Abstract
Purpose
We wanted to determine whether additional breast ultrasound examinations are needed for patients who have clustered calcifications found by mammography for the detection of breast carcinomas.
Methods
We performed targeted ultrasound examinations in 125 consecutive patients who had clustered calcifications found by mammography. Forty-eight pathologically proven patients with 61 breast lesions were included in this study (26 invasive carcinomas, 10 ductal carcinomas in situ and 25 benign diseases). Two breast radiologists evaluated the mammography and the ultrasound findings and they graded the probability of malignancy by consensus as follows: definitely benign 1, probably benign 2, probably malignant 3, and definitely malignant 4. The diagnostic performance values, including the sensitivity, specificity, accuracy, positive predictive value and negative predictive value, for mammography and additional ultrasound were compared using McNemar's test and receiver operating characteristic (ROC) analysis. On the ROC analysis, areas under the ROC curves (AUC) and 95% confidence intervals (CI) were obtained.
Results
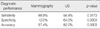
The sensitivity, specificity, accuracy, positive predictive value, and negative predictive value for making the diagnosis of breast carcinoma by mammography were 88.9%, 12.0%, 57.4%, 59.3%, and 42.9% and those for additional ultrasound were 94.4%, 64.0%, 82.0%, 79.1%, and 88.9%, respectively. The differences of specificity and accuracy were statistically significant (p=0.0003). On the ROC analysis, ACU were significantly different between mammography (AUC=0.586, 95% CI=0.453-0.711) and ultrasound (AUC=0.823, 95% CI=0.704-0.909) (p=0.003). Clustered calcifications with associated masses or ductal changes on additional breast ultrasound had high frequency of malignancies, 79% or 73%. In addition, 87% of malignant masses were invasive carcinomas and 45% of malignant ductal changes were ductal carcinomas in situ.
Conclusion
Additional breast ultrasound examinations for the lesions with clustered calcifications on mammography can improve the diagnostic performance and significantly contribute to the specificity and accuracy of a diagnosis of breast carcinoma. In addition, the ultrasound features may predict the pathologic findings such as benignity or malignancy and invasive carcinoma or ductal carcinoma in situ.
Mammographic breast screening programs have increased the detection of early nonpalpable breast carcinoma and reduced the mortality rate of breast carcinoma.(1) Moreover, calcifications may be the most reliable mammographic feature in early nonpalpable breast carcinoma, and are present in 30-50% of breast carcinomas.(2,3)
Mammography is highly sensitive at evaluating breast calcifications, but its specificity for a diagnosis of breast carcinoma is limited. Only 20-35% of cases with calcifications are proven to be carcinomas after wire localization and excisional biopsy.(4-6) Therefore, unnecessary biopsies are performed and these cause worry and increase medical costs.
It has been reported that high-resolution ultrasound (US) can improve the detection and characterization of breast calcifications.(7,8) On breast US, calcifications are visualized as echogenic dots. However, US has low sensitivity as a primary imaging modality for the detection of calcifications, which remains its major limitation.(9) Furthermore, when calcifications are located inside echogenic, fibroglandular breast tissues, they may not be depicted by US because it is difficult to differentiate them from echogenic interfaces among tissues. However, US can detect associated masses or ductal changes in patients with calcifications, thus, US might be a feasible second-line additional diagnostic tool.
The purpose of this study was to determine whether additional US is needed in patients with clustered calcifications by mammography to improve diagnostic accuracy for breast carcinoma.
This study was approved by the institutional review board for human investigations. During the period from September 2005 to October 2007, when a patient had clustered calcifications without an associated mass or density in mammography, targeted US was performed on areas of clustered calcifications after mammography-guided 2D localization. A total 125 patients were scanned by US for evaluation of mammographically detected clustered calcifications. In the current study, we included lesions with tissue diagnosis for assessment of diagnostic benefits of additional US in patients with clustered calcifications by mammography. Among all 125 patients, 50 patients with 63 lesions were obtained tissue diagnosis by US-guided core needle biopsy (n=35), mammotome biopsy (n=5), or surgical excision (n=23) and two lesions that did not contain calcifications with specimens were excluded to eliminate the possibility of inadequate sampling. Accordingly, pathologically proven 48 patients with 61 lesions were included in this study. Specimen radiographs were obtained of all 61 lesions to confirm whether specimens contained calcifications. After confirming the presence of calcifications, specimens were sent for pathologic examination. Hematoxylin and Eosin-stained (H&E) sections of all breast lesions were examined by a board-certified pathologist.
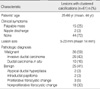
Table 1 demonstrates patients and lesions characteristics. All patients were women and mean age was 44 yr. The size of lesions was obtained by using mammography and the maximum distance of calcifications was measured. By pathologic examination 36 (59%) of the 61 breast lesions were malignant and the 36 malignant lesions were treated by mastectomy (n=16) or breast conserving surgery (n=20). When we correlated with clinical symptoms and pathologic findings, all 15 palpable masses were malignant; 13 invasive ductal carcinomas and 2 ductal carcinoma in situ (DCIS) cases. Of the two lesions with a nipple discharge, one was DCIS and the other was an intraductal papilloma. In terms of the 44 asymptomatic lesions, 13 were invasive ductal carcinomas, 7 were DCIS cases, and the remaining 24 were benign diseases.
