Abstract
Backgrounds/Aims
Tumor recurrence is very common after hepatic resection of hepatocellular carcinoma (HCC) ≥10 cm. The purpose of this study was to validate the prognostic significance of the preoperative alkaline phosphatase (ALP) level and early intrahepatic metastasis in HCC patients who underwent resection of large HCC.
Methods
Clinical data of 100 large HCC patients who underwent liver resection were retrospectively reviewed. All of them underwent protocol transarterial chemoinfusion (TACI) at 1 month.
Results
Median tumor diameter was 13.8 cm, and 94% were single lesions. Systematic and non-systematic resections were performed in 91% and 9%, respectively, with R0 resection achieved in 84%. Overall 1-, 3- and 5-year survival rates were 76%, 38.5%, and 30.4%, respectively. Univariate analyses on patient survival revealed that intrahepatic metastasis on 1-month protocol TACI was the only significant risk factor (p=0.002). Mean ALP values according to the intrahepatic metastasis on 1-month protocol TACI were 124.6±76.9 IU/L and 145.1±92.6 IU/L, which did not show a statistical difference (p=0.23).
Hepatocellular carcinoma (HCC) is one of the most common malignancies worldwide. The mainstay of treatment for HCC has been hepatic resection of curative intent. A considerable proportion of the patients present with advanced large HCC lesions at the time of the initial diagnosis. For patients with HCC larger than 10 cm in diameter, the outcomes of non-surgical treatment are known to be very poor,1 but patients who have had resection show prolonged survival.1-10 Thus if the hepatic functional reserve permits, hepatic resection is regarded as the treatment of choice for large HCC.
However, in patients with large HCC, tumor recurrence is very common after hepatic resection, thus close surveillance is an essential part of the treatment. HCC has various treatment modalities which can be applicable to recurrent lesions such as repeat resection, transarterial chemoembolization (TACE), radio-frequency ablation (RFA) and others. We reported that independent risk factors for HCC recurrence were resection margin less than 1 cm and macrovascular invasion.1 Recently, one Korean study reported that the statistically significant factors that predicted HCC recurrence after large HCC resection were alkaline phosphatase (ALP) ≥80 IU/ml and intrahepatic metastases.2 Since ALP is included in routine biochemical studies, we thought it worthwhile to validate its clinical significance. It was also considered worthy to assess the actual incidence of early intrahepatic metastasis.
To validate the significance of the preoperative ALP level and early intrahepatic metastasis, the clinical data of a consecutive 100 patients who underwent resection of HCC that was ≥10 cm and received protocol transarterial chemoinfusion (TACI) at 1 month were retrospectively reviewed.
Since this study was focused on the role of ALP and its potential correlation with early intrahepatic metastasis, we set the eligibility criteria as follows: resection of HCC lesions larger than 10 cm in the longest diameter; no perioperative mortality; no evidence of bile duct tumor thrombus; and the performance of the protocol TACI at 1 month. The reason why the 1-month protocol TACI was included was that it is the most sensitive test to detect intrahepatic metastasis and it can be concurrently used as an effective treatment modality for recurrent lesions.
