Abstract
Domestic human hydrophobia has not been reported since the one case of 2004 in South Korea, but still a few animal rabies occur persistently since the reemerging stage of rabies from 1993. The government has made efforts to control animal rabies in many aspects, but whether prophylactic strategy for human hydrophobia is performed adequately is in question. The rate of proper post-exposure prophylaxis for animal bite case in 'high-risk region' of rabies is very low with 20% between 2011 and 2013. The National Animal Bite Patient Surveillance targeting 'high-risk region' is missing out animal bite cases who visit directly to hospitals in 'suspect-risk region' of rabies. Little data seems to exist for pre-exposure prophylaxis of domestic hydrophobia. Danger of reoccurrence of human hydrophobia always remain in South Korea. The medical personnel needs to have greater interest on the matter and the government strengthen the management system.
Human hydrophobia (animal rabies) is a well-known zoonosis with a case-fatality rate approaching 100%. The estimated annual 60,000 human deaths occur from rabies, and most cases are in Africa and Asia [1, 2], but most clinicians nowadays in Korea is not familiar with hydrophobia because it has not been occurred since the one case of 2004. Animal rabies occur persistently even though a few yearly, and the government has made an efforts for control animal rabies in many aspects. However, whether prophylactic strategy for hydrophobia is performed adequately is in question. Epidemiology of rabies and hydrophobia, and prophylaxis in South Korea will be reviewed in this article, and just domestic occurrence covered.
Animal rabies in Korea are categorized into 'Enzootic stage', 'Decreased and elimination stage' and 'Reemerging stage' [3, 4]. 'Enzootic stage' accounts for the period from 1907, the first reported case of domestic rabies, to 1945. During this period 200 to 800 cases were reported every year in wild animals and live stocks nationwide. 'Decreased and elimination stage' describes the period after the emancipation where animal rabies gradually decreased since the launch of rabies vaccination program. Of this period, animal rabies to 1984 were limited to 1-91 cases annually near the De-Militarized Zone (DMZ), and there were no reports until the 'Re-emerging stage' which was began with rabies in a dog in 1993, from Cherwon-gun, Gangwon province. Cases of rabies for 10 years from 2004 to 2013 are shown Table 1. In 'Reemerging stage', animal rabies were limited to northern Gyonggi province and Goseong, Inje, Sokcho and other areas of Gangwon province until 2011. In 2012 there were reports of the disease from areas unreported, which are Suwon and Hwaseong of Gyeonggi province. This brought concerns about whether high-risk region of rabies is widening to south past Yeongdong expressway and Han River, considered as the natural barrier to the disease [5, 6]. Areas where animal rabies are reported from 2004 to 2013 is shown in the Table 2.
Susceptibility to rabies virus differs on some degree according to animal species [7] (Table 3). Whereas dogs function as reservoir for rabies virus in developing countries, foxes, skunks, raccoons, bats and such wild animals pose as problems for developed countries [8]. China, geographically near Korea has Chinese ferret badger, raccoon dog and bats for main reservoir for infection [9]. Raccoon dogs (Nyctereutes procyonoide) in canine family play a key role in transmitting rabies to cattle and dogs in Korea. When conducted studies of conditions for rabies infection on 54 wild animals of 8 different species, captured in the area bordering the DMZ during 3 years term from December 1998, of the studied wild animals only racoon dogs were positive for rabies virus antigen with positive rate of 32% [10]. Other studies reported that 21 of 61 captured or dead Korean racoon dogs were positive for rabies and their geographic distribution was almost identical to the areas where cases occurred in cattle and dogs [11, 12]. Most reported cases of rabies virus since 1993 to present were from cattle, dogs, and racoon dogs in the described order.
As rabies virus cause hydrophobia to humans by animal bites, measures to keep wild animals, cattle, and companion dogs or cats from being infected with rabies virus will be the first step for the prevention of human rabies. Thoroughly conducted vaccination is the most important above all. Companion animals such as dogs and cats in urban areas must be vaccinated for animal rabies yearly. Farms in areas vulnerable to or already reported with animal rabies must have dogs and cattle in households vaccinated. Strict prevention of contacts between cattle and raccoon dogs, carriers of rabies virus, is also very important [13, 14].
One of the injection rabies vaccines used domestically nowadays is a live vaccine produced with attenuated live vaccine strain Evelyn-Rokitnicki-Abelseth, and is used only on livestock such as dogs, cattle, sheep and horse [15]. Inactivated rabies vaccines for immunizing pets and other animal species, including dogs, cats, cattle, goats, and fox have been used to prevent animal rabies. Nerve tissue vaccine, which is an inactivated vaccine, was advised to be replaces to cell-culture rabies vaccine due to side effects by World Health Organization (WHO) in 2005 [16]. Nerve tissue vaccine is no longer used domestically for poor immunity and safety issues. Modified live oral rabies bait vaccine has been produced for free-ranging animals and wildlife species [17].
