Abstract
Background
Determination of the minimal erythema dose (MED) is important for developing a phototherapy protocol and to diagnosis photosensitivity disorders. But obtaining a precise and reproducible MED is quite difficult because a phototest for erythema is based on subjective assessment.
Objective
The objective of our study was to compare the gross interpretation of a phototest and the objective measurement using a spectrophotometer for determining the parameters of cutaneous narrow-band UVB (NBUVB) therapy.
Methods
A total of 14 psoriasis and 10 vitiligo patients who receiving NBUVB phototherapy with skin types III and IV were selected for this study. To perform phototesting, ten sites on the skin of the back were vertically exposed to a series of 10 NBUVB doses among 14 doses between 340 and 1,400 mJ/cm2. We interpreted the gross findings of erythema and measured the L*a*b* values with using a spectrophotometer at each phototest spot and at the control skin. Also, we evaluate the relationship between the gross presentation and the spectrophotometric analysis by delta E for the assessment of the minimal perceptible erythema (MPE) and MED.
Results
For all the subjects, the MEDs were measured in the 490~1,000 mJ/cm2 range. The average of the colorimetric values for the control skin were L*: 64.8, a*: 7.9 and b*: 19.8. Among them, the L* value and MED value were shown to be inversely correlated, and as the L* value was decreased, the MED was increased. For the MPE, the delta E, which was the color difference of the normal skin and the phototest area, was within the range of 1.5~3.0 in 17 of the 21 patients, and 4 patients were within the range of 1.0~1.5. For the MED, among the 21 patients, the delta E of 17 patients was within the range of 3.0~6.0, and 4 patients were within the range of 6.0~12.0.
Conclusion
A spectrophotometer enables UV erythema to be assessed objectively and quantitatively, and this can compensate for the disadvantages of subjective gross interpretation when determining the MED. Delta E is a good novel and objective indicator for determining the MPE and MED. So, a spectrophotometer is a very useful instrument for developing a phototherapy protocol for psoriasis and other dermatoses and for making the diagnosis of photosensitivity disorders.
Narrow-band UVB (NBUVB) has recently been widely applied to treat to psoriasis, vitiligo and atopic dermatitis, and excellent treatment outcomes have been reported1. Phototherapy protocols have been actively developed for the initial irradiation dose and increasing the dose according to the erythematous reactions and the skin phototype. Determining the minimal erythema dose (MED) is important for conducting phototherapy and for making the diagnosis of photosensitivity disorder2. Nonetheless, the MED is based on the subjective evaluation of the erythema, and so this has the shortcomings of low accuracy and reproducibility.
A spectrophotometer is an instrument that quantitates colors by applying tristimulus values or values corresponding to the basic colors, and this spectrophotometer has been actively used in the dermatologic field and it can objectively and quantitatively evaluate the erythema and pigmentation induced by UV radiation3. The spectrophotometer primarily presents the color of materials as the L*a*b* color space parameter (L*a*b* values): brightness is presented as L*, chromacity that shows hue and saturation are presented as a* and b*, and it presents the color differences as delta E by combining these values. In recent years, it has been reported that L* is associated with constitutive skin color and so it is significantly correlated to the MED4, and a* is a value associated with erythema. Yet there is scant information associated with delta E that sums up the brightness, hue and saturation.
Most Koreans have skin that is of the high Fitzpatrick skin type (phototype III, IV) and the mid-latitude as well as the facultative skin color depend on the season, which both influence the gross interpretation of MED. So we examined whether the objective evaluation of erythema by using a spectrophotometer is an effective alternative for determining the MED.
Among the patients who visited our hospital from March 2005 to December 2006, we selected 14 psoriasis patients and 10 vitiligo patients as the subjects for our study. There were 10 male patients and 14 female patients (age range: 8 to 73 years, mean age: 40 years). All the patients were surveyed by a questionnaire in order to assess their Fitzpatrick skin types. The patients who had a past history of phototherapy, hepatic dysfunction or renal dysfunction, photosensitivity disorder, diabetes mellitus, pregnancy, breast feeding, those planning to become pregnant, those taking photosensitive drugs or those who undergone long term radiation therapy were excluded (Table 1).
An ultraviolet cabinet (Waldmann UV1000KL, Waldmann Co., Germany) with an attached fluorescence lamp that emitted a 311 nm continuous wavelength of lite (Waldmann F85/100W, TL-01, Waldmann Co., Germany) was used. A questionnaire was used at the initial visit to assess the weight and height of the patients, the area that developed psoriasis, the duration of illness, the family medical history, the patient's treatment history, the past history of systemic diseases and the skin phototype.
The spectrophotometer presents the hue, brightness and saturation of materials as L*a*b*. L* represents the brightness, an increase indicates more brightness and a decrease indicates more darkness. a*b* indicates the color direction, and the increase of a* indicates red, a decrease of a* indicates the color direction toward green, and as b* is increased, it indicates the color direction toward yellow, and the decrease of b* implies the color direction toward blue. Delta E numerically represents the difference between two colors, and it could be obtained by the application of the following formula, and its meaning is shown in Table 25.
