Abstract
Purpose
To evaluate the diagnostic value of the Korean version of the Douleur Neuropathique 4 (DN4) questionnaire and to validate this questionnaire in terms of psychometric properties in patients with chronic pain due to degenerative spinal disease.
Materials and Methods
The Korean version of the DN4 questionnaire, which was translated and linguistically validated by the MAPI Research Group, was tested on 83 patients with lumbar or lumbar-radicular pain. Test-retest reliability was evaluated in a subsample of 40 patients who completed two assessments with an interval of 2 weeks. Nociceptive pain and neuropathic component pain were diagnosed in 40 and 43 patients, respectively.
Results
The Cronbach's α coefficient of internal consistency was 0.819, and the test-retest intraclass correlation coefficient (3, 1) (95% confidence interval) was 0.813 (0.776–0.847) (n=40). The area under the receiver-operator characteristics curve was 0.953 (p<0.001), with 95% confidence interval between 0.869 and 0.990. The Korean version of the DN4 questionnaire showed a sensitivity of 100% and 87.1%, and a specificity of 88.2% and 94.1% at the cutoff value of 3/10 and 4/10, respectively, for discriminating neuropathic component pain.
The management of neuropathic pain has been highlighted for the treatment of degenerative spinal disease. Not only ischemia in nerve tissue but also a neuropathic pain mechanism was implicated in the genesis of leg pain in patients with degenerative spinal disease because compressed nerve roots exhibit edema, fibrosis, demyelination, and axonal degeneration of the involved neural element.123 Therefore, pharmacological treatment should be aimed at the management of the neuropathic component of pain for the effective treatment of degenerative spinal disease.45
For this treatment approach, proper assessment of the neuropathic pain component in degenerative spinal disease is imperative, and discrimination or subcategorization according to the presence of neuropathic pain in patients with degenerative spinal disease is a prerequisite. Hitherto, several questionnaires have been used for the assessment of neuropathic pain, including the Leeds Assessment of Neuropathic Symptoms and Signs Pain Scale, the ID Pain, Neuropathic Pain, painDETECT, and Douleur Neuropathique 4 (DN4) questionnaires.678910
The DN4 questionnaire was developed by the French Neuropathic Pain Group as a clinic-based instrument for identifying patients whose pain has a predominantly neuropathic mechanism,911 and was designed as an easy-to-use diagnostic questionnaire and is composed of 10 "yes" or "no" items; seven items are related to pain quality (i.e., sensory and pain descriptors) based on interviews with patients, whereas three items are based on clinical examination and are related to the presence or absence of touch or pinprick hypoesthesia and tactile allodynia. The total score is calculated as the sum of all 10 items, and the cutoff value for the diagnosis of neuropathic pain is a total score of 4/10.9 The DN4 questionnaire has been shown to have very good sensitivity (83%) and specificity (90%) for the identification of chronic pain associated with a lesion in the nervous system (either peripheral or central).912
Nevertheless, to apply or use this assessment tool in non-English speaking countries, the questionnaires should undergo a standardized process of translation, cross-cultural adaptation, and psychometric validation in terms of its ability to take into account culture-specific conditions.13 The analysis of psychometric validation included reliability (internal consistency, inter-rater agreement) and validity (receiver operating characteristics curve) analysis. Even though the DN4 questionnaire has been translated linguistically,14 the psychometric validation of the Korean version of the DN4 questionnaires was not performed yet.1112151617 We hypothesized that the present linguistically validated DN4 would have good psychometric properties. Therefore the objectives of this study were to evaluate the diagnostic value of the Korean version of the DN4 questionnaire and to validate this questionnaire in terms of psychometric properties in patients with chronic pain due to degenerative spinal disease.
The study was approved by the hospital institutional review board. The study was designed as an observational, prospective collected data and retrospective analysis. All data, including the DN4 questionnaire results, were recorded as part of the routine care of patients with lumbar or lumbar-radicular pain due to degenerative lumbar disease. Therefore, we did not take the signed informed consent. The inclusion criteria were patients 1) from 35 to 85 years old: this age criterion was decided considering the capability to understand the questionnaires; 2) visiting the outpatient's facilities for chronic lumbar and/or lumbar-radicular pain due to degenerative spinal disease; 3) with a pain duration of ≥3 months, because the present study dealt with chronic pain; 4) with moderate or severe pain intensity [scoring 4 or higher on the Visual Analogue Scale (VAS) for back or leg pain]; and 5) who are native Korean speakers.
