Dear Editor:
The efficacy of ultraviolet A1 (UVA1, 340~400 nm) in the treatment of mycosis fungoides (MF) appears to be equal to or better than psoralen UVA (PUVA), and may be more effective for nodular and thick plaque lesions1. There are several reports regarding the effectiveness of UVA1 for MF1,2. However, no study to date in Asians has described the patient response to UVA1 therapy for the treatment of MF according to a low-, medium-, or high-dose regimen.
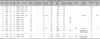
Fourteen patients with histologically proven MF (9 males, 5 females, mean age 43.8 years, age range 14~67 years) were enrolled in this study. The duration of diseases ranged from 2 months to 10 years (mean, 4.2 years). Ten patients (71.4%) had stage IA, 3 (21.4%) had stage IB, and 1 (7.1%) had stage IVB of the TNM staging system.
Patients were treated with low-dose (20 J/cm2), medium-dose (65 J/cm2) or high-dose (100 J/cm2) UVA1. The UVA1 therapy was delivered by a SELLAMED 3000® (Sellas Medizinische Gerate GmbH, Gevelsberg, Germany). The main wavelengths were emitted from 340 nm to 400 nm. The irradiation intensity was 70 mW/cm2. The frequency of therapy was 3 to 5 times per week.
Clinical response was graded as complete response (CR, 95~100%), partial response (PR, 50~95%), and no response (<50%). Biopsies were taken after treatment in 5 of 14 patients.
Three patients were treated with low-dose UVA1 therapy. CR was observed in 3 patients (100%). None of the 3 patients with CR relapsed over a median period of 62 months after treatment.
Seven patients were treated with medium-dose UVA1. Of the 7 patients, CRs and PRs were achieved in six (85.7%), and one (14.3%) patient, respectively. One of the 6 patients with CR relapsed after 30 months. The patient that relapsed achieved a CR after an additional 14 irradiations with medium-dose UVA1, and did not relapse for 34 months. None of the 5 patients with CR relapsed over a median period of 35 months after treatment.
Four patients were treated with high-dose UVA1. Two patients exhibited a CR and 2 patients had a PR. In 1 of the 2 patients with CR, the skin lesions relapsed. The relapsed patient showed a CR after 39 treatment sessions of UVA1, but the skin lesions relapsed after another 6 months. This patient again achieved a CR after 11 more irradiations with high-dose UVA1 and did not relapse for 35 months. The other patient who exhibited CR did not relapse at a follow-up of 33 months. Among the 14 patients with MF treated in our study, CRs and PRs were observed in 11 (78.5%) and 3 (21.5%) patients, respectively (Fig. 1). The mean number of treatments in patients with a CR was 22.0 within a mean time of 41.3 months (range, 2~120 months). In this study, CR was observed between 9 and 50 exposures regardless of the dosages of UVA1. In low-dose UVA1 therapy, CR was observed in all 3 patients after a mean number of 16.7 UVA1-irradiations. In medium-dose UVA1 therapy, CR was observed in 6 patients after a mean number of 24.2 UVA1-irradiations. In high-dose UVA1 therapy, CR was observed in 2 patients after a mean number of 36 UVA1-irradiations.
During patient follow-up (range 21 to 88 months), only 2 of 14 patients relapsed. The 2 relapsed patients responded faster to a second course of UVA1 therapy than the first treatment suggesting that acute lesions quickly responded to UVA1 therapy.
Five patients were evaluated histopathologically after completed treatment. CRs and PRs were observed in 4 and 1 patients, respectively. No serious adverse effects were observed except for hyperpigmentation (Table 1).
Currently, phototherapy is a main treatment option in early stage MF. In a meta-analysis study, CR rates ranged from 54% to 91% in patients with MF treated with narrowband ultraviolet B1 (NB-UVB) or PUVA3.
In addition, UVA1 phototherapy also has a favorable and fast therapeutic effectiveness in localized thick and nodular lesions. Our study showed a 78.5% overall complete remission rate. The effectiveness of UVA1 can be related to its penetration depth and ability to mediate different forms of apoptosis. Specifically, UVA1 penetrates deeper than PUVA and NB-UVB4,5. Thus, the duration of CR by UVA1 is typically shorter than PUVA and NB-UVB for palmar or plantar MF. In addition, UVA1 can induce both a protein synthesis dependent (programmed cell death) and protein synthesis independent (pre-programmed cell death) apoptotic mechanism6,7. Furthermore, UVA1 phototherapy has no adverse effect of psoralen sensitization.
Plettenberg et al.2 demonstrated that medium and high-dose UVA1 phototherapy leads to complete clearance. In another study, one patient with MF (stage III) showed marked improvement after 15 sessions of medium-dose UVA18. These results showed medium-dose UVA1 is sufficient to induce marked apoptosis in dermal T-cells.
Zane et al.1 reported that 11 of 13 patients treated with high-dose UVA1 showed CR, with 7 of the patients who exhibited a CR not experiencing recurrence during a mean follow-up of 7.2 months, while the other 4 patients relapsed within 3 months. Yamauchi et al.7 found that malignant T cells are more sensitive than normal cells in UVA1 radiation-induced apoptosis. In addition, good therapeutic responses were observed in both medium- and high-dose UVA1. As a consequence, they did not use the high-dose regimen in the treatment of MF. We also observed the therapeutic improvement in all low-, medium- and high-dose UVA1. Thus, the results of our study suggest that the therapeutic effectiveness for MF may be unrelated to UVA1 dose.
UVA1 may cause minimal erythema, burning sensation, dryness and hyperpigmentation as short-term side effects. The long-term side effects such as carcinogenesis have so far not been established. Although high doses of UVA1 induced carcinogenesis in some studies, there have been few reported cases of malignant skin cancer9,10. However, based on this observation, a lower cumulative dose from the use of low- and medium-dose UVA1 is likely advantageous compared with a high-dose UVA1 regimen.
Our data indicate that UVA1 phototherapy is a well tolerated therapeutic treatment, with excellent results in patients with MF, irrespective of the dose regimen.
Figures and Tables
References
1. Zane C, Leali C, Airò P, De Panfilis G, Pinton PC. "High-dose" UVA1 therapy of widespread plaque-type, nodular, and erythrodermic mycosis fungoides. J Am Acad Dermatol. 2001. 44:629–633.

