Abstract
Primary care lays the foundation of national healthcare systems, but it has been weak in playing its role correctly because of legal and environmental attributes surrounding the healthcare industry in Korea. This study is conducted to concretize the definition and scope of primary care and to deduce its standard functions to contribute to establishing the healthcare delivery system and appropriate healthcare systems embracing socio-environmental leverage. The term primary healthcare institution was adopted based on literature review to achieve the research goal. The principle diseases appropriate for the primary healthcare institution based on ambulatory care sensitive conditions were analyzed, and the standard functions were deduced by matching these diseases with current procedural terminologies using CrossCoder package. Based on the analysis, the primary healthcare institution-specific diseases were 53 specific diseases under 23 broad disease groups. The standard functions were deduced in three categories of the standard functions of the entire primary healthcare institutions with 100% frequency, common standard functions with 70% frequency, and peculiar standard functions specific to diseases or body systems. These functions included outpatient evaluation and measurement, various factor tests through blood collection, and X-ray. Establishing the standard functions for the primary healthcare institution can promote patient reliability on primary care, alleviate health demand congestion toward large-sized advanced healthcare institutions. Furthermore, it contributes to establishing and reinforcing other healthcare policies related to the healthcare reimbursement system and referral system, and fosters primary care physician education. Most importantly, it reduces the national health expenditures by realizing efficient and effective healthcare delivery.
Primary care is essential healthcare, which is the foundation of national healthcare systems, and is the initial health services provided in the general healthcare delivery system. It is an efficient measure to alleviate or resolve the majority of health needs of the entire population, and has the capability of inducing rational decision from consumers by acting as a gatekeeper to the healthcare delivery system. Furthermore, primary care can substantially contribute to reducing the national health expenditures by curbing unnecessary usage of health services. According to preceding studies on the effect of primary care on the patient and society as a whole, the attributes of primary care have been explored mainly to reduce unnecessary hospitalization, enhance patient satisfaction, and lead to reduced healthcare expenditures. Dixon et al.[1] argued that comprehensive services in healthcare decrease hospitalization and operation rates that lead to increased patient satisfaction. According to Grumbach and Fry [2], maintaining sustainability reduced preventable hospitalization. Meanwhile, the ability to coordinate and arbitrate in terms of healthcare among primary care physicians was found to reduce unneeded medical examinations and treatment volumes, and actively determine specific health problems of patients [3].
It is also widely disclosed to the public in Korea that a large gap of medical fees exists depending on the scale and type of healthcare institutions. The size of medical bills charged to patients is the largest among tertiary specialized general hospitals followed by general hospitals, hospitals, and clinics. Although this gap varies depending on the groups and categories of diseases, the size of medical bills charged by the tertiary specialized general hospitals is reported as up to three times higher than that of clinics for a given identical disease. This difference was often due to a variation in resource consumption in the diagnosis process [4]. Not only is primary care capable of rationalizing the national healthcare and contributing to fair resource allocation, it is also capable of enhancing the efficiency of the overall healthcare systems.
Despite such importance, primary care in Korea has not been playing its role in the national healthcare correctly while losing its vitality because the healthcare delivery system is not solidly established and the functions and roles of different types of healthcare institutions are not clearly defined in Korea. Under the current structure, primary, secondary, and tertiary healthcare institutions all perform identical health services, and thus the relationship among these institutions has turned competitive for attracting own customers, patients in this case, rather than complementary. Because of this environmental change, primary care in Korea ended up having weak authority and isolation as its attributes, and thus it has not been able to realize its merits. Consequently, this phenomenon has caused inefficient healthcare resource allocation and an increase in the national health expenditures, and has ultimately hindered the benefit of healthcare users.
Therefore, this study is conducted to concretize the definition and scope of care of primary care, which is one of the core components and gatekeeper of national health, and deduce its standard functions so that we may be one step closer to firmly establishing the healthcare delivery system and appropriate healthcare systems, which embrace socio-environmental changes and leverage in Korea.