ΔE=[(ΔL*)2+(Δa*)2+(Δb*)2]1/2
For the Waldmann 1,000 K cabinet, among the 311 nm UVB 340~1,400 mJ/cm2 light settings (a total of 14 grades), 10 grades were irradiated to the back vertically, and the MED was evaluated after 24 hours. On each phototest area of the total 24 patients, skin color (L*a*b*) was measured as the constitutive skin color by using the spectrophotometer CM-2006d (Minolta Co. Ltd, Osaka, Japan) (Fig. 1). The buttock skin was used as the normal control group, and its skin color (L*a*b*) was measured. The delta E between the phototest area and the normal control skin was calculated for 21 patients.
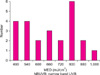
For 24 patients (14 psoriasis patients and 10 vitiligo patients), the MED was measured in the range of 490~1,000 mJ/cm2 (mean MED: 679.2 mJ/cm2) (Fig. 2). No statistically significant difference was observed according to the age group. No significant relationships were found between previous treatment and the MED.
According to Fitzpatrick's classification, the skin types of the 24 patients were distributed as follows: type III: 17 and type IV: 7 (Table 3). No significant relationships were found between previous treatment and the skin types.
Regarding the result of the measurement of the normal control skin by the spectrophotometer, the mean L* value was 64.8, the mean a* was 7.9 and the mean b* value was 19.8 (Fig. 3). Among them, the L* value and the MED value were shown to be inversely correlated: as the L* value was decreased, the MED was increased (L* value=70.0~0.00776 MED, p<0.001). However, the a* value and b* value did not show any significant correlation with the MED.
For the MPE, the delta E, which is the color difference of the normal skin and the phototested area, was within the range of 1.5~3.0 and this showed a visible difference and could not be accepted as a same color by the spectrophotometer for 17 of the 21 patients. Four patients had a delta E that was within the range of 1.0~1.5, which could be accepted as a same color by the spectrophotometer (Fig. 4). For the MED, among the 21 patients, the delta E of 17 patients was within the range of 3.0~6.0, which could be accepted as different colors, and 4 patients were within the range of 6.0~12.0, which showed a distinct color difference (Fig. 5).
The MED and the minimal melanogenic dose (MMD) have been widely used as an objective index of erythema and the color caused by UV radiation, respectively. However, the above methods rely on the gross evaluation by examiners, and so the MED and MMD may be different among examiners depending on the individual experience and the subjective index, and they could be different depending on the lighting at the time of examination and the facultative skin color of the subject6. For the treatment of psoriasis and vitiligo, the method using the NBUVB has recently been widely used7-9, and although objective methods that measure skin reactions on phototests and in response to phototherapy are required, any studies on these objective methods are currently not sufficient.
The equipment used to objectively measure the MED includes the laser Doppler blood flowmeter, the skin reflectance instrument, the spectrophotometer etc10. Among them, the spectrophotometer is a tool that measures color values under artificial light that is delivered to a target, according to the regulations of the Commission Internationale de I'Éclair age (CIE). The reflected light is sent to a diffraction grating system that separates the reflected light according to waves. The reflexibility value of the separated light is measured by a photodiode array detector and the values are integrated to form a reflexibility value curve. The errors of the level of erythema and the pigmentation of the skin, which are caused by the subjective determination of examiners, can be overcome by using the spectrophotometer4, and the spectrophotometer can be applied to assess the effectiveness of various therapies such as drug application, laser etc11-13.
We routinely see several colors simultaneously, and in such cases, because of the mutual action of the colors, phenomena occur that are different from those that occur with observing one color at a time. Particularly, the difference of chromacity is perceived by the visual sense, and this sense is very relative, and so understanding the attributes that allow us to sense the color differences and also training for sensing color differences are required14. Such points also influence determining the MED and MMD, which evaluate the macroscopic change of erythema after UVB irradiation. If a spectrophotometer is used, then colors are measured by installing sensors comparable to the human eye and with using a constant light source and method; hence, this way of measuring colors is not influenced by environmental conditions. The spectrophotometer presents the color by evaluating its hue, brightness and saturation with using color space parameters15 and among them, the L*a*b* color space parameter has been standardized by the CIE in 1976, and it is now commonly used in many fields16.
For 24 patients (14 psoriasis patients and 10 vitiligo patients), we quantitatively evaluated the level of erythema and pigmentation that developed after NBUVB radiation with using a spectrophotometer and we compared these evaluated levels of erythema and pigmentation with those of gross interpretation. The measured L* value of the normal control skin showed a significant correlation to the MED, which is in agreement with the previous reports4. The value of a* and the value of b* did not show a significant correlation to the MED.
