Abstract
NK/T-cell lymphoma (NKTCL) is characterized by the expression of the NK-cell antigen CD56. Non-nasal NK/T-cell lymphomas are subdivided into primary cutaneous and 4 subtypes of secondary cutaneous lymphomas; nasal type, aggressive, blastic (blastoid), and other specific NK-like cell lymphoma. Aggressive NK/T-cell lymphoma/leukemia is a rare leukemic variant of nasal type NKTCL. We herein report a rare case of aggressive NK/T-cell lymphoma/leukemia with cutaneous involvement in adolescence.
NK/T-cell lymphomas (NKTCL) are a rare but clinically important group of neoplasms. Most of these diseases undergo aggressive clinical courses,with a high rate of mortality. Pathologically, NKTCL show a polymorphic neoplastic infiltrate with an angioinvasive and angiodestructive pattern. Lymphoma cells express a characteristically CD2+, CD56+, cytoplasmic CD3ε+ immunophenotypes and frequently show negativity for other T-lineage markers123.
NKTCL can involve the skin in a primary or secondary fashion. NKTCL are subdivided into nasal NKTCL and non-nasal NKTCL. Although the nasal NKTCL commonly present as a midfacial destructive disease, the non-nasal NKTCL often arise in extranodal locations, including the skin. Non-nasal NKTCL are then further subdivided into primary cutaneous and 4 subtypes of secondary cutaneous lymphomas; nasal type NKTCL, aggressive NK/T-cell lymphoma/leukemia (ANKTCL), blastic (blastoid) NKTCL, and other specific NK-like cell lymphoma3.
A 14-year-old Korean boy presented with a 1-month history of multiple, deep-seated, erythematous nodules on the left upper eyelid, neck and both thighs. He had been experiencing fever, fatigue and weight loss for 2 months. The patient appeared acutely ill, and intermittent fevers up to 39.5oC were recorded. Physical tests showed multiple, asymptomatic, deep-seated, erythematous nodules with central necrotic crusts on the left upper eyelid, neck and both thighs (Fig. 1). He had hepatosplenomegaly without peripheral lymphadenopathy. Laboratory examination revealed leukopenia (leukocyte count 1.33×109/L; normal 3.3~10.7×109/L), thrombocytopenia (platelet count 38×106/L; normal 140~440×106/L), and elevated liver enzymes (lactate dehydrogenase 941 U/L, normal 101~218 U/L; aspartate aminotransferase 347 U/L, normal 0~40 U/L; alanine aminotransferase 202 U/L, normal 0~40 U/L). A peripheral blood smear revealed atypical lymphoid cells with irregular nuclear margins and fine azurophilic granules in the cytoplasm (Fig. 2A). Bone marrow examination showed atypical immature lymphoid cells and several hemophagocytic macrophages (Fig. 2B). Computed tomographic scans revealed marked hepatosplenomegaly, pleural effusion, and ascites. Skin biopsy specimens demonstrated dense perivascular infiltration of atypical polymorphic lymphoid cells and extensive necrosis throughout the dermis (Fig. 3). Using immunohistochemical analysis, these cells were found to be CD3-, CD4-, CD5-, CD8-, CD20-, CD45+, CD56+ and CD68- (Fig. 4A). EBER in situ hybridization for Epstein-Barr virus was positive in the infiltrated lymphoid cells (Fig. 4B).
Based on the results of laboratory and histopathological findings, this case was diagnosed as an aggressive NK/T cell lymphoma/leukemia. He was scheduled to receive chemotherapy and bone marrow transplantation, but transferred to another tertiary hospital by his parents' wishes.
NK/T-cell lymphomas (NKTCL) have been increasingly recognized over the past decade with the advances in immunohematology. In the past, these lymphomas were often diagnosed as one of the following entities: lethal midline granuloma, midline malignant reticulosis, lymphoma of large granular lymphocytes, CD56+ angiocentric T-cell lymphoma, and CD56+ hematolymphoid malignancy367. This confusion was caused by the uncertain origin of these uncommon lymphomas. Now, these CD56+ lymphomas are better designated as NKTCL because they express NK-cell markers and a limited number of T-cell markers7.
