Abstract
Portal hypertension can arise from any condition interfering with normal blood flow at any level within the portal system. Herein, we presented two uncommon cases of the portal hypertension and its treatment with brief literature review. A 71-year-old man who underwent right hemihepatectomy revealed a tumor recurrence adjacent to the inferior vena cava (IVC). After radiofrequency ablation (RFA) with lymph node dissection, he was referred for abdominal distension. The abdomen computed tomography scan showed severe ascites with a narrowing middle hepatic vein (MHV) and IVC around the RFA site. After insertion of two stents at the IVC and MHV, the ascites disappeared. Another 73-year-old man underwent right trisectionectomy of liver and segmental resection of the portal vein (PV). After operation, he underwent conservative management due to continuous abdominal ascites. The abdomen computed tomography scan showed severe ascites with obliteration of the left PV. After insertion of stent, the ascites disappeared. A decrease of the pressure gradient between the PV and IVC is one of the important treatment strategies for portal hypertension. Vascular stent is useful in the reduction of pressure gradient and thus, can be a treatment option for portal hypertension.
Portal hypertension is a common clinical syndrome that is characterized by an increased portal pressure gradient. It causes an increased pressure gradient between the portal vein (PV) and the inferior vena cava (IVC) to above normal values (1-5 mmHg). Portal hypertension causes varices within the gastrointestinal tract and can lead to gastrointestinal bleeding with abdominal ascites, diffuse abdominal pain, diarrhea and hepatic dysfunction.123 Chronic liver disease is the most common cause of portal hypertension.1 However, portal hypertension has various rare causes.2 Herein, we presented two uncommon cases of the portal hypertension and its treatment with a brief literature review.
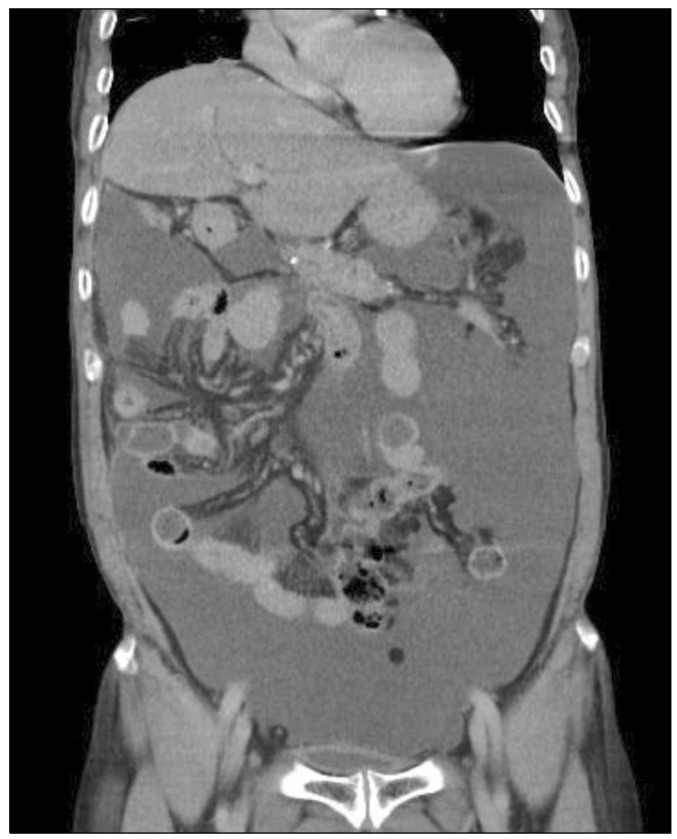
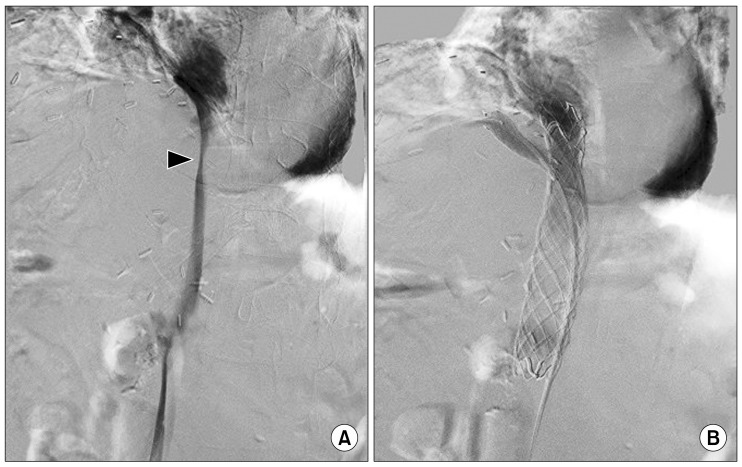
A 71-year-old man who underwent right hemihepatectomy one year prior due to combined hepatocellular and cholangiocarcinoma was found with elevated CA19-9 level of 60.2 U/ml at the follow-up examination. The imaging studies revealed tumor recurrence in the resection margin that was adjacent to the inferior vena cava (IVC) with an enlarged metastatic lymph node (LN) at the hepatoduodenal area. We performed radiofrequency ablation (RFA) with LN dissection due to severe adhesion between the tumor and IVC. Pathologic examination confirmed metastatic carcinoma derived from the previous cancerous lesion. Two weeks after discharge, he was referred to the emergency room for abdominal distension. Laboratory tests showed hypoalbuminemia (2.7 g/dl) and prolonged prothrombin time (PT) (1.24 INR). Although the ascitic fluid was slightly turbid, serum-to-ascites albumin gradient was 1.3 g/dl suggesting transudate ascites. The abdomen computed tomography (CT) scan showed severe ascites with a narrowing of the middle hepatic vein (MHV) and IVC around the RFA site (Fig. 1). The pressure gradient on IVC venography measured 11 mmHg between the IVC and MHV (Fig. 2A). After insertion of 2 stents at the IVC and MHV, the pressure gradient was decreased to 3 mmHg (Fig. 2B). The patient was discharged home on the fifteenth day with disappearance of ascites.
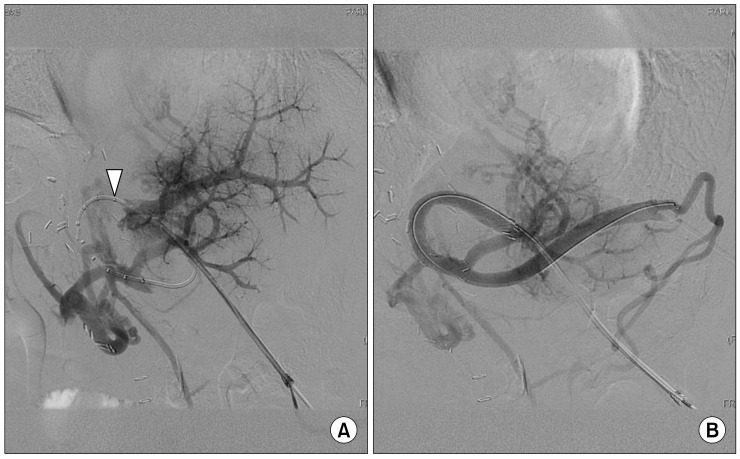
A 73-year-old man underwent right trisectionectomy of the liver after portal vein embolization due to gallbladder cancer with hepatic duct invasion. Portal vein (PV) segmental resection was performed intra-operatively because of adhesion between PV around the hilum and tumor. Pathologic examination confirmed chronic inflammation and metaplasia of gallbladder. After operation, he underwent conservative management at the outpatient department for several months due to continuous abdominal ascites and pleural effusion. Six months after the operation, he visited the emergency room due to melena and dizziness. Laboratory tests showed anemia (7.8 g/dl), thrombocytopenia (99 k/ul), hypoalbuminemia (2.2 g/dl) and prolonged PT (1.36 INR). Ascitic fluid was clear and serum-to-ascites albumin gradient was 1.9 g/dl. The abdomen CT scan showed severe ascites and pleural effusion with an oblation of the left PV (Fig. 3). Colonoscopy indicated bleeding at the ascending colon. Small bowel capsule endoscopy was performed to identify an accurate bleeding focus without success. In addition, PV stent insertion was performed in order to prevent varix bleeding and control the portal hypertension-induced ascites and pleural effusion. The pressure gradient on venography measured 11 mmHg between the left PV and splenic vein (Fig. 4A). After insertion of a stent at the LPV, the pressure gradient was decreased to 2 mmHg (Fig. 4B). The patient was discharged home on the twelfth day on recovery from ascites and melena.
