Abstract
Takayasu arteritis is a chronic vasculitis involving the large vessels. At diagnosis, ischemic symptom are usually present in the affected vessels. However, fever of unknown origin (FUO) is rare as an initial presentation and renders the condition difficult to diagnose. In this case report, we describe a patient who presented with a fever of unknown origin. A 68-year-old female was diagnosed with Takayasu arteritis after fluorodeoxyglucose (FDG) positron-emission tomography-computed tomography (PET-CT) was performed at the prepulseless stage. FDG PET-CT can assist in the early diagnosis of Takayasu arteritis patients with FUO and can improve the prognosis of such patients.
Takayasu arteritis is a chronic vasculitis that affects large vessels, including the aorta and the principal branches thereof. The etiology of the condition is poorly understood, but it is thought that abnormalities of the immune system play important roles in triggering inflammation. The prevalence of the condition is high in asian countries, particularly in females of reproductive age [1].
Inflammation and destruction of blood vessels may cause vascular narrowing and occlusion in Takayasu arteritis patients, culminating in a pulseless stage. However, earlier (i.e., in the prepulseless stage), patients may initially present with nonspecific symptoms including fever, malaise, and myalgia [2]. Diagnostic criteria were developed in 1990 by the American College of Rheumatology, and the gold diagnostic standard is angiographic confirmation of narrowing or occlusion of the aorta, branches thereof, or large arteries [2]. Differential diagnosis should include other causes of large-vessel vasculitis, including syphilis and giant cell arteritis.
Takayasu arteritis rarely presents as fever of unknown origin (FUO). Here, we report such a case of Takayasu arteritis diagnosed at the prepulseless stage using non-invasive imaging.
A 68-year-old female was admitted with fever and general weakness. The fever had developed 2 months prior, was persistent, over 38℃, and spiked 2-3 times per day with accompanying chills and headache. She thought she had caught a common cold and was observed for some time with prescription of antipyretics. The fever did not subside after 1 month and she was admitted to another hospital.
The patient had been generally well despite her fever and chills. Her blood pressure and pulse were normal. No bacteria were cultured from blood. Extended spectrum beta lactamase-negative Escherichia coli was isolated from the initial urine culture, but the fever did not subside after administration of appropriate antibiotics and conversion of urine culture status to negative. Computed tomography (CT) of the chest and abdomen revealed that the abdomen was normal, but diffuse thickening of the aortic wall, without significant narrowing or occlusion of vessels, was evident. Cerebrospinal fluid analysis and transesophageal echocardiography yielded normal results. No symptomatic improvement was evident and she was transferred to our hospital for further evaluation of the origin of fever.
On admission, she had a febrile sense, chills, and anorexia, but no change in body weight. She denied experiencing neck stiffness, tinnitus, dizziness, sweating, chest discomfort, dyspnea, symptoms of upper respiratory or urinary tract infection, claudication, arthralgia, or joint swelling. She had taken antihypertensive medication commencing 5 years prior and had no known drug or food allergies. She was a retired teacher and lived in a city. She consumed alcohol once or twice per month and did not smoke.
On examination, her temperature was 38.9℃, her blood pressure 136/66 mmHg, and her pulse 84 beats per minute. The respiratory rate was 20 breaths per minute, and the oxygen saturation 96% when ambient air was breathed. She appeared tired when the fever spiked, but otherwise did not appear to be ill. Her heart and breathing sounds were normal. Neither the liver nor spleen was palpable and no palpable lymph node could be found. The peripheral pulse was intact, palpable, and present bilaterally at the carotid, brachial, radial, popliteal, and dorsalis pedis artery. No skin rash, petechial development, joint swelling, or tenderness was evident. All other examination was normal.
Laboratory examination indicated that anemia was present (hemoglobin 9.5 g/dL) in the absence of leukopenia or thrombocytopenia (white blood cell count 7,600/mm3, platelet count 498,000/mm3). The erythrocyte sedimentation rate was 82 mm/hr and the C-reactive protein level 7.08 mg/dL. Blood cultures and serologic markers for hepatitis B, hepatitis C, human immunodeficiency virus, and syphilis were all negative. The serum protein/albumin ratio was elevated (being 6.3/2.6), accompanied by rouloux formation when a peripheral blood smear was performed. Bone marrow examination revealed no specific abnormality.
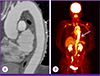
The inflammatory focus was sought using FDG positron-emission tomography-computed tomography (PET-CT) imaging; significant radiolabel uptake was evident along the walls of the aorta (Fig. 1A and B) and the large vessels (Fig. 2A and B). The fever subsided several days after commencement of systemic steroids. The elevated levels of inflammatory markers fell and the peripheral blood smear became normal. Our patient was discharged, and, after 1 year of outpatient follow-up, shows no evidence of disease progression.
Takayasu arteritis is a systemic vascular inflammatory disease of unknown etiology, although autoimmunity may be involved [3]. Panarteritis may involve all layers of the arterial wall and progress to wall thickening or stenosis. Ischemic symptoms develop because of vascular insufficiency associated with stenosis and thrombosis of the affected vessels. Disease presentations are variable, although absence or asymmetry of the peripheral pulse, and asymmetric blood pressure readings, are common. Unusual initial presentations include the Horner syndrome, bilateral cataracts, and malignant hypertension of affected arteries. Constitutional symptoms such as fever or malaise are observed in fewer than 50% of patients, but fever develops in 20-30% of patients over the course of disease. Fever is not a common initial presentation, being reported in fewer than 20% of patients. Fever of unknown origin present at the time of diagnosis is much rarer [4].
In 1989, Wu et al. [5] described a 26-year-old female with fever and myalgia who was diagnosed with Takayasu arteritis only after a delay of months, during which time vascular deformation had occurred. In Korea, Oh et al. [6] also reported a case of Takayasu arteritis presenting as fever of unknown origin.
In our case, fever of unknown origin was sustained for 2 months and we conducted a laboratory evaluation and performed serological tests and culture studies. Culture studies were negative and no focus of infection identified by repeated physical examination. From the results, we considered that the fever did not have an infective source. Chest CT revealed diffuse thickening of the aortal walls, with absence of calcification. This suggested that the thickening was caused by an inflammatory condition such as aortitis, rather than atherosclerosis. FDG PET-CT revealed diffuse hypermetabolism of the walls of the aorta and large vessels consistent with Takayasu arteritis. The fever subsided after steroid administration. No vascular complications were noted during 12 months of follow-up.
Previous studies showed that FDG PET-CT was valuable when used to assess the etiology of FUO, being associated with high sensitivity, a good positive predictive value, and a high negative predictive value [7]. FDG PET-CT facilitates early diagnosis, reducing the need for conduct of other unnecessary tests, and hospitalization costs [8].
FDG PET-CT is valuable when used to diagnose large vessel vasculitis. Angiography remains the gold standard but the procedure is invasive and the results are unreliable if tests are conducted in the prepulseless phase. FDG PET-CT is noninvasive and can detect prestenotic lesions, thus facilitating early diagnosis. There were reported cases of usefulness of FDG PET-CT in the diagnosis of large-vessel vasculitis in patients with FUO [910]. FDG PET-CT can identify the extent of vasculitis, and scoring of FDG uptake correlates well with measures of disease activity markers. Compared to magnetic resonance imaging which is also noninvasive, FDG PET-CT identifies more inflammatory lesions especially in patients with large-vessel vasculitis and is more reliable when used to assess disease activity during the course of immunosuppressive therapy [11]. Improvements in diagnostic modalities facilitating early diagnosis have significantly decreased the extent of vascular complications in patients with Takayasu arteritis [12]. In our patient, early diagnosis contributed to improvement of the symptoms and prevented development of vascular complications.
If a patient presents with FUO, FDG PET-CT can be usefully employed to detect regions of inflammation and to evaluate disease activity. Further, vasculitis can manifest as FUO and early diagnosis with the aid of FDG PET-CT improves patient prognosis.
Figures and Tables
Figure 1
Chest CT revealed thickening of the aortal wall (arrow) (A) whereas the FDG PET-CT scan revealed intense radiolabel uptake by the walls of the ascending and descending aorta (arrow) (B).
CT, computed tomography; FDG PET-CT, fluorodeoxyglucose positron emission tomography-computed tomography.
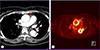
Figure 2
Chest CT revealed diffuse thickening of the aortic arch and the thoracic aorta (arrow) (A), whereas the FDG PET-CT scan revealed high-level radiolabel uptake by aortal wall regions corresponding to the areas that were diffusely thickened on chest CT. FDG PET-CT imaging also revealed increased glucose uptake by the walls of the subclavian arteries (arrow) (B).
CT, computed tomography; FDG PET-CT, fluorodeoxyglucose positron emission tomography-computed tomography.
References
2. Arend WP, Michel BA, Bloch DA, Hunder GG, Calabrese LH, Edworthy SM, Fauci AS, Leavitt RY, Lie JT, Lightfoot RW Jr, Masi AT, McShane DJ, Mills JA, Stevens MB, Wallace SL, Zvaifler NJ. The American College of Rheumatology 1990 criteria for the classification of Takayasu arteritis. Arthritis Rheum. 1990; 33:1129–1134.