In the companion animal (dog and cat) section, the government supplies injection vaccine to local veterinary clinics through local governments every spring and fall. But fixed seasons (spring, fall) and short periods (2 weeks) every year prevents adequate timing of boosting injection. In the farm animal (cattle) section, inactivated vaccine and live vaccines are supplied for farms in rabies-occurring region and non-outbreak region, respectively. But most farmers shares negative feelings towards cattle rabies vaccination for several reasons such as side effects of vaccination and no obligatory vaccine certificate for trade. The guard dogs and abandoned animals (dogs and cat) are exposed to rabies infection because they easily come into contact with racoon dogs. Plans to regulate their population and vaccination are required [6]. A large amount of bait vaccine, vaccinia-rabies glycoprotein recombinant virus (VRG) vaccine, has been distributed for wild racoon dogs in Korea since 2000. Sufficient supply of bait vaccine based on density of raccoon dogs is needed. Unfortunately the VRG bait vaccine is not effective in skunks and dogs [18]. Thorough animal vaccination is the primary measure to prevent human hydrophobia.
In 1960s there were various reports of occurrences on a yearly basis (1-103 cases), and in 1970s the reports decreased dramatically to 0-13 cases yearly. For 14 years after respectively 1 case in 1982 and in 1984, there have been total of 6 cases up to 2004 including 1 case of reoccurrence in 1999. There have been no reports of the occurrence in the past decade leading to 2014 [19].
As for Korea, government categorized into 'high-risk region' where any one case of rabies or hydrophobia has been occurred since reemerging stage and 'suspect-risk region'. High-risk region of rabies are 19 areas of which are Gangwon province (Goseong, Sokcho, Yanggu, Yangyang, Inje, Cheorwon, Chuncheon, Hwacheon and Hongcheon), Gyeonggi province (Gapyung, Goyang, Gimpo, Dongducheon, Yangju, Yangpyeong, Yeoncheon, Paju and Pocheon) and Eunpyeong-gu, Seoul. Suspect-risk region account for areas bordering high-risk region. Since the reoccurrence of animal rabies in 2012 of Suwon and Hwaseong of Gyeonggi province, corresponding areas have been added to high-risk region [20].
Korean Centers for Disease Control and Prevention (KCDC) is operating the National Animal Bite Patient Surveillance from 2005 in high-risk region of rabies of Gyeonggi and Gangwon province [21]. However, suspect-risk region is not covered in this Surveillance. Three hundred fifty-nine people were bitten in 2005, 463 in 2006, 449 in 2007, 529 in 2008, 658 in 2009, 641 in 2010, 638 in 2011, 606 in 2012 and 552 in 2013. In 2013, areas with the most number of bitten people out of every population of a hundreds of thousands were Yeoncheon, Yangju and Gapyeong of Gyeonggi province, and Yanggu, Goseong, Sokcho and Cheorwon of Gangwon province. Of the number of inflicting animals the most frequent was dogs (82.1%), followed by cats (11.4%). Injuries by raccoon dogs, known as the natural reservoir for domestic rabies virus, only accounted for 0.2% [22].
From the injuries during the recent 3-years period (2011-2013), tests have been conducted on sum of 50 of inflicting animals. Nine of these were positive for rabies virus (18%), including 8 household dogs and 1 raccoon dog. All 9 of the bitten patients received adequate post-exposure prophylaxis and thus the injury did not progress to hydrophobia [22, 23].
As shown above patients with injuries and post-exposure prophylaxis of high-risk region are well realized but flaws may exist for the patient control of suspect-risk region of rabies. This leads directly to the problem with hydrophobia prevention. From 2009 to 2013, total of 131 patients with dog bites had visited the affiliated teaching hospital in Uijeongbu, included in suspect-risk region adjoin to high-risk regions of rabies in northern Gyeonggi province. Out of these patients, 64 (48.9%) of them were bitten in high-risk region. Two patients transferred from hospitals in high-risk region and the rest of 62 visited directly to the hospital in susepect-risk region immediately after the injury. This hospital is not covered in National Animal Bite Patient Surveillance, and is thus missed from the statistics for animal bite case and also from the management of whether timely post-exposure was conducted. Only 10% of the 131 patients were treated with proper post-exposure prophyaxis (data, not shown). National Animal Bite Patient Surveillance will require taking into consideration factors such as geographical circumstances and accessibility to medical facilities. If the range of Surveilllance is able to encompass regions as this, we can get the more correct number of reports on animal bites occurring in high-risk region.