World Health Organization (WHO) classification subdivided NKTCL into 4 types; extranodal nasal type NKTCL, enteropathy-type T-cell lymphoma, blastic NK-cell lymphoma and aggressive NK-cell leukemia8. But Radonich et al3 subdivided NKTCL into 2 subtypes; nasal NKTCL and non-nasal NKTCL. Non-nasal NKTCL are then further subdivided into primary cutaneous and 4 subtypes of secondary cutaneous lymphomas; nasal type NKTCL, aggressive NK/T-cell lymphoma/leukemia (ANKTCL), blastic (blastoid) NKTCL, and other specific NK-like cell lymphoma. NKTCL are defined by their growth pattern and may have variable immunogenetic features.
NKTCL is far more prevalent in Asians and South Americans than in Western Europeans3. It classically presents as a midline facial destructive disease, previously known as lethal midline granuloma. The lymphoma may declare itself with a mass effect or more strikingly with palatal destruction, orbital swelling, and erythema9. Histologically, there is a polymorphic infiltration of atypical lymphocytes, and an angiocentric and angiodestructive growth pattern may be seen13. Immunohistochemistry shows the characteristic of NK cells. This disease is strongly associated with Epstein-Barr virus (EBV), which can be demonstrated in the great majority of cases by in situ hybridization studies with probes to EBVencoded small nuclear RNA139. In this case, histopathologic examination showed dense perivascular infiltration of atypical polymorphic lymphoid cells and extensive necrosis throughout the dermis. And the immunophenotypes belong to CD3-, CD4-, CD5-, CD8-, CD20-, CD45+, CD56+ and CD68-.
Aggressive NK/T-cell lymphoma/leukemia (ANKTCL) is a rather rare form of non-nasal NKTCL that is considered to be the leukemic form of the nasal type lymphoma9. Men and women are equally affected, at a median age in the third decade10. Systemic symptoms include significant weight loss, jaundice and high fever, and lymphadenopathy may be found with hepatosplenomegaly. Severe anemia and thrombocytopenia are common, due to direct infiltration or active hemophagocytosis in the marrow and occasional involvement of the peripheral blood21011. White blood cell count may be increased due to circulating neoplastic cells. Liver function derangement and features of disseminated intravascular coagulopathy are frequent2. ANKTCL pursues a highly aggressive course, resulting in death often within 6 weeks. Response to chemotherapy is poor and the curable potential of bone marrow transplantation remains unproven3569.
Clinically, ANKTCL is characterized by lymphoadenopathy, hepatosplenomegaly, presence of atypical lymphocytes with large azurophilic cytoplasmic granules in the peripheral blood, and partial involvement of the bone marrow. In this case, there were hepatosplenomegaly without peripheral lymphadenopathy, presence of atypical lymphoid cells with large azurophilic cytoplasmic granules in the peripheral blood and bone marrow.
Although ANKTCL is identical to extranodal NKTCL in histopathology (angiocentric pattern), immunophenotypic profile (CD2+, surface CD3-, cytoplasmic CD3ε+, CD56+), genotype (lack of TCR gene rearrangement), and strong association with EBV, it does show some distinguishing features; (1) the prominent systemic symptoms; (2) younger age at onset (mean 36 years); (3) presence of peripheral blood involvement; (4) widespread tissue involvement with marrow infiltration (nasal/extranasal NKTCL rarely disseminate even in terminal stage); (5) a fulminant disease course; and (6) very infrequent skin involvement356121314.
Among the 20 cases of non-nasal NKTCL reported in Korean dermatologic literature, none of them occurred in adolescence. So far only two cases of ANKTCL have been reported in Korean patients (Table 1)45. Compared to previous cases, this case is unique in that it occurred in a younger child. In previous cases, the skin lesions were localized in both thighs and the forearm, respectively. But in this case, the lesions were located in more extensive regions; the upper eyelid, neck and thigh. Including this case, all three cases showed invasion in the skin, bone marrow, liver and spleen.
We herein report a rare case of aggressive NK/T-cell lymphoma/leukemia with the cutaneous involvement in adolescence.
Figures and Tables
Fig. 1
Multiple, asymptomatic, deep-seated, erythematous nodules with central necrotic crusts on the left upper eyelid (A), neck (B) and left thigh (C).

