Abstract
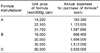
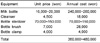
Although the advantages of breastfeeding, such as nutritional and immunologic support to the baby and improvement of emotional bonding between mother and baby, are well recognized, economic benefits of the breastfeeding are not emphasized. Breastfeeding help mothers save money to purchase breast milk substitutes and related equipments, such as bottles, nipples and sterilizers. It also reduces the incidences of common respiratory and gastrointestinal infection of babies, premenopausal breast cancer and ovarian cancer of mothers, and related hospital expenses. For employed mothers, a hospital visit due to illness of their babies can cause absence from their work places. For estimation of the economic advantages of breastfeeding in Korea, we surveyed the cost of the breast milk substitutes and related equipments. The yearly costs for the formulas were 763 thousand to 2.5 million wons, and for the equipment was 360 to 480 thousand wons. If the breastfeeding rate of the total population increased to 50%, 162-294 billion wons can be saved per year in this country by reducing the costs for the formula at the equipment. Total hospital expenses for the illness of babies can be reduced by 7.9-13.8 billion wons per year and hospital costs for maternal breast and ovarian cancers can be reduced by 24.8-57.7 billion wons per year. Durations of maternal absence from their work can be reduced to the value of 21.6-42.5 billion wons per year. In summary, by increasing breastfeeding rates in this country to 50%, 216.4-407.5 billion wons can be saved every year.
Figures and Tables
References
1. Montgomery DL, Splett PL. Economic benefit of breast-feeding infants enrolled in WIC. J Am Diet Assoc. 1997. 97:379–385.

2. Hoey C, Ware JL. Economic advantages of breast-feeding in an HMO setting: A pilot study. Am J Manag Care. 1997. 3:861–865.
3. Hyun T, Kim K, Kang N, Lim E. The economic benefits of breastfeeding. Korean J Community Nutr. 2002. 7:863–871.
4. Dewey KG, Heinig MJ, Nommsen-Rivers LA. Differences in morbidity between breast-fed and formula-fed infants. J Pediatr. 1995. 126(5 Pt 1):696–702.

5. Chen Y. Relationship between type of infant feeding and hospitalization for gastroenteritis in Shanghai infants. J Hum Lact. 1994. 10:177–179.

6. Howie PW, Forsyth JS, Ogston SA, Clark A, Florey CD. Protective effect of breast feeding against infection. BMJ. 1990. 300(6716):11–16.

7. Paricio Talayero JM, Lizán-García M, Otero Puime A, Benlloch Muncharaz MJ, Beseler Soto B, Sánchez-Palomares M, Santos Serrano L, Rivera LL. Full breast-feeding and hospitalization as a result of infections in the first year of life. Pediatrics. 2006. 118(1):e92–e99.

8. Ball TM, Wright AL. Health care costs of formula-feeding in the first year of life. Pediatrics. 1999. 103(4 Pt 2):870–876.

9. Leung GM, Lam TH, Ho LM, Lau YL. Health consequences of breast-feeding: doctors visits and hospitalizations during the first 18 months of life in Hong Kong Chinese infants. Epidemiology. 2005. 16:328–335.
10. Cattaneo A, Ronfani L, Burmaz T, Quintero-Romero S, Macaluso A, Di Mario S. Infant feeding and cost of health care: cohort study. Acta Paediatr. 2006. 95:540–546.
11. Bachrach VR, Schwarz E, Bachrach LR. Breastfeeding and the risk of hospitalization for respiratory disease in infancy: a meta-analysis. Arch Pediatr Adolesc Med. 2003. 157:237–243.

12. Shin NK, Park JH, Jun HR. Effect of feeding type on the morbidity of infants. J Korean Soc Matern Child Health. 1997. 1:145–156.
13. Quigley MA, Kelly YJ, Sacker A. Breastfeeding and hospitalization for diarrheal and respiratory infection in the United Kingdom Millennium Cohort Study. Pediatrics. 2007. 119:e837–e842.

14. Libster R, Bugna Hortoneda J, Laham FR, Casellas JM, Israele V, Polack NR, Delgado MF, Klein MI, Polack FP. Breastfeeding prevents severe disease in full term female infants with acute respiratory infection. Pediatr Infect Dis J. 2009. 28:131–134.

15. Chantry CJ, Howard CR, Auinger P. Full breastfeeding duration and associated decrease in respiratory tract infection in US children. Pediatrics. 2006. 117:425–432.

16. Yoon PW, Black RE, Moulton LH, Becker S. Effect of not breastfeeding on the risk of diarrheal and respiratory mortality in children under 2 years of age in Metro Cebu, The Philippines. Am J Epidemiol. 1996. 143:1142–1148.

17. Mårild S, Hansson S, Jodal U, Odén A, Svedberg K. Protective effect of breastfeeding against urinary tract infection. Acta Paediatr. 2004. 93:164–168.

18. Pisacane A, Graziano L, Mazzarella G, Scarpellino B, Zona G. Breast-feeding and urinary tract infection. J Pediatr. 1992. 120:87–89.

19. Moreland J, Coombs J. Promoting and supporting breast-feeding. Am Fam Physician. 2000. 61:2093–2100. 2103–2104.
20. Ministry of Health and Welfare. Planned Population Federation of Korea. A Survey of the actual state of breastfeeding. 2005. Soeul, Korea: Planned Population Federation of Korea.
21. Newcomb PA, Storer BE, Longnecker MP, Mittendorf R, Greenberg ER, Clapp RW, Burke KP, Willett WC, MacMahon B. Lactation and a reduced risk of premenopausal breast cancer. N Engl J Med. 1994. 330:81–87.

22. Korean Breast Cancer Society. Breast cancer facts & figures, 2006-2008. 2008. Seoul, Korea: Korean Breast Cancer Society.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download