3. Arnaud L, Haroche J, Mathian A, Gorochov G, Amoura Z. Pathogenesis of Takayasu's arteritis: a 2011 update. Autoimmun Rev. 2011; 11:61–67.

4. Kerr GS, Hallahan CW, Giordano J, Leavitt RY, Fauci AS, Rottem M, Hoffman GS. Takayasu arteritis. Ann Intern Med. 1994; 120:919–929.

5. Wu YJ, Martin B, Ong K, Klein NC, Cunha BA. Takayasu's arteritis as a cause of fever of unknown origin. Am J Med. 1989; 87:476–477.

6. Oh MD, Ko EM, Suh C, Choi SJ, Choe KW. Fever of undetermined origin (FUO) as a presenting symptom of Takayasu arteritis. J Korean Med Assoc. 1986; 29:1018–1022.
7. Keidar Z, Gurman-Balbir A, Gaitini D, Israel O. Fever of unknown origin: the role of 18F-FDG PET/CT. J Nucl Med. 2008; 49:1980–1985.

8. Becerra Nakayo EM, García Vicente AM, Soriano Castrejón AM, Mendoza Narváez JA, Talavera Rubio MP, Poblete García VM, Cordero García JM. Analysis of cost-effectiveness in the diagnosis of fever of unknown origin and the role of 18F-FDG PET-CT: a proposal of diagnostic algorithm. Rev Esp Med Nucl Imagen Mol. 2012; 31:178–186.

9. Akin E, Coen A, Momeni M. PET-CT findings in large vessel vasculitis presenting as FUO, a case report. Clin Rheumatol. 2009; 28:737–738.

10. Tatò F, Weiss M, Hoffmann U. Takayasu's arteritis without manifest arterial stenoses as a cause of fever of unknown origin. Dtsch Med Wochenschr. 2006; 131:1727–1730.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download