However, a color cannot be explained by only one index among hue, brightness and chromacity, and so to compensate for this, the concept of delta E was introduced. As a result, the difference of two colors can be obtained by delta E, and the delicate differences of colors can also be distinguished17,18. According to Österberg et al5, the measured delta E could be differently interpreted for determining the range of color differences that could not be measured by a spectrophotometer to assess the color difference that could be evaluated as definitely different colors according to the ranges (Table 2). Based on this, we defined the delta E value in the range of 1.5~3.0 as showing a visible difference and the colors could not accepted as a same color by the spectrophotometer as the index of the MPE, and the delta E value in the range 3.0~6.0 that could be accepted as different colors as the index comparable to the MED. We then calculated the delta E between the normal control group skin and the phototest area of the 21 patients and compared the delta E with gross interpretation. Regarding comparison of the delta E against the MPE, among 21 patients, 17 patients showed measurement values of 1.5~3.0. In addition, for comparison of the delta E against the MED, among 21 patients, 17 showed the measurement value in the range of 3.0~6.0 and 4 patients showed the measurement value of 6.0~12.0, which showed distinct color differences. In most patients, gross interpretation and the delta E value measured by spectrophotometer showed comparable values, yet in some patients, the delta E value was measured to be higher than the delta E against the MED. Thus it was found that gross interpretation and the objective measurement values could be different. It appears that for such cases whose MED value was hard to determine, a more objective evaluation of the erythematous reaction could be done when applying the delta E value as a supplement.
NBUVB has been regarded as the ideal UVB source for phototherapy for psoriasis and vitiligo. To optimize the therapeutic response with using NBUVB rays and to exclude the possible risks of intensive burns, most of the previous studies have recommended 70% of the MED as the initial dosage for treating psoriasis and vitiligo patients. We measured the delta E value, which is the color difference between the phototest areas and the normal control group skin corresponding to the MPE and MED, respectively, and we determined the 70% dosage corresponding to the delta E value in the range of 3.0~6.0 as the initial dosage for treating psoriasis and vitiligo patients. The delta E value was confirmed to be one of the alternatives that could compensate for the subjective evaluation of the MED by examiners. There have been no previous studies showing the possible use of this method, and so further studies in this are needed.
In the field of dermatology, the spectrophotometer is currently being used to evaluate the color of rosacea and pigmentary lesions, and it has been applied to assess the effectiveness of laser treatment13. In our study, erythematous and pigmentation reactions in response to NBUVB were measured by the spectrophotometer, and the level of erythematous and color reactions according to each radiation dose could be measured objectively and quantitatively by the use of delta E, and particularly, it could supplement the subjective gross interpretation during the process of measuring the MED, which is essential in the field of photomedicine. Thus, a spectrophotometer and determining the delta E are useful tools for establishing phototherapy protocols for psoriasis and other diseases and for making the the diagnosis of photosensitivity disorder.
Applying a spectrophotometer that could quantitatively measure erythematous and pigmentation reactions, we irradiated 24 patients (14 prosiaris patients and 10 vitiligo patients) with NBUVB, we measured the erythematous and pigment reactions according to each radiation dose and the following results were obtained.
1. In 24 patients (14 psoriasis patients and 10 vitiligo patients), the MED was measured to be in the range of 490~1,000 mJ/cm2 (average MED: 679.2 mJ/cm2).
2. Regarding the result of the measurement of the normal area skin (the control group) by the spectrophotometer, the L* value was an average of 64.8, the a* value was an average of 7.9 and the b* value was an average 19.8. Among them, the L* value and the MED value were inversely correlated, and as the MED increased, the L* value was decreased.
3. For the case of delta E compared with the MPE, among the 21 patients, 17 patients showed a delta E in the range of 1.5~3.0, which showed a visual difference and this could not be accepted as an identical color by the spectrophotometer. In the case of delta E compared with the MED, among 21 patients, 17 patients showed a delta E in the range of 3.0~6.0, which could be accepted as an identical color. Delta E presents the delicate difference of colors as an objective numerical value, and it has a meaning as an important index to determine MPE and MED.
We were able to objectively measure erythematous and pigmentation reactions in response to NBUVB with using a spectrophotometer, and it is thought that the values obtained from this could be used as an objective index of skin reactions to UV radiation.
Figures and Tables
References
1. Choe YB, Park SB, Yoon JI. Narrow-band UVB phototherapy in Korean psoriasis patients. Korean J Dermatol. 2000. 38:358–362.
2. Rim JH, Choe YB, Youn JI. Minimal erythema dose of narrow band UVB in Korean psoriasis patients. Korean J Dermatol. 2001. 39:883–886.
3. Park SB, Huh CH, Choe YB, Youn JI. Time course of ultraviolet-induced skin reactions evaluated by two different reflectance spectrophotometers: DermaSpectrophotometer and Minolta spectrophotometer CM-2002. Photodermatol Photoimmunol Photomed. 2002. 18:23–28.