Fig. 2
(A) Peripheral blood smear shows atypical immature cell (Wright, ×1,000). (B) Bone marrow biopsy shows infiltrations of hemophagocytic cells and atypical immature cell (Wright, ×1,000).
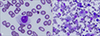
Fig. 3
(A) Dense polymorphous infiltrate with extensive necrosis throughout the dermis (H&E, ×40). (B) Perivascularly infiltrative atypical polymorphic lymphoid cells (H&E, ×400).

References
1. Chan JK, Sin VC, Wong KF, Ng CS, Tsang WY, Chan CH, et al. Nonnasal lymphoma expressing the natural killer cell marker CD56: a linicopathologic study of 49 cases of an uncommon aggressive neoplasm. Blood. 1997; 89:4501–4513.

2. Kwong YL. Natural killer-cell malignancies: diagnosis and treatment. Leukemia. 2005; 19:2186–2194.

3. Radonich MA, Lazova R, Bolognia J. Cutaneous natural killer/T-cell lymphoma. J Am Acad Dermatol. 2002; 46:451–456.

4. Kim JW, Kim KJ, Lee CJ. A case of aggressive T/NK-cell lymphoma/leukemia with cutaneous involvement. Korean J Dermatol. 2003; 41:1638–1643.
5. Choi YL, Park JH, Kim WS, Lee DY, Lee JH, Yang JM, et al. Aggressive NK-cell leukaemia associated with reactive haemophagocytic syndrome. Clin Exp Dermatol. 2005; 31:83–85.

6. Imamura N, Kusunoki Y, Kawa-Ha K, Yumura K, Hara J, Oda K, et al. Aggressive natural killer cell leukaemia/lymphoma: report of four cases and review of the literature. Possible existence of a new clinical entity originating from the third lineage of lymphoid cells. Br J Haematol. 1990; 75:49–59.

7. Ansai S, Maeda K, Yamakawa M, Matsuda M, Saitoh S, Suwa S, et al. CD56-positive (nasal-type T/NK cell) lymphoma arising on the skin: report of two cases and review of the literature. J Cutan Pathol. 1997; 24:468–476.
8. Russell-Jones R. World Health Organization classification of hematopoietic and lymphoid tissue: Implications for dermatology. J Am Acad Dermatol. 2003; 48:93–102.

9. Jaffe ES, Chan JK, Su IJ, Frizzera G, Mori S, Feller AC, et al. Report of the workshop on nasal and related extranodal angiocentric T/natural killer cell lymphomas: definitions, differential diagnosis, and epidemiology. Am J Surg Pathol. 1996; 20:103–111.

10. Kwong YL, Chan AC, Liang R, Chiang AK, Chim CS, Chan TK, et al. CD56+ NK lymphomas: clinicopathological features and prognosis. Br J Haematol. 1997; 97:821–829.
11. Suzuki R, Suzumiya J, Nakamura S, Aoki S, Notoya A, Ozaki S, et al. Aggressive natural killer-cell leukemia revisited: large granular lymphocyte leukemia of cytotoxic NK cells. Leukemia. 2004; (18):763–770.

12. Nava VE, Jaffe ES. The pathology of NK-cell lymphomas and leukemias. Adv Anat Pathol. 2005; 12:27–34.

13. Quintanilla-Martinez L, Jaffe ES. Aggressive NK cell lymphomas: insights into the spectrum of NK cell derived malignancies. Histopathology. 2000; 37:372–374.

14. Siu LL, Chan JK, Kwong YL. Natural killer cell malignancies: clinicopathologic and molecular features. Histol Histopathol. 2002; 17:539–554.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download