Abstract
This study was performed to identify hypertension outpatients' motivations in choosing healthcare providers i.e. tertiary hospitals, general hospitals (number of bed is more than or equal to 100), hospitals (number of bed is more than or equal to 30), and clinics for their care management and find the determinants influencing on their choice of healthcare providers. The unit of analysis was a hypertension outpatient visit (n=11,046). The χ2-test was performed to find the differences in choices of healthcare providers by patient characteristics. Additionally, ANOVA was employed to identify differences in out-of-pocket medical and medication costs by the type of provider. The 4 types of healthcare providers were then categorized into two levels (1=hospitals, 2=clinics), and finally, logistic regression analysis was performed to find factors influencing the patients' clinic visit for their care. Of the 11,046 cases, 82.9 percent of patients visited clinics for their care. The medical and medication out-of-pocket costs per case were the highest among the tertiary hospitals followed by general hospitals, hospitals, and clinics. Lower income and less education were associated with a higher frequency of clinic visits. The patients with National Health Insurance were more likely to visit clinics for their care than medicaid patients. Patients with any comorbidity or disability were more likely to visit hospitals than patients without them. Patients taking any medical test were more likely to visit hospitals than those who were not. Patients with a medication prescription were more likely to visit clinics than those without. Not only for cost-containment to maintain a sound healthcare financing system, but also to reduce the burden of hypertension patients' out-of-pocket costs, policy-makers should pay more attention to encouraging chronic patients to visit clinics rather than hospitals for their care management.
Figures and Tables
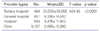
Table 5
Logistic regression results of factors related to hypertension patients' clinic visita)

Likelihood ratio test, -2 Log L=10,106.81; X2=1,375.49, p<0.0001.
OR: odds ratio, CI: confidence interval.
a)Results were adjusted for all other independent variables of Table 2.
b)Others include private car, taxi, public transportation, airplane, train, etc.
References
1. Coleman K, Austin BT, Brach C, Wagner EH. Evidence on the chronic care model in the new millennium. Health Aff (Millwood). 2009. 28:75–85.

2. Son KA, Kim YS, Hong MH, Jeong MA. Analysis of the continuity of outpatient among adult patients with hypertension and its influential factors in Korea. J Korea Academia-Ind Coop Soc. 2010. 11:2161–2168.

3. Result of hypertension patient analysis [Internet]. National Health Insurance Corporation. c2009. cited 2011 Aug 15. Seoul: National Health Insurance Corporation;Available from: http://www.nhic.or.kr/portal/site/main/menuitem.31f14893bf4f6c38b31148b4062310a0.
4. Choi YS, Lee JS, Moon SW, Han JT, Beck SJ, Koh YK. Development of model project program for usual medical provider registration of chronic disease. 2009. Seoul: National Health Insurance Corporation.
5. Lee JH. Implementation for managing chronic diseases. 2009. Seoul: The Catholic University of Korea School of Medicine.
6. Lee HY, Joeng HJ, Seo NK, Moon SW, Koh Y. The introduction of integrated system unifying the insurance system. 2009. Seoul: National Health Insurance Corporation.
7. Jeong SH. Management for chronic diseases of clinics. 2009. Seoul: Health Insurance Review and Assessment Service.
8. Ministry of Health and Welfare, KR. Plan of standard role and functions by classification of medical institutions. 2011. Seoul: Ministry of Health and Welfare.
9. Myung JI, Jeong YC. An analysis of the effects of health care delivery system. 1991. Seoul: The Korea Institute for Health and Social Affairs.
10. Furrow BR, editor. Health law. 1995. St Paul, MN: West Publishing.
11. Song KY. Developement of standard role and functions by classification of medical institutions. 2001. Seoul: Ministry of Health and Welfare.
12. Kang BS. Preventive medicine and public health. 2002. Seoul: Kye Chuk.
13. Park BH. A direction of health policy for primary care activation. J Korean Acad Fam Med. 1999. 20:953–958.
14. Kim J, Kim H, Kim H, Min KW, Park SW, Park IB, Park JH, Baik SH, Son HS, Ahn CW, Oh JY, Lee S, Lee J, Chung CH, Choi KM, Choi I, Kim DJ. Current status of the continuity of ambulatory diabetes care and its impact on health outcomes and medical cost in Korea using National Health Insurance database. J Korean Diabetes Assoc. 2006. 30:377–387.