All patients were actively followed up with serum tumor markers (alpha-fetoprotein [AFP] and proteins induced by vitamin K absence or antagonist-II [PIVKA-II]), dynamic liver computed tomography (CT), liver ultrasonography and chest x-ray every one or two months, especially during the first 2 years. For suspected recurrence, all available diagnostic modalities including hepatic angiography, magnetic resonance imaging, high-resolution chest CT and positron emission tomography-CT were performed. We tried to treat the recurrent HCC lesion as vigorously as we could.
All numeric data were reported as the mean and standard deviation, and as the median and range. The continuous variables were compared by using Student's t-test. Survival curves were estimated by the Kaplan-Meier method and compared using the log-rank test. Differences of p<0.05 were considered statistically significant.
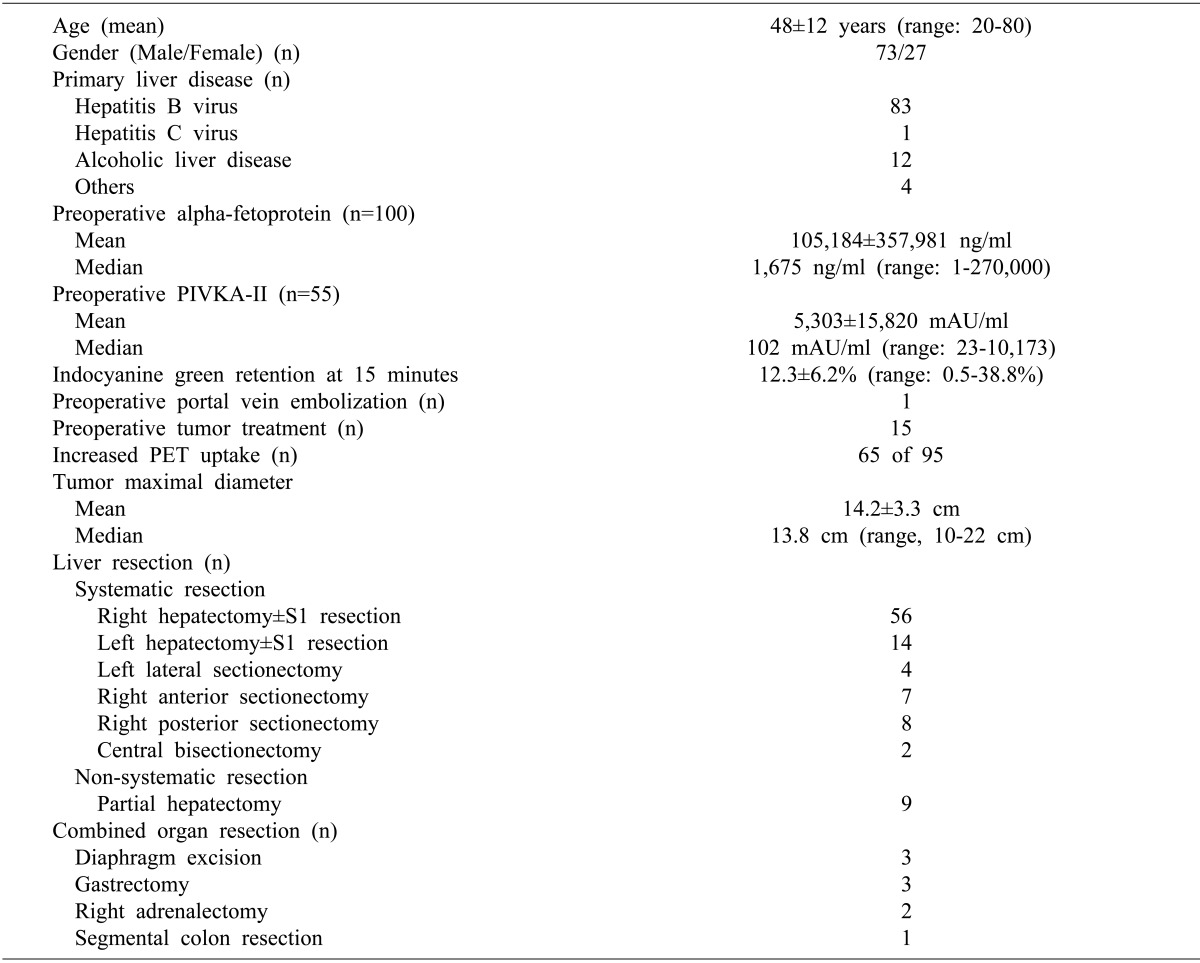
The clinicopathologic features and surgical treatments of these 100 patients are summarized in Table 1.
Systematic resection was performed in 91 and tumor-free resection margin was obtained in 84. The tumor number was a single tumor in 94, two in 5, and three in 1. Satellite nodules were identified in 18. Glissonian capsule invasion was found in 21. Micro- and macrovascular invasions were found in 73 and 21, respectively. A wide range of tumor necrosis was observed in 85. Tumor differentiation was well-to-moderate in 80 and poor in 20.
All 100 patients underwent 1-month protocol TACI to detect and treat early intrahepatic metastasis. The TACI timing was determined to be 3 to 5 weeks after the surgery depending on the patient's condition. One-month intrahepatic metastasis was found in 45, in which single and multiple lesions were observed in 15 and 30, respectively (Fig. 1). When metastatic lesions were observed, the TACI was converted to TACE for therapeutic purposes. Interestingly, one patient who had early multiple recurrences at 1 month did not reveal any evidence of further HCC recurrence during the next 22 months to date.
During the outpatient clinic follow-up, 83 of 100 patients showed HCC recurrence. The initial recurrence sites were the liver in 61, lung in 15, bone in 2, adrenal gland in 1, liver and lung in 2, and lung and brain in 1. Every available loco-regional treatment was performed on all of the recurrent patients, and Sorafenib was also administered in 44.
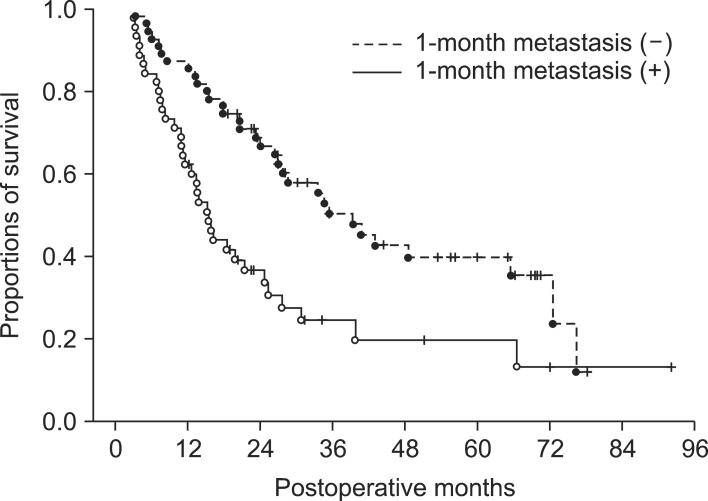
The overall patient survival curves are depicted in Fig. 2. Patient survival rates were 76% at 1 year, 38.5% at 3 years and 30.4% at 5 years.
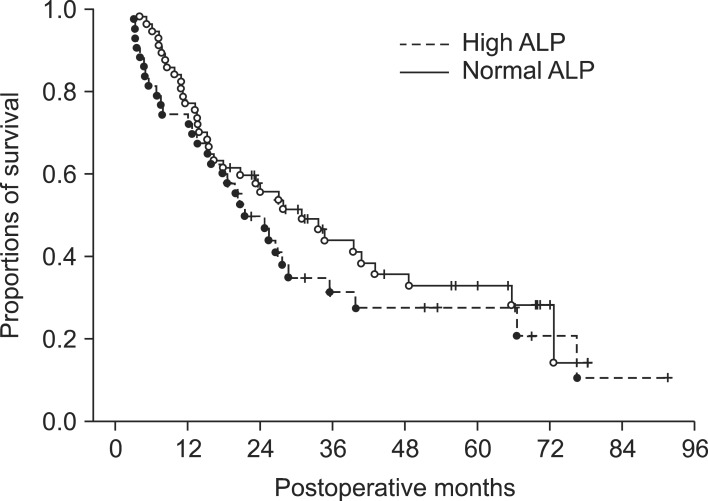
Univariate analyses on patient survival revealed that hepatitis B virus infection (vs. non-hepatitis B, p=0.48), AFP ≥100 ng/ml (p=0.089, Fig. 3), PIVKA-II ≥200 mAU/ml (p=0.19), tumor differentiation (well-to-moderate vs. poor, p=0.38), systematic resection (vs. non-systematic resection, p=0.41), R0 resection (vs. R1 resection, p=0.09), ALP ≥100 IU/L (p=0.31, Fig. 4), intrahepatic metastasis on 1-month protocol TACI (p=0.002, Fig. 5), microvascular invasion (p=0.06) and macrovascular invasion (p=0.09).
Mean ALP values according to intrahepatic metastasis on 1-month protocol TACI were 124.6±76.9 IU/L and 145.1±92.6 IU/L, which did not show a statistical difference (p=0.23).