Mammograms were obtained either using a film-screen mammography system (Bennett Contour; Bennett Co., New York, USA) or a digital mammography system (Selenia IV; Lorad, Bedford, USA). In all 48 patients, standard craniocaudal and mediolateral oblique views were obtained followed by spot compression or magnification views of areas containing calcifications. Mammography images were evaluated as described by the Breast Imaging Reporting and Data System (BI-RADS®)-Mammography issued by the American College of Radiology.(10)
We evaluated breast compositions and calcification morphologies. Breast compositions were categorized into 4 types; 1) extremely dense, 2) heterogeneously dense, 3) scattered fibroglandular densities, and 4) almost entirely fat. Calcification morphologies were categorized into 7 types; 1) lucent-centered, 2) coarse, 3) round or punctate, 4) amorphous or indistinct, 5) coarse heterogeneous, 6) fine pleomorphic, and 7) fine linear or fine-linear branching calcifications.
US examinations were performed using HDI 5000SonoCT or iU22 units (Advanced Technology Laboratories, Bothell, USA) using a broad-bandwidth (14-5 MHz) linear scanhead. Transverse, sagittal, radial, and antiradial scans were obtained with knowledge of mammographic findings concerning the presences and areas of calcifications, which allowed examiners to focus on suspicious areas. On US, the presence of calcifications was also suggested when echogenic dots with or without acoustic shadowing were observed.
US findings in presumed calcification regions were classified as follows: 1) calcifications with a visible mass, 2) calcifications with ductal change, 3) calcifications within a normal duct, 4) calcifications with cysts, 5) calcifications without an associated finding, or 6) none. For mass lesions, we evaluated shape and margin to determine probabilities of malignancy. Ductal change was defined as an abnormal caliber and/or arborization according to the BI-RADS®-Ultrasound lexicon.(11)
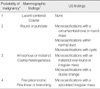
All mammographic and US images were evaluated by consensus between two breast radiologists and probabilities of malignancy were determined based on mammographic and additional breast US findings, respectively. We defined the grades of probability of malignancy according to the BI-RADS® lexicon and the previous studies.(3,7,8,10-13) Table 2 summarizes definitions of probabilities of malignancy for mammographic and US findings. Probabilities of malignancy were categorized into 4 types: 1) definitely benign, 2) probably benign, 3) probably malignant, and 4) definitely malignant.
Diagnostic performances including sensitivity, specificity, accuracy, positive predictive value (PPV), and negative predictive value (NPV) for diagnosis of breast carcinoma were calculated for mammographic and additional breast US findings. Probability of malignancy was dichotomized for assessment of diagnostic performances. Grade 3 (probably malignant) and 4 (definitely malignant) by mammography or US were defined as 'positive' for the purpose of calculating diagnostic parameters and grade 1 (definitely benign) and grade 2 (probably benign) were considered as 'negative'. Diagnostic performances were based on pathologic results. McNemar's test was used to compare sensitivity, specificity, and accuracy values of mammography and additional US. In addition, receiver operating characteristic (ROC) curves were plotted and areas under the ROC curves (AUC) and 95% confidence intervals (CI) were calculated for comparison of diagnostic performance between mammography and additional breast US. Statistical significance was considered if a p-value was less than 0.05. All statistical analyses were performed using SAS version 9.12 (SAS Institute, Cary, USA). The statistical analyses of the data were supervised by a biostatistician.
Breast compositions for the 61 lesions were; almost entirely fat (n=3), scattered fibroglandular densities (n=15), heterogeneously dense (n=11), and extremely dense (n=32). Calcification morphologies were; lucent-centered in 1 lesion, coarse in 1 lesion, round or punctate in 5 (Figure 1), amorphous or indistinct in 10, coarse heterogeneous in 3 (Figure 2), fine pleomorphic in 28 (Figures 3, 4), and fine linear or branching in 13. Therefore, malignancy probability grades were; grade 1 in 3% (2/61), grade 2 in 8% (5/61) (Figure 1), grade 3 in 21% (13/61) (Figure 2), and grade 4 in 67% (41/61) (Figures 3, 4).
Table 3 demonstrates the correlation between grades of probability of malignancy using mammography or additional US and pathologic diagnoses. On pathologic examinations, all 13 fine linear or branching calcifications (grade 4) were proven as malignancies, and 50% (14/28) of fine pleomorphic calcifications (grade 4) and 40% (4/10) of amorphous calcifications (grade 3) were malignant. Punctate calcifications were classified into grade 2, probably benign lesions according to the BI-RADS®-Mammography lexicon, however, three (60%) of 5 punctate calcifications were proven as malignancies and two malignant lesions were DCIS cases (Figure 1).
In 61 lesions with mammographically detected clustered calcifications, 47 (77%) lesions were identified by breast US. Most of these 47 lesions had associated masses (Figures 1, 2) or ductal changes (Figure 3) in 29 (47%) and 15 (25%) lesions, respectively. The probability of malignancy grades were grade 1 in 23% (14/61) (Figure 4), grade 2 in 7% (4/61), grade 3 in 59% (36/61) (Figures 1, 3), and grade 4 in 11% (7/61) (Figure 2).
Table 4 summarizes the frequencies of malignancies according to US findings. Of the 29 lesions with associated masses by additional breast US, 23 (79%) were diagnosed as malignancies. Most associated masses (97%, 28/29) were grade 3 or 4. The characteristics of masses based on the BI-RADS®-Ultrasound lexicon were correlated with pathologic findings. All 7 spiculated irregular masses (grade 4) and 16 (76%) of 21 indistinct oval, round, or irregular masses (grade 3) were malignancies (Figures 1, 2). In these 23 malignant calcifications with associated masses on US, 20 (87%) were invasive ductal carcinomas; 7 spiculated masses and 13 indistinct masses. On the other hand, 11 (73%) out of 15 lesions with ductal changes on additional breast US were proven as malignancies on pathologic examinations (Figure 3) and five lesions (45%, 5/11) were DCIS cases.