Although the term primary care is often cited and used in today's society, its definition as well as its origin cannot be found in the epidemiological dictionary or in the related literatures. A wide spectrum to investigate what is truly primary care exists even to date. The World Health Organization (WHO) and United Nations Children's Fund (UNICEF) defined primary through the Alma Ata international conference in 1978 as essential healthcare based on practical, scientifically sound and socially acceptable methods and technology made universally accessible to individuals and families in the community through their full participation and at a cost that the community and the country can afford to maintain at every stage of their development in the spirit of self-determination [5]. Afterward, primary care was accepted by the member countries of WHO as the key to achieving the goal of health for all.
Meanwhile, the US Institute of Medicine (IoM) defined primary care as the provision of integrated, accessible health care services by clinicians who are accountable for addressing a large majority of personal health care needs, developing a sustained partnership with patients, and practicing in the context of family and community [6]. This definition viewed primary care a distinct function. In other words, although particular groups of healthcare providers such as general practitioners and family physicians exist on the dimension of primary care, it is a function rather than a specific medical area or a specialty.
In Korea, the definition of primary care varies to a great degree. It is defined simply as health services provided mainly focusing on outpatients in some laws or regulations, while also defined as basic or general health services provided to an individual who requires healthcare when initially contacting the medical professional in other related laws or regulations. These are further discussed later in the study.
Establishing appropriate healthcare systems and health services delivery system requires suggesting functions specific to different types of healthcare institutions based on diseases and conditions of each patient. Various healthcare laws and legislation are reviewed, which lay the foundation of this study.
First, a parent law, which controls all of the healthcare institutions in Korea, is healthcare law, and these institutions are established under the article 3 clause 1 of the law. It does not, however, define primary, secondary, and tertiary care. Rather, healthcare institutions are classified into four types of clinic, hospital, general hospital, and specialized general hospital under the law. According to the law, cliniclevel institutions are the ones that provide health services mainly focusing on outpatients. These institutions are approved by mayor, county governor (Gunsu) or chief of a borough (Gu) at the time of establi-shment. These are shown in Table 1.
Second, national health insurance law, on the contrary, stipulates two types of health insurance coverage, which are level 1 health insurance coverage and level 2 health insurance coverage under article 2. Level 1 is received from healthcare institutions other than specialized general hospitals. Level 2 is received only from specialized general hospitals. When policy holders wish to receive health services at level 2 healthcare institutions, they must obtain doctor's referral accompanied by required documents. This stipulation concerns the referral process in the healthcare system.
Third, healthcare insurance coverage law for basic living subsidies classifies healthcare institutions into three types of primary, secondary, and tertiary healthcare institutions under the article 9 clause 2. Under the law, the scope of health services provided by primary healthcare institutions is as follows.
1) Care of diseases requiring basic surgical procedures and other outpatient treatment
2) Care of diseases excluding diseases requiring long-term treatment and hospitalization
3) Emergency care for patients only if, considering the disease condition and transfer distance, transferring the patient to another healthcare institution may threaten the patient's life
4) Care of patients referred from other secondary or tertiary healthcare institutions.
The law also stipulates that primary healthcare institutions can refer their patients to secondary healthcare institutions.
In summary, healthcare laws and regulations for different types of healthcare providers and institutions adopt discordant classification methods. In the healthcare law, hospital and general hospital share very similar attributes except for the requirements and approval authorities of initial establishment. In the national health insurance law, only two classifications are stipulated and the definition and scope of healthcare institutions are ambiguous. In the healthcare insurance coverage law, healthcare institutions are classified into three types, which share similar attributes stipulated in the healthcare law. Moreover, the definition, scope, approval authorities, and referral processes are clearly stipulated.
The ultimate purpose of this study is to deduce and suggest standard functions of primary healthcare institutions based on concrete definition and scope of care. Based on literature review, we were very careful in establishing the definition and scope of primary care, and determined that the term primary healthcare institution is more appropriate than primary care to analyze the appropriate diseases and standard functions of primary care in Korea. Therefore, the term primary healthcare organization is used henceforth.