Despite the large number of animal bite cases in high-risk region and the annual occurrence of animal rabies, actual hydrophobia patients have not surfaced for the last decade. Animal vaccination is thought to be the most influential factor in this. It is very fortunate that 9 bitten patients by rabies positive animals in recent 3 years (2011-2013) were treated adequately and have not progressed to hydrophobia [22, 23]. However, the rate of proper post-exposure prophylaxis after animal biting injury is not high in Korea.
Adequate management for biting injuries regarding the categories of exposure, advised by WHO, is shown in Table 4 [24]. When categorized animal biting wounds occurred in 2011 and 2012, WHO class III was 81.21%, class II was 11.55% and class I was 0.48%. Case of complete post-exposure prophylaxis regarding all categories of wounds was only 22.6% [23]. Complete post-exposure prophylaxis in 2013 was conducted on a low level as well, of merely 18.8% [22]. None of 6 hydrophobia patients occurred since 1999 had received proper post-exposure prophylaxis (Table 5), and all patients were dead [25].
There should be several reasons for the failure of performing adequate post-exposure prophylaxis. Medical personnel treating bitten patients on the frontline may have certain difficulties in the knowledge and awareness of hydrophobia. Obscure fear towards side effects of rabies vaccine and rabies immunoglobulin may pose a problem as well. In addition, the inconvenience of injecting multiple does of vaccines, the high costs of vaccine and immunoglobulin, and the scarcity of the medicine for those outside high-risk region, as it is supplied only by Korean Orphan Drug Center, will be several reasons why. Medical personnel on the frontline, including suspect-risk region as well as high-risk region, requires education. One must keep in mind that while the adverse events to the vaccine may arise, but the only prevention is by post-exposure prophylaxis otherwise the disease will lead to death. Thus hesitation to perform complete post-exposure prophylaxis must be eliminated.
Purified Vero cell culture rabies vaccine (PVRV, Verorab®) currently used in Korea is injected on once every 0, 3rd, 7th, 14th, 28th day for the total of 5 times. In July 2010, CDC of the United States modified the proposal of recommendation for human diploid vaccine and purified chick embryo cell culture vaccine to be injected once every 0, 3rd, 7th, 14th day to the total of 4 times, but has not modified the recommendation for PVRV [26]. When humans with existing immunity are exposed to dangers of animal rabies, only booster vaccines on 0, 3rd day for twice without immunoglobulin is sufficient. In mostly countries with high rate of animal rabies, researches are being implemented to lower the frequency of vaccine injections [27].
Park et al. [28] reported 371 animal bite cases abroad from 2006 to 2012 visiting the International Travel Clinic of the National Medical Center in Korea, and the regions of exposure were mostly Southeast Asia. Animal bite cases in overseas travelers are high than expected.
WHO recommend pre-exposure prophylaxis for anyone who is at continual, frequent or increased risk to exposure to the rabies virus [24]. KCDC recommends vaccination to veterinarians, to workers of animal hospitals, to animal handlers, to hydrophobia researchers, to animal research lab workers, to people with frequent contacts with hydrophobia-prone mammals such as bats, raccoons, skunks, cats, and dogs, and lastly to people travelling overseas to regions with high rate of hydrophobia and no proper medical facilities (for those who stay over 1 month, are unable to immediately use medical facilities and are more likely to be exposed to rabies virus due to the nature of activities in the region) [29]. Korean Society of Infectious Diseases specifically mentions soldiers stationed near the DMZ in addition to the recommendations of KCDC [30]. In Korea high-risk region of rabies is mostly near the DMZ and placed soldiers, members of relief organization for wild animals, and veterinarians are in the high-risk group [25].
However, vaccination rate is expected to be extremely low, although no detailed domestic data of how much pre-exposure vaccination is being used to the high-risk group. Pre-exposure prophylaxis is even more emphasized with children living in countries where canine rabies is highly endemic, but the fact that pre-exposure vaccination rate is low in these areas is also a problem [31].
As for domestic high-risk group, sufficient implementation of pre-exposure prophylaxis will be most ideal. But in environment as Korea where hydrophobia is very rare, post-exposure prophylaxis seems more practical.
Although for the past decade there was no hydrophobia patients, danger of reoccurrence always exists. Animal vaccination is the most important measure to keep wild animals, cattle, and companion dogs or cats from getting rabies. Frontline medical personnel must heed more attention to the management of animal bite patients and be cautious not to miss the proper post-exposure prophylaxis. Government must place more interest in managing rabies in suspect-risk region including easy medicinal supplies and personnel education. Rabies pre-exposure prophylaxis on the high-risk group is in need of examination.
Figures and Tables
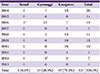
Table 1
Animal rabies in South Korea by year (2004-2013)