The two lesions categorized as microcalcifications within normal ducts because ductal diameters were normal and no ductal wall thickening was evident were benign. In 14 clustered calcifications without detectable breast lesions on US, two lesions were malignancies, DCIS cases (Table 3). These two lesions were shown as amorphous calcifications (grade 3) and punctuate calcifications (grade 2) on mammography.
The sensitivity, specificity, accuracy, PPV and NPV for a diagnosis of breast carcinoma by mammography were 88.9%, 12.0%, 57.4%, 59.3%, and 42.9%, respectively, and those by additional US were 94.4%, 64.0%, 82.0%, 79.1%, and 88.9%, respectively. All diagnostic performance values of additional US were higher than those of mammography alone. Specificity and accuracy values of additional US were significantly higher than those of mammography (p=0.0003) (Table 5). Figure 5 shows the ROC analysis for diagnostic performance of mammography and additional US. The AUC was 0.586 (95% CI, 0.453-0.711) for mammography and 0.823 (95% CI, 0.704-0.909) for breast US. This difference was statistically significant (p=0.003).
Mammography is the gold standard for the detection and characterization of calcifications, but although mammography is highly sensitive at detecting calcifications, it has low specificity, which results in a large number of false-positive mammograms and low true-positive biopsy rates. Moreover, although some benign calcifications cannot be distinguished from those of malignancy, the number of biopsies for benign conditions could be decreased by carefully analyzing mammograms for features that indicate benignity. Several studies have revealed the feasibility of US for the evaluation of calcifications. In 1982, Kasumi and Tanaka succeeded in detecting calcifications (down to 110 µm in size) within breast carcinomas by US, and subsequently the ability of high-resolution US to demonstrate calcifications within breast carcinomas was evaluated.(12,14) US is less sensitive than mammography at demonstrating calcifications, but modern US transducer technology offers substantially improved spatial resolution and contrast, and thus, allows breast calcifications to be better and more frequently visualized, especially in dense breasts.(13) Moreover, high-resolution US is able to visualize calcifications within breast carcinomas with a sensitivity of 95%.(12,13) In the current study, our goal was to determine whether additional US is needed in patients with clustered calcifications by mammography to improve the diagnosis of breast carcinoma. Thus, we studied consecutive pathologically verified clustered calcifications by mammography.
In this study, we graded probability of malignancy using mammographic and US imaging findings: 1) definitely benign, 2) probably benign, 3) probably malignant, and 4) definitely malignant. Why we chose not to use the familiar BI-RADS® lexicon we conducted. First, the lesions with microcalcifications are described in detail in the BI-RADS®-Mammography lexicon.(10) Their morphology, distribution, and final assessment about probability of malignancy are written in the lexicon. However, the BI-RADS®-Ultrasound lexicon does not give full details of lesions with microcalcifications.(11) In the BI-RADS®-Ultrasound lexicon, the location of microcalcifications is only mentioned such as microcalcifications out of a mass or microcalcifications in a mass and there is no any description about probability of malignancy according to the characteristics of lesions with microcalcifications.(11) Therefore, we could not use the BI-RADS® assessment categories for analysis of the lesions with clustered microcalcifications on breast US. In the current study, we graded the lesions into four types in terms of probability of malignancy based on the BI-RADS® lexicon and the previous studies.(3,7,8,10-13) Second, while radiologists are well trained in the use of BI-RADS® terms, BI-RADS® terms do not measure anything in the required and statistically continuous fashion that would be suitable for ROC analysis. Our scale of probability of malignancy did allow the reader to record an impression of malignancy on a four-point scale. This allows the drawing of smooth ROC curves.
On mammography, lucent centered, coarse, round, or punctate calcifications are classified as typical benign calcifications in by BI-RADS®-Mammography, and thus, we graded these calcifications as 1 or 2, i.e., negative for malignancy. However, one lesion with coarse calcifications (grade 1) and three lesions with punctate calcifications (grade 2) were confirmed as breast carcinoma by pathologic examinations. The lesion that was assessed as grade 1 by mammography was categorized as grade 3 by additional breast US because of an indistinct oval mass, and this was confirmed to be invasive ductal carcinoma by pathologic examination. The three lesions that were assessed as grade 2 by mammography were confirmed as DCIS in two and as invasive ductal carcinoma in one. These three lesions were assessed as grade 3 by breast US because of indistinct oval masses in two lesions and ductal change in one. Thus, these were false negative cases by mammography and US helpfully detected the presence of breast carcinoma. According to the BI-RADS®-Mammography lexicon, round or punctate calcifications are classified as typical benign calcifications, and round calcifications smaller than 0.5 mm as punctate calcifications.(10) The lexicon further advocates that an isolated cluster of punctate calcifications may warrant close surveillance or even biopsy if new or ipsilateral to a cancer, even though these calcifications are classified as typically benign. In our study, three lesions with punctate calcifications were categorized as probably benign by mammography, but were diagnosed as breast carcinoma by pathologic examinations. Furthermore, the frequency (60%) of breast carcinoma among punctate calcifications was higher than that (38%) among amorphous or coarse heterogeneous calcifications. Amorphous or coarse heterogeneous calcifications are classified as intermediate concern, suspicious calcifications in the BI-RADS® lexicon.(10) It has also been reported that cribriform and micropapillary DCIS has characteristically punctate calcifications.(2) Accordingly, it may be necessary to revise the classification of punctate calcifications in the next edition of the BI-RADS®-Mammography lexicon. We recommend round and punctate calcifications to be devised and punctate calcifications to be included as lesions of intermediate concern, suspicious calcifications.