According to the scope of primary care presented by WHO, UNICEF, US IoM, and healthcare legislation in Korea, principle diseases appropriate for the primary healthcare institution can be characterized by those diseases and conditions caused by individual lifestyle that do not require hospitalization when treated properly. Based on this scope of the primary healthcare institution, lifestyle diseases suggested by MedicineNet in the US and chronic non-communicable diseases (NCD) suggested by the Western Pacific Region are first adopted in this study. Lifestyle diseases are diseases that appear to increase in frequency as countries become more industrialized and people live longer, and these diseases are associated with the way a person or group of people lives [7]. For chronic NCDs, these are non-contagious diseases with risk factors such as a person's lifestyle, genetics, or environment known to increase the likelihood of certain non-communicable diseases [8]. In other words, the lifestyle diseases and chronic NCDs are diseases developed mainly due to primitive factors not requiring such heavy and advanced healthcare technologies provided typically through the tertiary healthcare institution. Since the primary healthcare institution is defined as playing the role of a gatekeeper to the national healthcare system, these diseases were first determined to be appropriate for the primary healthcare institution in Korea.
Subsequently, we discovered through a comprehensive literature review that diseases do not require hospitalization when treated properly, which is the second characteristic of the diseases appropriate of the primary healthcare institution in Korea, are connected directly with ambulatory care sensitive conditions (ACSC). ACSCs are a group of diagnoses that are related to access to good primary care and medical problems that are potentially preventable. ACSCs were analyzed as encompassing lifestyle diseases and chronic NCDs discussed above, and are studied and suggested by the Agency for Healthcare Research and Quality (AHRQ) under the Centers for Medicare & Medicaid Services of the US Department of Health & Human Services each year [9]. Therefore, these ACSCs, due to their comprehensiveness of lifestyle diseases and chronic NCDs, are finally reviewed and analyzed in order to deduce and suggest the diseases appropriate for the primary healthcare institution in Korea in this study.
After the diseases appropriate for the primary healthcare institution in Korea were analyzed, we initially obtained International Classification of Diseases (ICD) 9 codes relevant to each of the specific diseases in order to deduce the standard functions of the primary healthcare institution in Korea. In order to deduce these standard functions, we corresponded and matched these ICD 9 codes-based diseases with Current Procedural Terminologies (CPT). CPT code set is maintained by the American Medical Association (AMA) through the CPT editorial panel, and it accurately describes medical, surgical, and diagnostic services and is designed to communicate uniform information about medical services and procedures among physicians, coders, patients, accreditation organizations, and payers. Physicians may perform various medical procedures on patients with specific medical problems and conditions. Among these many procedures performed by the physician, US Medicare only reimburses particular procedures approved and assigned with CPT codes. Because of the nature of CPT, these terminologies may be understood as a series of standard procedures for specific diseases. In this study, CPTs for the deduced primary healthcare-specific diseases were considered standard functions of the primary healthcare institution in Korea. The matching process between ICD 9 and CPT was performed by using the CrossCoder package acquired through Wasserman Medical Publishers. For example, a disease with the ICD 9 code xxx.x was analyzed in this study as a disease appropriate for the primary healthcare institution in Korea. Subsequently, we would use the CrossCoder package to input the ICD 9 above, and extract the corresponding CPTs. These CPTs stipulate specific procedures such as xxx test, examination of xxx, and injection of xxx. We would finally suggest the CPTs deduced from the process above to be the standard functions of the primary healthcare institution in Korea.
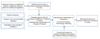
We reviewed the international and domestic literatures available on healthcare systems, healthcare delivery system, health care legislation, and diseases appropriate for different types of healthcare institutions. Based on the literature review, we analyzed the specific diseases appropriate for the primary healthcare institution in Korea and corresponding standard functions. The research flow and framework are illustrated in Figure 1.