Data source: KAHIS program (www.kahis.go.kr) from Animal and Plant Quarantine Agency.
Table 2
Animal rabies in Seoul, Gyeonggi and Gangwon Province (2004-2013)
Data source: KAHIS program (www.kahis.go.kr) from Animal and Plant Quarantine Agency.
aEunpyeong-gu, Seoul.
bincluding Suwon- and Hwaseong-si, Gyeonggi province.
References
1. Fooks AR, Banyard AC, Horton DL, Johnson N, McElhinney LM, Jackson AC. Current status of rabies and prospects for elimination. Lancet. 2014; pii: S0140-6736(13)62707-5.

2. Song M, Tang Q, Rayner S, Tao XY, Li H, Guo ZY, Shen XX, Jiao WT, Fang W, Wang J, Liang GD. Human rabies surveillance and control in China, 2005-2012. BMC Infect Dis. 2014; 14:212.

3. Hwang EK. Outbreak and control of rabies in animals in Korea. Korean J Vet Public Health. 1995; 19:281–293.
4. Kim CH, Lee CG, Yoon HC, Nam HM, Park CK, Lee JC, Kang MI, Wee SH. Rabies, an emerging disease in Korea. J Vet Med B Infect Dis Vet Public Health. 2006; 53:111–115.

5. Yang DK, Kim SY, Oh YI, Lee JA, Cho SD, Lee KW, Song JY. Epidemiological characteristics of rabies in South Korea from January 2004 to March 2011. J Bacteriol Virol. 2011; 41:165–171.

6. Cheong Y, Kim B, Lee KJ, Park D, Kim S, Kim H, Park E, Lee H, Bae C, Oh C, Park SY, Song CS, Lee SW, Choi CS, Lee JB. Strategic model of national rabies control in Korea. Clin Exp Vaccine Res. 2014; 3:78–90.

7. Baer GE, Bellini WJ, Fishbein DB. Rhabdoviruses in Virology. 2nd ed. New York: Raven press;2002. 190:p. 883–930.
8. Hankins DG, Rosekrans JA. Overview, prevention, and treatment of rabies. Mayo Clin Proc. 2004; 79:671–676.