4. Youn JI, Park JY, Jo SJ, Rim JH, Choe YB. Assessment of the usefulness of skin phototype and skin color as the parameter of cutaneous narrow band UVB sensitivity in psoriasis patients. Photodermatol Photoimmunol Photomed. 2003. 19:261–264.

5. Österberg F. The visual impact of lamination [Internet]. 2005. 02. 08. cited 2007 Nov 6. Sweden: Linköpings universitet, Department of Science and Technology;Available from: http://www.t2f.nu/t2frapp_f_144.pdf.
6. Farr PM, Diffey BL. Quantitative studies on cutaneous erythema induced by ultraviolet radiation. Br J Dermatol. 1984. 111:673–682.

7. Picot E, Meunier L, Picot-Debeze MC, Peyron JL, Meynadier J. Treatment of psoriasis with a 311-nm UVB lamp. Br J Dermatol. 1992. 127:509–512.

8. Karvonen J, Kokkonen EL, Ruotsalainen E. 311 nm UVB lamps in the treatment of psoriasis with the Ingram regimen. Acta Derm Venereol. 1989. 69:82–85.
9. Picot E, Picot-Debeze MC, Meunier L, Peyron JL, Meynadier J. Narrow-band UVB phototherapy (Philips TL01 lamps) in psoriasis. Ann Dermatol Venereol. 1992. 119:639–642.
10. Taylor S, Westerhof W, Im S, Lim J. Noninvasive techniques for the evaluation of skin color. J Am Acad Dermatol. 2006. 54:S282–S290.

11. Andersen PH, Abrams K, Maibach H. Ultraviolet B dose-dependent inflammation in humans: a reflectance spectroscopic and laser Doppler flowmetric study using topical pharmacologic antagonists on irradiated skin. Photodermatol Photoimmunol Photomed. 1992. 9:17–23.
12. Zachariae R, Oster H, Bjerring P. Effects of hypnotic suggestions on ultraviolet B radiation-induced erythema and skin blood flow. Photodermatol Photoimmunol Photomed. 1994. 10:154–160.
13. Kawana S, Ochiai H, Tachihara R. Objective evaluation of the effect of intense pulsed light on rosacea and solar lentigines by spectrophotometric analysis of skin color. Dermatol Surg. 2007. 33:449–454.

14. Yap AU, Sim CP, Loh WL, Teo JH. Human-eye versus computerized color matching. Oper Dent. 1999. 24:358–363.
15. Jorgenson MW, Goodkind RJ. Spectrophotometric study of five porcelain shades relative to the dimensions of color, porcelain thickness, and repeated firings. J Prosthet Dent. 1979. 42:96–105.

16. Kuehni RG. Color-tolerance data and the tentative CIE 1976 L a b formula. J Opt Soc Am. 1976. 66:497–500.




 PDF
PDF ePub
ePub Citation
Citation Print
Print









 XML Download
XML Download