The primary healthcare institution-specific diseases were analyzed to be total 53 specific diseases under 23 broad disease groups or categories. First, the 23 disease groups analyzed included the following: immunization-related and preventable conditions, grand mal status and other epileptic convulsions, convulsions, ear, nose, and throat infections, pulmonary tuberculosis, other tuberculosis, chronic obstructive pulmonary disease, bacterial pneumonia, asthma, congestive heart failure, hypertension, angina, cellulitis, diabetes A, diabetes B, diabetes C, hypoglycemia, gastroenteritis, kidney/urinary infection, dehydration-volume depletion, iron deficiency anemia, failure to thrive, and pelvic inflammatory disease.
Second, the specific diseases appropriate for the primary healthcare institution for the 23 disease groups or categories were analyzed as follows. For disease group 1 immunization-related and preventable conditions, whooping cough due to bordetella pertussis, tetanus, acute paralytic poliomyelitis specified as bulbar unspecified type of poliovirus, hemophilus meningitis, and acute rheumatic pericarditis were analyzed. For disease group 2 grand mal status and other epileptic convulsions, generalized nonconvulsive epilepsy without intractable epilepsy was analyzed. For disease group 3 convulsions, febrile convulsions (simple) unspecified was analyzed. For disease group 4 ear, nose, and throat infections, acute suppurative otitis media without spontaneous rupture of eardrum, acute pharyngitis, acute tonsillitis, acute laryngopharyngitis, and chronic pharyngitis were analyzed. For disease group 5 pulmonary tuberculosis, tuberculosis of lung infiltrative confirmation unspecified was analyzed. For disease group 6 other tuberculosis, tuberculous pleurisy confirmation unspecified, tuberculous meningitis unspecified examination, tuberculous peritonitis unspecified examination, tuberculosis of vertebral column unspecified examination, tuberculosis of kidney unspecified examination, tuberculosis of skin and subcutaneous cellular tissue unspecified examination, and acute miliary tuberculosis unspecified examination were analyzed. For disease group 7 chronic obstructive pulmonary disease, acute bronchitis was analyzed. For disease group 8 bacterial pneumonia, pneumococcal pneu-monia, pneumonia due to hemophilus influenza, pneumonia due to streptococcus unspecified, bacterial pneumonia unspecified, pneumonia due to mycoplasma pneumonia, bronchopneumonia organism unspecified, and pneumonia organism unspecified were analyzed. For disease group 9 asthma, extrinsic asthma unspecified was analyzed. For disease group 10 congestive heart failure, congestive heart failure unspecified, benign hypertensive heart disease with heart failure, and acute edema of lung unspecified were analyzed. For disease group 11 hypertension, unspecified essential hypertension and benign hypertensive heart disease without heart failure were analyzed. For disease group 12 angina, intermediate coronary syndrome and angina decubitus were analyzed. For disease group 13 cellulitis, unspecified cellulitis and abscess of finger and cellulitis and abscess of face were analyzed. For disease group 14 diabetes A, diabetes with ketoacidosis type II or unspecified type not stated as uncontrolled and diabetes with hyperosmolarity type II or unspecified type not stated as uncontrolled were analyzed. For disease group 15 diabetes B, diabetes with other specified manifestations type II or unspecified type not stated as uncontrolled and diabetes with unspecified complication type II or unspecified type not stated as uncontrolled were analyzed. For disease group 16 diabetes C, diabetes mellitus without mention of complication type II or unspecified type not stated as uncontrolled was analyzed. For disease group 17 hypoglycemia, hypoglycemia unspecified was analyzed. For disease group 18 gastroenteritis, other and unspecified noninfectious gastroenteritis and colitis was analyzed. For disease group 19 kidney/urinary infection, chronic pyelonephritis without lesion of renal medullary necrosis, urinary tract infection site not specified, and unspecified disorder of urethra and urinary tract were analyzed. For disease group 20 dehydration-volume depletion, volume depletion unspecified was analyzed. For disease group 21 iron deficiency anemia, iron deficiency anemia secondary to inadequate dietary iron intake and iron deficiency anemia unspecified were analyzed. For disease group 22 failure to thrive, unspecified lack of normal physiological development was analyzed. Last, for disease group 23 pelvic inflammatory disease, acute salpingitis and oophoritis was analyzed. These results are shown in Table 2.