9. Wang L, Tang Q, Liang G. Rabies and rabies virus in wildlife in mailnland China, 1990-2013. Int J Infect Dis. 2014; 25:122–129.
10. So BJ, Jean YH, Lee SJ, Lee ED, Lee KK, Hwang EK, Lee SK, Kim JH, Park CK, Yoon SS, Kim KS, Moon OK, Shin MK, Lee SS. Rabies infectious situation in wild animals of Kyonggi and Kangwon provinces in the Republic of Korea. Korean J Vet Public Health. 2002; 26:115–120.
11. Kim JH, Hwang EK, Sohn HJ, Kim DY, So BJ, Jean YH. Epidemiological characteristics of rabies in South Korea from 1993 to 2001. Vet Rec. 2005; 157:53–56.

12. Hwang EK. Outbreaks and control of rabies in animals in Korea: a review. Korean J Vet Public Health. 1995; 19:281–293.
13. Park JS, Han MG. General features and post-exposure prophylaxis of rabies. Infect Chemother. 2010; 42:6–11.

15. Faber M, Dietzschold B, Li J. Immnunogenicity and safety of recombinant rabies viruses used for oral vaccination of stray dogs and wildlife. Zoonoses Public Health. 2009; 56:262–269.

16. World Health Organization (WHO). WHO Expert Committee on Rabies, 2004. First report, WHO technical report series no.931. Geneva, Switzerland: WHO;2005. p. 13.
17. Wiktor TJ, Macfarlan RI, Reagan KJ, Dietzschold B, Curtis PJ, Wunner WH, Kieny MP, Lathe R, Lecocq JP, Mackett M. Protection from rabies by a vaccinia virus recombinant containing the rabies virus glycoprotein gene. Proc Natl Acad Sci U S A. 1984; 81:7194–7198.

18. Yang DK, Kim HH, Lee KW, Song JY. The present and future of rabies vaccine in animals. Clin Exp Vaccine Res. 2013; 2:19–25.

19. Ministry of Health and Welfare, Korea Centers for Disease Control and Prevention. Infectious diseases surveillance yearbook. 2013.
20. Korea Cenetrs for Disease Control and Prevention. Human rabies prevention & control. 2007.
21. National Animal Bite Patient Surveillance. Comprehensive surveillance system of diseases and health. Accessed 1 September 2014. Available at: http://is.cdc.go.kr.
22. Park JS, Kim SY, Hwang KJ. Animal bite cases in high-risk region of rabies, 2013. Public Health Wkly Rep. 2014; 7:713–719.
23. Park JS, Kim SY. Animal bite cases in high-risk region of rabies, 2011-2012. Public Health Wkly Rep. 2013; 6:465–470.
24. World Health Organization (WHO). WHO guide for rabies pre and post-exposure prophylaxis in human(updated 2013). Accessed 12 September 2014. Available at: http://www.who.int/rabies/WHO_Guide_Rabies_Pre_Post_Exposure_Prophylaxis_Humans_2013.pdf?ua=1.
25. Korea Centers for Disease Control and Prevention (KCDC). Public strategy development for civils and medicals. Seoul: KCDC;2007.
26. Rupprecht CE, Briggs D, Brown CM, Franka R, Katz SL, Kerr HD, Lett SM, Levis R, Meltzer MI, Schaffner W, Cieslak PR. Centers for Disease Control and Prevention (CDC). Use of a reduced (4-dose) vaccine schedule for postexposure prophylaxis to prevent human rabies: recommendations of the advisory committee on immunization practices. MMWR Recomm Rep. 2010; 59:1–9.
27. Permpalung N, Wongrakpanich S, Korpaisarn S, Tanratana P, Angsanakul J. Trend of human rabies prophylaxis in developing countries:toward optimal rabies immunization. Vaccine. 2013; 31:4079–4083.

28. Park JH, Lee CH, Won YK, Chin BS, Shin HS, Kim JY. Rabies post-exposure of overseas travelers in the international travel clinic of the national medical center from 2006 to 2012, Korea. Infect Chemother. 2014; 46:13–20.

29. Korea Centers for Disease Control and Prevention (KCDC). Epidemiology and prevention of vaccine-preventable disease. 4th ed. Chungwon: KCDC;2013. p. 453.
30. Korean Society of Infectious Disease. Vaccination for adult. 2nd ed. Seoul: MIP;2012. p. 58.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download