HCC size has been traditionally considered as one of the most important risk factors for HCC recurrence and patient survival, but other biological factors are also involved in HCC recurrence.11 A huge size of the HCC per se implies that the lesion is advanced already, and there is a higher possibility of tumor spread, including the existence of satellite nodules or macrovascular invasion.12 Such advanced tumors induce an increased risk of tumor recurrence after resection, and thus, the merits of hepatic resection are diminished in this situation.
Even after resection of large HCC, a majority of patients show tumor recurrence within the first year. Interestingly, in the 1-month TACI surveillance of this study, single intrahepatic metastasis was found in 15% and another 30% showed multiple intrahepatic metastases. Considering that only 3-5 weeks had passed after the surgery and the usual HCC tumor doubling time is not short,13,14 these HCC lesions appear to be evidence of the spread of the preexisting tumor before the resection. Accelerated liver regeneration followed by liver resection may contribute to the rapid growth of such metastatic lesions. Absence of such intrahepatic metastases must lead to improved patient outcomes. The actual prognostic benefit of the 1-month protocol TACI was not fully proven in this study, but it can be an important diagnostic and therapeutic modality before the appearance of visible intrahepatic metastases on imaging studies. Considering the high early recurrence rate after resection of large HCC, any preventive treatment modality appears to be necessary even after curative resection. However, to date, no standard treatment has been proven to be effective for wide usage.15,16 We think that it is reasonable to include the 1-month protocol TACI as one of the routine preventive measures.
For resection of large HCC ≥10 cm, the risk factors were widely variable depending on the patient groups.1-10 Compared with even our previous study, we found that most risk factors lost their statistical significance in this study.1 One Korean study reported that the statistically significant factors that predicted HCC recurrence after large HCC resection were ALP ≥80 IU/ml and intrahepatic metastases.2 We investigated the significance of the ALP, but in vain. This validation study failed to prove the prognostic role of preoperative ALP.
In this study, most of the initial HCC recurrences were presented with intrahepatic recurrence, whereas some patients showed extrahepatic recurrence, especially at the lung. To treat intrahepatic recurrent HCC, TACE has been most commonly used after hepatectomy,17 especially in patients with multifocal recurrence within the remnant liver. Percutaneous RFA is also an effective and safe method for treating recurrent HCC in the remnant liver.18 Aggressive management with resection of isolated extrahepatic recurrence, especially solitary lung metastasis, was reported to offer long-term survival.19-21
In conclusion, in patients with large HCC ≥10 cm, the 1-month protocol TACI combined with hepatic resection may contribute to the early detection and timely treatment of potentially preexisting metastatic lesions.
References
1. Lee SG, Hwang S, Jung JP, et al. Outcome of patients with huge hepatocellular carcinoma after primary resection and treatment of recurrent lesions. Br J Surg. 2007; 94:320–326. PMID: 17205495.