Standard functions of the primary healthcare institution were deduced in three categories including the standard functions of the entire primary healthcare institutions with 100% frequency, common standard functions with 70% frequency, and peculiar standard functions (specific to diseases or body systems). First, the standard functions of the entire primary healthcare institutions with 100% frequency are the functions that every primary healthcare institution is recommended to perform. The first set of these standard functions includes evaluation and measurement of outpatients. The scope of the activities is as follows.
1) Evaluation and measurement based on problem-focused history, problem-focused examination, and simple medical decision making
2) Evaluation and measurement based on detailed history, detailed examination, and moderately complex medical decision making
3) Evaluation and measurement based on comprehensive history, comprehensive examination, and highly complex medical decision making
When performing the evaluation and measurement above, the primary healthcare physician is required to perform at least 2 items in each scope. The second set of the standard functions for the entire primary healthcare institutions are specific tests and examinations including collection of venous blood by venipuncture, hepatic function panel, basic metabolic panel, smear, infectious agent antigen detection, culture, urinalysis, renal function panel, electrolyte panel, comprehensive metabolic panel, lipid panel, blood count, homocysteine level (serum), collection of capillary blood specimen (e.g., finger, heel, ear stick), and X-ray. Although many of the primary healthcare institutions in Korea currently may conduct such tests and examinations internally but receive corresponding results externally from other secondary or tertiary healthcare institutions, clinics specializing in conducting and analyzing these tests and exams do exist in Korea. Therefore, the entire primary healthcare institutions are recommended to perform these standard functions as shown in Table 3.
Second, the common standard functions with 70% frequency are the functions not for the entire primary healthcare institutions but suitable for about 70% of the population. These common standard functions include injection (for whooping cough due to bordetella pertussis, tetanus, generalized nonconvulsive epilepsy without intractable epilepsy, febrile convulsions (simple) unspecified, acute suppurative otitis media without spontaneous rupture of eardrum, acute laryngopharyngitis, chronic pharyngitis, acute bronchitis, bacterial pneumonia unspecified, extrinsic asthma unspecified, congestive heart failure unspecified, benign hypertensive heart disease with heart failure, acute edema of lung unspecified, unspecified essential hypertension, benign hypertensive heart disease without heart failure, intermediate coronary syndrome, angina decubitus, unspecified cellulitis and abscess of finger, cellulitis and abscess of face, diabetes with unspecified complication type II or unspecified type not stated as uncontrolled, diabetes mellitus without mention of complication type II or unspecified type not stated as uncontrolled, other and unspecified noninfectious gastroenteritis and colitis, chronic pyelonephritis without lesion of renal medullary necrosis, urinary tract infection site not specified, unspecified disorder of urethra and urinary tract, volume depletion unspecified, iron deficiency anemia secondary to inadequate dietary iron intake, and iron deficiency anemia unspecified) and allergy testing and immunotherapy (for acute pharyngitis, acute tonsillitis, and acute bronchitis) as shown in Table 4.
Last, the peculiar standard functions are only specific to diseases or body systems including pulmonary function testing for respiratory diseases and vestibular and audiologic function tests for ear, nose, andthroat-related diseases. Because of the nature of these standard functions, such tests and exams may get some attention by the primary healthcare physicians but have been analyzed as insignificant to be standard functions for the primary healthcare insti-tution in Korea.
The initiation of the national health insurance and a rise in the national economic power have increased national healthcare needs and expectations. Consequently, this phenomenon has led the healthcare industry to rapidly grow. However, this growth of the industry has resulted in the decline and functional distortion of primary care that plays a central role in the national health system simultaneously. Large-sized hospitals, reflecting a substantial increase in number over the last decade, are leading the industry today, and the majority of primary healthcare institutions that accounted for over 80% of the entire demand in healthcare in the past are falling behind in the competition. With these environmental changes in mind, we conducted this study to ultimately deduce the standard functions of the primary healthcare institutions so that the findings of this study may contribute to revitalizing primary care and re-establishing the healthcare systems and healthcare delivery system in Korea.