Portal hypertension can arise from any condition that interferes with normal blood flow at any level within the portal system.123 Among these, hepatic venous outflow obstruction that is called Budd-Chiari syndrome (BCS) accounts for 5-10% of portal hypertension.45 BCS is classified as primary or secondary BCS. Primary BCS occurs due to intrinsic intraluminal thrombosis or webs and secondary BCS occurs due to intraluminal invasion or extraluminal compression.4 Hepatic vein occlusion after radiofrequency ablation is classified as secondary BCS and its incidence is very rare. Hepatic vein occlusion occurs by liver parenchymal deformity due to hepatic infarction. However, the reported incidence of hepatic infarction after RFA is only 0.1%.6 Moreover, because of the heat-sink effect that is due to the adjacent hepatic vessels, hepatic infarction rarely occurs around hepatic vein.7
Portal venous stenosis by extrahepatic obstruction accounts for 5-10% of portal hypertension.8 Increasing liver transplantation has led to frequent cases of acquired portal vein stenosis post-transplantation.9 In the non-transplant population, PV stenosis occurs rarely due to tumor encasement or post-surgical complications.10 While PV stenosis was manifested in advanced pancreatic and biliary neoplasms a decade ago, it currently presents as post-surgical complications.1011
Although portal hypertension is derived from different causes, it causes similar and typical symptoms such as ascites, varix or gastrointestinal bleeding. The study of portal hypertension during the past decades has dramatically changed our knowledge of it. Recently, portal pressure gradient has received attention as the complications of portal hypertension.12 According to causes of portal hypertension, different pressure changes are seen between detailed areas such as intrasplenic pressure, portal vein pressure or right atrial pressure. However, all of them increase the portal pressure gradient and can cause the complications of portal hypertension.123 The critical threshold value of portal pressure gradient is 10 mmHg. In other words, if the portal pressure gradient can be controlled at less than 10 mmHg, all complications of portal hypertension can be prevented.
In accordance with this trend, several studies have used insertion of vascular stent to resolve blockage of the portal blood flow and improve symptoms. Although there is no large scale study of usefulness of stent insertion for portal hypertension, previous reports indicated good clinical outcome at various sites from PV to IVC by various causes of portal hypertension.10131415 In our cases, the portal pressure gradient was more than 10 mmHg before the procedure and decreased to below 5 mmHg after the procedure. After control of portal pressure gradient, complications of portal hypertension i.e., ascites, pleural effusion and gastrointestinal bleeding from unknown focus disappeared.
There is currently no consensus on prophylactic anticoagulation therapy for maintaining stent patency after its insertion for portal hypertension. Some recommend at least 6 month interval follow-ups for clinical and laboratory evaluations.2 Our patients were treated with warfarin and evaluated for stent patency using abdomen CT scans every 3 months; consequently, the first stent has been patent for 8 months and the other stent for 6 months.
In conclusion, regardless of the causes, a decrease of the pressure gradient between the PV and the IVC is one of the important treatment strategies of portal hypertension. Vascular stent is useful to reduce the portal pressure gradient and thus, can be a treatment option for portal hypertension.
References
1. Bosch J, Groszmann RJ, Shah VH. Evolution in the understanding of the pathophysiological basis of portal hypertension: How changes in paradigm are leading to successful new treatments. J Hepatol. 2015; 62(1 Suppl):S121–S130. PMID: 25920081.