2. Kim JM, Kwon CH, Joh JW, et al. The effect of alkaline phosphatase and intrahepatic metastases in large hepatocellular carcinoma. World J Surg Oncol. 2013; 11:40. PMID: 23432910.

3. Poon RT, Ngan H, Lo CM, et al. Transarterial chemoembolization for inoperable hepatocellular carcinoma and postresection intrahepatic recurrence. J Surg Oncol. 2000; 73:109–114. PMID: 10694648.

4. Mok KT, Wang BW, Lo GH, et al. Multimodality management of hepatocellular carcinoma larger than 10 cm. J Am Coll Surg. 2003; 197:730–738. PMID: 14585406.

5. Yeh CN, Lee WC, Chen MF. Hepatic resection and prognosis for patients with hepatocellular carcinoma larger than 10 cm: two decades of experience at Chang Gung memorial hospital. Ann Surg Oncol. 2003; 10:1070–1076. PMID: 14597446.

6. Zhou XD, Tang ZY, Ma ZC, et al. Surgery for large primary liver cancer more than 10 cm in diameter. J Cancer Res Clin Oncol. 2003; 129:543–548. PMID: 12898232.
7. Chen XP, Qiu FZ, Wu ZD, et al. Chinese experience with hepatectomy for huge hepatocellular carcinoma. Br J Surg. 2004; 91:322–326. PMID: 14991633.