2. Plettenberg H, Stege H, Megahed M, Ruzicka T, Hosokawa Y, Tsuji T, et al. Ultraviolet A1 (340~400 nm) phototherapy for cutaneous T-cell lymphoma. J Am Acad Dermatol. 1999. 41:47–50.

3. Carter J, Zug KA. Phototherapy for cutaneous T-cell lymphoma: online survey and literature review. J Am Acad Dermatol. 2009. 60:39–50.

4. Breuckmann F, von Kobyletzki G, Avermaete A, Radenhausen M, Höxtermann S, Pieck C, et al. Mechanisms of apoptosis: UVA1-induced immediate and UVB-induced delayed apoptosis in human T cells in vitro. J Eur Acad Dermatol Venereol. 2003. 17:418–429.

5. Weichenthal M, Schwarz T. Phototherapy: how does UV work? Photodermatol Photoimmunol Photomed. 2005. 21:260–266.

6. Godar DE. UVA1 radiation triggers two different final apoptotic pathways. J Invest Dermatol. 1999. 112:3–12.

7. Yamauchi R, Morita A, Yasuda Y, Grether-Beck S, Klotz LO, Tsuji T, et al. Different susceptibility of malignant versus nonmalignant human T cells toward ultraviolet A-1 radiation-induced apoptosis. J Invest Dermatol. 2004. 122:477–483.

8. Von Kobyletzki G, Heine O, Stephan H, Pieck C, Stücker M, Hoffmann K, et al. UVA1 irradiation induces deoxyribonuclease dependent apoptosis in cutaneous T-cell lymphoma in vivo. Photodermatol Photoimmunol Photomed. 2000. 16:271–277.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download