The lesions with associated masses on breast US had a high rate (23/29, 79%) of breast carcinoma on pathologic examination. Several reports have shown that clustered calcifications associated with a visual mass are virtually pathognomonic for carcinoma, thus, our results concur with these reports.(2,3,8) In the present study, the characteristics of associated masses, such as, shapes and margins were also important differentiators of benignity and malignancy like isolated masses. Therefore, if a mass is associated with clustered calcifications, we should analyze the mass like an isolated mass according to BI-RADS® lexicon.
In terms of the diagnostic performances of mammography and breast US for evaluation of clustered calcification, all values, including sensitivity, specificity, accuracy, PPV, and NPV, were higher for breast US than mammography. In particular, the specificity and accuracy after performing additional breast US were substantially greater than those of mammography only. For assessment of additional effect of breast US, we used ROC analysis and the AUC values were significantly higher after using the additional breast US (0.823) than using only mammography (0.586). Mammography has been used as a gold standard for examination of microcalcifications. We routinely perform additional mammography for analysis of clustered microcalcifications such as magnification or compression views or zooming process on the monitor in digital mammography for magnifying the microcalcifications. However, low specificity is still a weak point of mammography, especially in terms of assessing clustered calcifications. Furthermore, most clustered microcalcifications are small in size and asymptomatic. In our cases, the mean size of lesions on mammography was 14 mm and 44 (72%) of all 61 lesions had no symptoms. However, 20 (45%) of 44 asymptomatic lesions were proven as malignancy. Thus, our results indicate that additional breast US after mammographic evaluation can be highly recommended as a second-line imaging modality for improving diagnostic performances and positive biopsy rate, and decreasing unnecessary biopsy in cases with clustered calcifications without any associated masses or densities on mammography. Furthermore, US can detect associated features, such as, masses or ductal changes and may be helpful at predicting the presence of invasive carcinoma or DCIS. On breast US, most lesions with associated malignant masses were invasive carcinomas (20/23, 87%), though a few (3/23, 13%) were DCIS. On the other hand, 45% (5/11) of lesions with associated ductal change on breast US were DCIS cases.
This study has several limitations. First, the cohort was relatively small because we only included pathologically verified clustered calcifications in this study. Most clustered calcifications with no associated masses are small and asymptomatic, thus, these are initially detected by screening mammography. After initial detection of clustered calcifications, the patients are classified into diagnostic population for additional evaluation, such as additional mammography or other imaging modalities. And then the lesions are finally assessed and recommended for tissue biopsy or short-interval follow-up by using all imaging modalities. Our goal of this study was to determine whether additional breast US after mammography can improve diagnostic performance when compared with mammography alone, especially specificity. Specificity is the weak point of mammography and these are related with overdiagnosis, unnecessary biopsy, increase of medical cost, and patients' anxiety. In addition, there are three definitions about PPV on the BI-RADS® lexicon and PPV3 is known as the Positive Biopsy Rate or Biopsy Yield of Malignancy.(10) Therefore, we used only pathologically verified clustered calcifications for assess the diagnostic performances of two imaging modalities. Second, the US examinations were highly dependent on examiner's experience and transducer technology, and thus, imaging findings were classified in a subjective manner in this study.
In conclusion, additional breast US can improve diagnostic performance for lesions with clustered calcifications on mammography, and that it can substantially increase diagnostic specificity and accuracy for diagnosis of breast carcinoma. In addition, breast US can detect associated masses or ductal changes, which are associated with higher malignancy rate. The study demonstrates the majority of lesions with associated malignant masses were invasive carcinomas and half of the lesions with associated malignant ductal changes were DCIS. Accordingly, additional breast US may be helpful for predicting malignant tumor type.
Figures and Tables
Figure 1
A 40-yr-old woman with ductal carcinoma in situ in the right breast. (A) A mediolateral oblique view showing clustered punctate calcifications (arrows) in the right breast, which were assessed as grade 2 for malignancy probability. (B) The ultrasound (US) image showing an associated indistinct irregular mass (arrows) with calcifications (arrowheads), which was assessed as grade 3 for malignancy probability. This case was false negative by mammography and true positive by breast US.