The exclusion criteria were patients with other severe musculoskeletal pain, major comorbidity (e.g., malignant disorders or sepsis), fibromyalgia, headache or visceral pain, cognitive impairment or intellectual disability, and severe depression or psychosis. The study was carried out at the spine center of a tertiary-care teaching institution between November 2014 and January 2015. The Korean version of the DN4 questionnaire was used, which was translated and linguistically validated by the MAPI Research Group.18 The principal investigator who an expert in degenerative spinal disease and neuropathic pain, proposed the diagnosis of neuropathic component or nociceptive pain without the information from the DN4 questionnaire by using medical history taking and examination according to usual clinical practice. The diagnosis of the principal investigator was considered the gold standard. Before this gold standard diagnosis, a research coordinator, blinded to the diagnosis proposed by the principal investigator, administered the DN4 questionnaire. In addition, to investigate the test-retest reliability, a research coordinator administered the DN4 questionnaire for a second time in a subsample of 40 patients, 2 weeks after the first. For inter-rater reliability, the DN4 questionnaire was administered twice in a subsample of 30 patients by an another investigator. Between the two visits, patient underwent further radiological examinations such as plain X-ray and/or magnetic resonance image of lumbar spine. If necessary, patient took medications such as non-steroid anti-inflammatory drugs (NSAIDs) or acetaminophen.
Internal consistency was evaluated, by using the Cronbach's α coefficient, to assess the contribution of each item to the concept measured by the questionnaire. Cronbach's α was first assessed for the complete questionnaire; then, each item was removed to assess the independent contribution of each item to the measurement error of the instrument. For inter-rater reliability, the Cohen's kappa coefficient was used to measure the agreement of the results obtained by two different raters for each item and for the total score of the DN4 questionnaire. The test-retest reliability was assessed by comparing the replies in the first and second administrations of the DN4 questionnaire in a subsample of subjects (n=40), by using the intraclass correlation coefficient (ICC). In addition, we calculated that a minimum sample of 88 patients would be required for the current study, with expected area under the curve (AUC) would be 0.7 and a ratio (negative/positive groups) of 1.5, based on an alpha of 0.05 and beta of 0.10. Receiver-operator characteristics (ROCs) analysis was done to assess the utility of the DN4 total score in distinguishing patients who had neuropathic component pain defined by the gold standard diagnosis of the principal investigator. The AUC and its 95% confidence intervals (CIs) for the ROC curve were calculated. The AUC is a measure of the diagnostic power of the test. An AUC of ≤0.60 is considered "negative"; 0.61 to 0.80, "doubtful"; 0.81 to 0.90, "good"; and ≥0.91, "very good."17 This also determined and set the ideal cutoff to provide the best sensitivity and specificity values for the diagnosis of neuropathic component pain and the determination of Youden's index. All statistical analyses were performed by using the SPSS 20.0.0 statistics package (SPSS Inc., Chicago, IL, USA). A value of p<0.05 was accepted as significant.
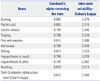
Between November 2014 and January 2015, 115 patients not previously examined by the principal investigator were evaluated at the spine center of a tertiary-care teaching institution and were eligible candidates to participate in this study. Of the 115 patients, 83 who met the inclusion criteria were included. On the other hand, 32 patients were excluded from the study: 15 patients had pain of <3 months' duration, 12 patients had other severe musculoskeletal pain and/or fibromyalgia, and 5 patients had major depression. Nociceptive pain and neuropathic component pain were diagnosed in 40 and 43 patients, respectively. Table 1 shows the baseline demographic data and characteristics of patients in each of the study groups. There were no differences in demographic characteristics between the two groups. Patients with neuropathic component pain showed a statistically significantly higher VAS score for leg pain than patients with nociceptive pain (p<0.001). The most common cause of nociceptive pain and neuropathic component pain was mechanical low back pain (87.5%) and spinal stenosis (62.8%), respectively. The mean DN4 score differed significantly between the two groups (p<0.001) (Table 1). There was a significant correlation between the total DN4 score and the VAS score for leg pain (r=0.521, p<0.001).