15. Ibrahim MA, Savitz LA, Carey TS, Wagner EH. Population-based health principles in medical and public health practice. J Public Health Manag Pract. 2001. 7:75–81.

16. Norris SL, Glasgow RE, Engelgau MM, O'Connor PJ, McCulloch D. Chronic disease management: a definition and systematic approach to component interventions. Dis Manag Health Outcomes. 2003. 11:477–488.
17. Cho KH, Hong MH. The study of disease structure and utilization of health care facility in the elderly. J Korean Acad Fam Med. 1997. 18:824–843.
18. Youn KI, Doh SR. An analysis of the diseases specific medical service organization selection factors of patients. Korean J Hosp Manage. 2007. 12:1–21.
19. Jang S, Park C, Jang S, Yoon HK, Shin CS, Kim DY, Ha YC, Lee SS, Choi HJ, Lee YK, Kim BT, Choi JY. Medical service utilization with osteoporosis. Endocrinol Metab. 2010. 25:326–339.

20. Kim YK. Analysis of factors affecting the level of regional medical utilization. 1995. Seoul: Yonsei University The Graduate School of Public Health.
21. Hjortdahl P, Laerum E. Continuity of care in general practice: effect on patient satisfaction. BMJ. 1992. 304:1287–1290.

22. Weissman JS, Stern R, Fielding SL, Epstein AM. Delayed access to health care: risk factors, reasons, and consequences. Ann Intern Med. 1991. 114:325–331.

23. Hurley RE, Gage BJ, Freund DA. Rollover effects in gatekeeper programs: cushioning the impact of restricted choice. Inquiry. 1991. 28:375–384.
24. Smith SR, Kirking DM. Access and use of medications in HIV disease. Health Serv Res. 1999. 34:123–144.
25. Newschaffer CJ, Zhang D, Hauck WW, Fanning T, Turner BJ. Effect of enhanced prenatal and HIV-focused services for pregnant women who are infected by human immunodeficiency virus on emergency department use. Med Care. 1999. 37:1308–1319.

26. Weiss LJ, Blustein J. Faithful patients: the effect of long-term physician-patient relationships on the costs and use of health care by older Americans. Am J Public Health. 1996. 86:1742–1747.

27. Park JH, Kim KW, Sung NJ, Choi YG, Lee JH. Association between primary care quality and health behaviors in patients with essential hypertension who visit a family physician as a usual source of care. Korean J Fam Med. 2011. 32:104–111.

28. He J, Muntner P, Chen J, Roccella EJ, Streiffer RH, Whelton PK. Factors associated with hypertension control in the gene-ral population of the United States. Arch Intern Med. 2002. 162:1051–1058.

29. McCombs JS, Nichol MB, Newman CM, Sclar DA. The costs of interrupting antihypertensive drug therapy in a Medicaid population. Med Care. 1994. 32:214–226.

30. Xu KT. Usual source of care in preventive service use: a regular doctor versus a regular site. Health Serv Res. 2002. 37:1509–1529.

31. Oh HJ, Park JS, Park AR, Pyun SW, Kim YK. A study on revitalization of primary healthcare organizations through development of standard functions. J Korean Med Assoc. 2011. 54:205–216.

32. Kim YK, Kim JS. A study on healthcare institution selection of healthcare consumers using theory of consumption values: focusing on relations among clinics or small sized hospitals, general hospitals, and large-sized hospitals. J Korean Soc Quality Manage. 2009. 37:71–86.
33. Shin YS. On the appropriate use of health services. Health Welf Policy Forum. 2006. (114):91–101.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download