Based on the results of this study, the following implications are presented. First, in order to coincide with the principles laying the foundation of healthcare laws and regulations in Korea that clinic-level (primary) healthcare institutions focus on outpatient services while hospital-level healthcare institutions focus on inpatient services, reform of the current healthcare delivery system is imperative in the long-term. Designating diseases and standard functions appropriate for the primary healthcare institution has potential to empower these institutions, to promote patient reliability on primary care, and to alleviate health demand congestion toward large-sized advanced healthcare institutions.
Second, establishing the standard functions for the primary healthcare institution can contribute to establishing and reinforcing other healthcare policies. These policies may concern relative values and conversion factors for health services provided in the healthcare reimbursement systems or referring and transferring patients to appropriate healthcare institutions within the healthcare system under the health referral systems.
Third, the diseases appropriate for the primary healthcare institutions suggested in this study are mainly preventive and managerial diseases. One of the essential causes of the decline of the primary healthcare institution is proper and sustainable training and education of primary healthcare physicians. By establishing appropriate diseases and standardized functions of the primary healthcare institution, the quality of these physicians will further be enhanced so that they can better serve in the national healthcare systems efficiently and effectively.
Fourth, not only does deducing the standard functions have implications valid for policy making, but it also has valuable implications for the people in Korea. By providing health services appropriate for specific diseases and conditions of individual patients based on appropriate disease classification and standard functions, the national health expenditures can be significantly decreased to lighten the burden off our citizens. The standard functions can eliminate unnecessary health services provided, and induce efficient and effective services in the healthcare delivery system. After all, the standard functions for the primary healthcare institution is not about mere money, it is about contributing to the better national healthcare.
Finally, this study retains the following research limitations. The diseases appropriate for the primary healthcare institution in this study were deduced based on lifestyle diseases, chronic non-communicable diseases, and ambulatory care sensitive conditions. Although the scope and applicability of these diseases have been examined and verified, these diseases were initially suggested in the western context and thus their applicability in the Korean context may cause disputes. Therefore, the diseases analyzed in this study shall be further examined by clinical panels from a clinical perspective and in the Korean context. Furthermore, these diseases were deduced without consideration of severity of each specific disease and condition. Therefore, further research with these factors taken into account is recommended in the future.
Figures and Tables
References
1. Dixon J, Holland P, Mays N. Primary care: core values developing primary care: gatekeeping, commissioning, and managed care. BMJ. 1998. 317:125–128.

2. Grumbach K, Fry J. Managing primary care in the United States and in the United Kingdom. N Engl J Med. 1993. 328:940–945.

3. Moore SH, Martin DP, Richardson WC. Does the primary-care gatekeeper control the costs of health care? Lessons from the SAFECO experience. N Engl J Med. 1983. 309:1400–1404.

4. Jeong EK, Moon OR, Kim CY. A study on the practice variations according to physician characteristics. Korean J Prev Med. 1993. 26:614–627.
5. World Health Organization. United Nations Children's Fund. Declaration of Alma-Ata [Internet]. c2010. cited 2010 Jun 10. Geneva: World Health Organization;Available from: http://www.who.int/hpr/NPH/docs/declaration_almaata.pdf.
6. Institute of Medicine of the National Academies. Defining primary care: an interim report. 1994. Washington: Institute of Medicine of the National Academies.
7. Lifestyle diseases [Internet]. MedicineNet. c2010. cited 2010 Jun 1. San Clemente, CA: MedicineNet;Available from: http://www.medicinenet.com/script/main/hp.asp.
8. World Health Organization, Western Pacific Region. Chronic noncommunicable disease [Internet]. c2010. cited 2010 Jun 1. Manila: World Health Organization, Western Pacific Region;Available from: http://www.wpro.who.int/health_topics/chronic_disease.
9. Agency for Healthcare Research and Quality. Ambulatory care sensitive conditions [Internet]. c2010. cited 2010 Jun 1. Rockville, MD: Agency for Healthcare Research and Quality;Available from: http://www.ahrq.gov/.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download