with oral antibiotics. After the administration of oral corticosteroid, the lesion rapidly resolved within 1 week. On the basis of the characteristic distribution of the lesion and the histopathologic features, a diagnosis of 'neutrophilic dermatosis on the lymphedematous area' was made.
Neutrophilic dermatosis or SS localized on the area of lymphedema is rare, and only 11 cases have been reported1,3,4. The clinical presentations of previously reported cases were erythematous papules, plaques, and vesicles on the lymphedematous arm after a mastectomy, which are consistent with our cases1,3,4. The pathomechanism cannot be fully demonstrated; however, the vulnerability of the lymphedematous area seems to be the main factor1,2,5. The stasis of protein-rich lymphatic fluid contains numerous cytokines that might attract neutrophils and also result in the impairment of immune surveillance2,5. Because this dermatosis shows typical clinicohistopathological findings of SS, they are considered a localized variant of SS4. However, other systemic presentations, such as leukocytosis, neutrophilia, or fever, were less frequent than in typical SS. Therefore, several other reports suggested the use of the new term NDPL1,3. Other clinical differential diagnosis included cellulitis or erysipelas. Contrary to cellulitis or erysipelas, the lesion was confined only to the lymphedematous area and was well treated with oral or topical corticosteroid1,4. Although the 11 reports to date were cases of a lesion on a lymphedematous arm after a mastectomy, our report includes one case of a lesion that had developed on the lymphedematous leg after a hysterectomy for cervical cancer. Consequently, our cases suggest a novel point that a lesion could develop on any lymphedematous limb after lymph node dissection. Therefore, we suggest the term 'neutrophilic dermatosis on the lymphedematous area' rather than NDPL.
Figures and Tables
Fig. 1
(A) Case 1. Multiple variable-sized erythematous papules, vesicles, and plaques localized on the right lymphedematous arm. (B) Case 3. Multiple erythematous papules and patches confined on the left lymphedematous leg. (C, D) Histopathological findings. Skin biopsy taken from the patient of case 1, showing marked papillary dermal edema and dense dermal neutrophil infiltrates (H&E; C: ×40, D: ×200).
References
1. Lee CH, Lee HC, Lu CF, Hsiao CH, Jee SH, Tjiu JW. Neutrophilic dermatosis on postmastectomy lymphoedema: a localized and less severe variant of Sweet syndrome. Eur J Dermatol. 2009; 19:641–642.

2. Mallon E, Powell S, Mortimer P, Ryan TJ. Evidence for altered cell-mediated immunity in postmastectomy lymphoedema. Br J Dermatol. 1997; 137:928–933.

3. Demitsu T, Tadaki T. Atypical neutrophilic dermatosis on the upper extremity affected by postmastectomy lymphedema: report of 2 cases. Dermatologica. 1991; 183:230–230.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download