Figure 2
A 30-yr-old woman with invasive ductal carcinoma in the left breast. (A) A craniocaudal spot compression mammographic view shows clustered coarse heterogeneous calcifications (arrows) in left breast, which was assessed as grade 3. (B) A breast ultrasound (US) image demonstrates an associated mass (arrows) with an irregular shaped, spiculated margined hypoechoic pattern, which was assessed as grade 4. This case was true positive by mammography and breast US.

Figure 3
A 46-yr-old woman with ductal carcinoma in situ in the left breast. (A) Mediolateral oblique view shows clustered fine pleomorphic calcifications (arrows) in the left breast. Malignancy probability was assessed as grade 4 on mammography. (B) A breast ultrasound (US) image shows associated ductal changes (arrows) with calcifications (arrowheads). On ultrasound, the malignancy probability was assessed as grade 3. This lesion was true positive by mammography and breast US.

Figure 4
A 48-yr-old woman with nonproliferative fibrocystic change in the left breast. (A) A mediolateral oblique view shows clustered fine pleomorphic calcifications (arrows) in the left breast, which were assessed as grade 3 for malignancy probability. (B) A ultrasound (US) image demonstrates no abnormal finding in the region of interest, and thus the assessment was grade 1 for malignancy probability. This case was false positive by mammography and true negative by breast US.