2. Khanna R, Sarin SK. Non-cirrhotic portal hypertension - diagnosis and management. J Hepatol. 2014; 60:421–441. PMID: 23978714.

3. Sanyal AJ, Bosch J, Blei A, Arroyo V. Portal hypertension and its complications. Gastroenterology. 2008; 134:1715–1728. PMID: 18471549.

4. Bogin V, Marcos A, Shaw-Stiffel T. Budd-Chiari syndrome: in evolution. Eur J Gastroenterol Hepatol. 2005; 17:33–35. PMID: 15647637.
5. Bayraktar UD, Seren S, Bayraktar Y. Hepatic venous outflow obstruction: three similar syndromes. World J Gastroenterol. 2007; 13:1912–1927. PMID: 17461490.

6. Akahane M, Koga H, Kato N, Yamada H, Uozumi K, Tateishi R, et al. Complications of percutaneous radiofrequency ablation for hepato-cellular carcinoma: imaging spectrum and management. Radiographics. 2005; 25(Suppl 1):S57–S68. PMID: 16227497.

7. Lu DS, Raman SS, Vodopich DJ, Wang M, Sayre J, Lassman C. Effect of vessel size on creation of hepatic radiofrequency lesions in pigs: assessment of the "heat sink" effect. AJR Am J Roentgenol. 2002; 178:47–51. PMID: 11756085.
9. Wang J, Yang W, Huang Q, Gao K, Wei B, Zhai R, et al. Interventional treatment for portal venous occlusion after liver transplantation: long-term follow-up results. Medicine (Baltimore). 2015; 94:e356. PMID: 25634164.
10. Woodrum DA, Bjarnason H, Andrews JC. Portal vein venoplasty and stent placement in the nontransplant population. J Vasc Interv Radiol. 2009; 20:593–599. PMID: 19339200.

11. Yamakado K, Nakatsuka A, Tanaka N, Fujii A, Isaji S, Kawarada Y, et al. Portal venous stent placement in patients with pancreatic and biliary neoplasms invading portal veins and causing portal hypertension: initial experience. Radiology. 2001; 220:150–156. PMID: 11425988.

12. Garcia-Tsao G, Bosch J. Management of varices and variceal hemorrhage in cirrhosis. N Engl J Med. 2010; 362:823–832. PMID: 20200386.

13. Zhou ZQ, Lee JH, Song KB, Hwang JW, Kim SC, Lee YJ, et al. Clinical usefulness of portal venous stent in hepatobiliary pancreatic cancers. ANZ J Surg. 2014; 84:346–352. PMID: 23421858.

14. Kim KR, Ko GY, Sung KB, Yoon HK. Percutaneous transhepatic stent placement in the management of portal venous stenosis after curative surgery for pancreatic and biliary neoplasms. AJR Am J Roentgenol. 2011; 196:W446–W450. PMID: 21427310.

15. Cui YF, Fu YF, Wei N, Zhu HC, Xu H. Retrograde puncture assisted hepatic vein recanalization in treating Budd-Chiari syndrome with segmental obstruction of hepatic vein. Radiol Med. 2015; 120:1184–1189. PMID: 26049739.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download