8. Nagano Y, Tanaka K, Togo S, et al. Efficacy of hepatic resection for hepatocellular carcinomas larger than 10 cm. World J Surg. 2005; 29:66–71. PMID: 15599739.

9. Liau KH, Ruo L, Shia J, et al. Outcome of partial hepatectomy for large (>10 cm) hepatocellular carcinoma. Cancer. 2005; 104:1948–1955. PMID: 16196045.
10. Pawlik TM, Poon RT, Abdalla EK, et al. International Cooperative Study Group on Hepatocellular Carcinoma. Critical appraisal of the clinical and pathologic predictors of survival after resection of large hepatocellular carcinoma. Arch Surg. 2005; 140:450–457. PMID: 15897440.

11. Vauthey JN, Lauwers GY, Esnaola NF, et al. Simplified staging for hepatocellular carcinoma. J Clin Oncol. 2002; 20:1527–1536. PMID: 11896101.

12. Pawlik TM, Delman KA, Vauthey JN, et al. Tumor size predicts vascular invasion and histologic grade: Implications for selection of surgical treatment for hepatocellular carcinoma. Liver Transpl. 2005; 11:1086–1092. PMID: 16123959.

13. Lou CY, Feng YM, Qian AR, et al. Establishment and characterization of human hepatocellular carcinoma cell line FHCC-98. World J Gastroenterol. 2004; 10:1462–1465. PMID: 15133854.

14. Liu ZZ, Huang WY, Lin JS, et al. Cell cycle and radiosensitivity of progeny of irradiated primary cultured human hepatocarcinoma cells. World J Gastroenterol. 2005; 11:7033–7035. PMID: 16437612.

15. Sun HC, Tang ZY. Preventive treatments for recurrence after curative resection of hepatocellular carcinoma--a literature review of randomized control trials. World J Gastroenterol. 2003; 9:635–640. PMID: 12679900.
16. Ren ZG, Lin ZY, Xia JL, et al. Postoperative adjuvant arterial chemoembolization improves survival of hepatocellular carcinoma patients with risk factors for residual tumor: a retrospective control study. World J Gastroenterol. 2004; 10:2791–2794. PMID: 15334671.

17. Chen WT, Chau GY, Lui WY, et al. Recurrent hepatocellular carcinoma after hepatic resection: prognostic factors and long-term outcome. Eur J Surg Oncol. 2004; 30:414–420. PMID: 15063895.

18. Choi D, Lim HK, Kim MJ, et al. Recurrent hepatocellular carcinoma: percutaneous radiofrequency ablation after hepatectomy. Radiology. 2004; 230:135–141. PMID: 14631050.

19. Poon RT, Fan ST, O'Suilleabhain CB, et al. Aggressive management of patients with extrahepatic and intrahepatic recurrences of hepatocellular carcinoma by combined resection and locoregional therapy. J Am Coll Surg. 2002; 195:311–318. PMID: 12229937.
20. Zhou XD, Tang ZY, Yang BH, et al. Experience of 1000 patients who underwent hepatectomy for small hepatocellular carcinoma. Cancer. 2001; 91:1479–1486. PMID: 11301395.

21. Hwang S, Kim YH, Kim DK, et al. Resection of pulmonary metastases from hepatocellular carcinoma following liver transplantation. World J Surg. 2012; 36:1592–1602. PMID: 22411088.