Figure 5
ROC curves for diagnostic performance of mammography and additional US. The AUC was 0.586 (95% CI, 0.453-0.711) for mammography alone and 0.823 (95% CI, 0.704-0.909) for additional breast US evaluation after mammographic examination. This difference was statistically significant (p=0.003).
ROC=receiver operating characteristic; US=ultrasound; AUC=areas under the ROC curves; CI=confidence intervals.

Table 3
Correlation between grades of probability of malignancy using mammography or additional US and pathologic diagnoses

References
1. Morimoto T, Okazaki M, Endo T. Current status and goals of mammographic screening for breast cancer in Japan. Breast Cancer. 2004. 11:73–81.

2. Bassett LW. Mammographic analysis of calcifications. Radiol Clin North Am. 1992. 30:93–105.
3. Yang WT, Suen M, Ahuja A, Metreweli C. In vivo demonstration of microcalcification in breast cancer using high resolution ultrasound. Br J Radiol. 1997. 70:685–690.

4. Ciatto S, Cataliotti L, Distante V. Nonpalpable lesions detected with mammography: review of 512 consecutive cases. Radiology. 1987. 165:99–102.

5. Meyer JE, Eberlein TJ, Stomper PC, Sonnenfeld MR. Biopsy of occult breast lesions. Analysis of 1261 abnormalities. JAMA. 1990. 263:2341–2343.

6. Orel SG, Kay N, Reynolds C, Sullivan DC. BI-RADS categorization as a predictor of malignancy. Radiology. 1999. 211:845–850.

7. Kang SS, Ko EY, Han BK, Shin JH. Breast US in patients who had microcalcifications with low concern of malignancy on screening mammography. Eur J Radiol. 2008. 67:285–291.

8. Moon WK, Im JG, Koh YH, Noh DY, Park IA. US of mammographically detected clustered microcalcifications. Radiology. 2000. 217:849–854.

9. Cilotti A, Bagnolesi P, Moretti M, Gibilisco G, Bulleri A, Macaluso AM, et al. Comparison of the diagnostic performance of high-frequency ultrasound as a first- or second-line diagnostic tool in non-palpable lesions of the breast. Eur Radiol. 1997. 7:1240–1244.

10. American College of Radiology. Breast imaging reporting and data system (BI-RADS®)-Mammography. 2003. 4th ed. Reston: American College of Radiology.
11. American College of Radiology. Breast imaging reporting and data system (BI-RADS®)-Ultrasound. 2003. 1st ed. Reston: American College of Radiology.
12. Kasumi F. Can microcalcifications located within breast carcinomas be detected by ultrasound imaging? Ultrasound Med Biol. 1988. 14:Suppl 1. 175–182.

13. Chiou SY, Chou YH, Chiou HJ, Wang HK, Tiu CM, Tseng LM, et al. Sonographic features of nonpalpable breast cancer: a study based on ultrasound-guided wire-localized surgical biopsies. Ultrasound Med Biol. 2006. 32:1299–1306.

14. Kasumi F, Tanaka H. Jellins J, Kobayashi T, editors. Detection of microcalcifications in breast carcinoma by ultrasound. Ultrasound examination of the breast. 1983. New York: John Wiley & Sons;89–97.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download