Fig. 1
Patterns of intrahepatic metastasis at 1-month protocol transarterial chemoinfusion. Arrows indicate single (A and B) and multiple lesions (C and D).
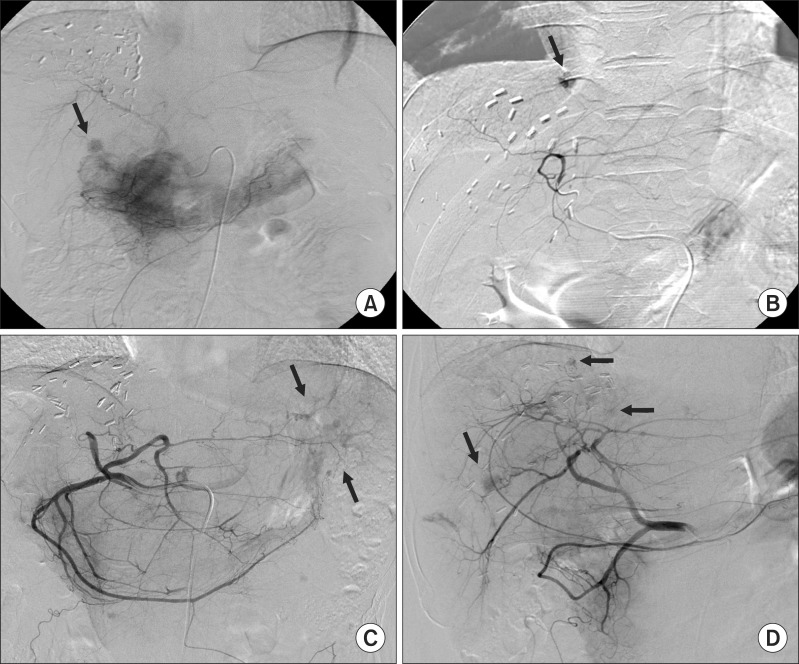
Fig. 2
Overall patient survival curve of 100 patients who underwent resection of hepatocellular carcinomas larger than 10 cm in diameter.
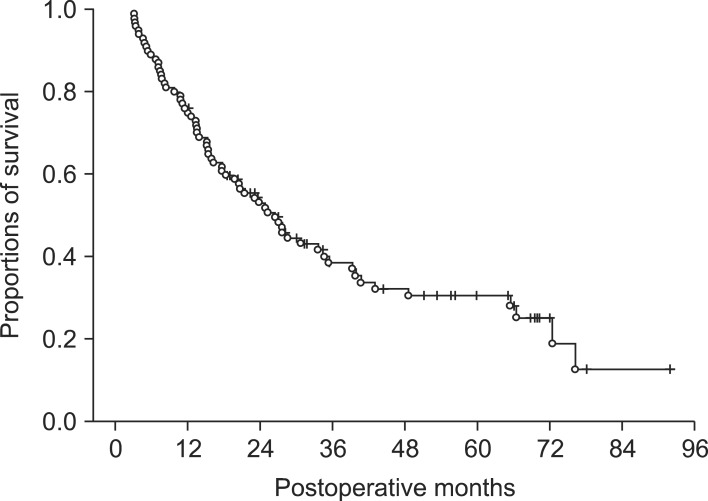
Fig. 3
Comparison of the patient survival curve according to preoperative alpha-fetoprotein (AFP) levels.
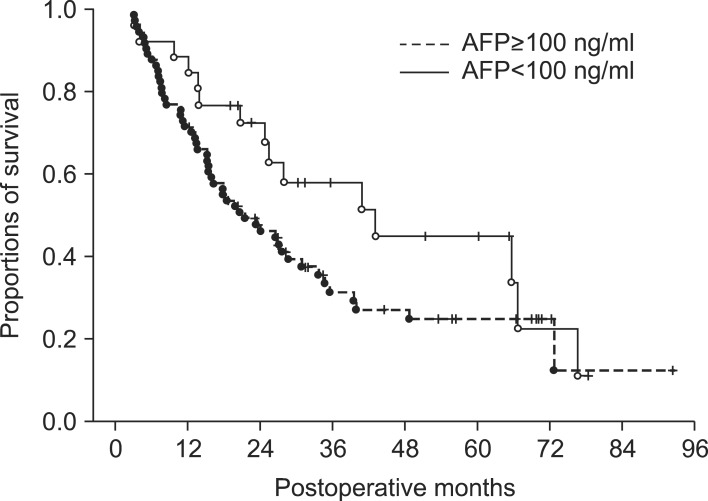
Fig. 4
Comparison of the patient survival curve according to preoperative alkaline phosphatase (ALP) levels.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download