The Cronbach's α coefficient of the internal consistency of the Korean version of the DN4 questionnaire, which measures the extent to which items of a scale represent a common underlying variable, was 0.819. The Cronbach's α coefficients did not improve when each scale item was successively removed (values ranging from 0.788 and 0.818), justifying the contribution of each item to the concept evaluated by the questionnaire (Table 2). As for inter-rater reliability, Cohen's kappa coefficients for each item ranged from 0.823 to 0.946, and Cohen's kappa coefficient for total DN4 score was 0.84 (Table 2). In an interval of 2 weeks, the test-retest ICC (3, 1) (95% CI) was 0.813 (0.776–0.847) (n=40). Test-retest coefficients >0.7 are generally accepted as sufficient, and coefficients >0.8 are considered as good.19
The AUC measured was 0.953 (p<0.001) with 95% CI between 0.869 and 0.990, and a standard error of 0.031 (Fig. 1). The result confirms the high discriminant power of the Korean version of the DN4 questionnaire. In the assessment of the suitability of the cutoff point, the sensitivity and specificity tests, as well as Youden's index, indicated that 3 and 4 are the ideal cutoff values for the sum of scores obtained in the items of the DN4 questionnaire. The cutoff point of 3 simultaneously represents a sensitivity of 100%, specificity of 88.2%, and Youden's index of 0.882. Furthermore, the cutoff point of 4 simultaneously represents a sensitivity of 87.1%, specificity of 94.1%, and Youden's index of 0.812 (Fig. 1).
The present study demonstrated the good discriminatory power of the linguistically validated Korean version of the DN4 questionnaire, between nociceptive pain and neuropathic component pain in patients with lumbar or lumbar-radicular pain. It should be acknowledged that our study population included only patients with lumbar or lumbar-radicular pain due to degenerative lumbar disease. However, previous studies have shown that the neuropathic component of "mixed pain" has clinical characteristics similar to those of pure neuropathic pain.1220 In addition, previous studies have also proved that the DN4 questionnaire has a high discriminatory power between neuropathic component pain and nociceptive pain in patients with mixed pain.1216 Furthermore, almost all patients have spinal pathologies of neural elements such as nerve compression in the neuropathic component group, whereas all patients complained mechanical low back pain in the nociceptive group (Table 1). This result was consistent with a previous report regarding the redefining and grading of neuropathic pain,21 suggesting that the lesion of somatosensory system was prerequisite for diagnosis of neuropathic pain.
Table 2 shows the results of internal consistency of the instrument. Our results were slightly higher than that obtained with the other language versions of the DN4 questionnaire,11121516 underlining the importance of each questionnaire item. It is highly likely that this was due to the characteristic of participants of having a single disease entity (i.e., lumbar or lumbarradicular pain by degenerative spinal disease), whereas other previous studies dealt with various neuropathic diseases. However, when each item was removed, no increases in the total Cronbach's α coefficients were found in the present study (Table 2). Furthermore, inter-rater agreement was very good, showing the kappa coefficient ranging from 0.823 to 0.946.16
In this study, 40 patients completed the questionnaire twice with an interval of 2 weeks. Compared with the other language versions of DN4,111216 the ICC (3, 1) of the Korean version of DN4 was slightly lower. This is likely due to longer interval, disease characteristics of the participants, and initiation of medication during the interval. The longer interval is related to the deterioration of correlation coefficients.22 Furthermore, although degenerative spinal disease has the characteristics of chronic disease, its symptoms would have episodic and/or variable clinical manifestation during the natural course of the disease. In addition, the mediation of NSAIDs or acetaminophen for the assessment interval might relieve or change the patients' symptom. Therefore, these would also attribute to the lower correlation coefficient.
Identification of neuropathic components is critical to the medical treatment of degenerative spinal disease because the therapeutic approach for these patients should be different from that for patients with only nociceptive pain.22324 The present study showed that the Korean version of DN4 has excellent psychometric properties: we confirmed its high discriminative ability in patients with neuropathic component pain or nociceptive pain, with an AUC score of 0.953, a sensitivity of 100% and 87.1%, and a specificity of 88.2% and 94.1% at the cutoff values of 3/10 and 4/10, respectively. This finding is consistent with previous studies with other languages,111216 where the cutoff value for the DN4 questionnaire in most of them was established at 4/10. In the Dutch version of the DN4 questionnaire, 5/10 was considered as an ideal cutoff value.17 This disparity highlights the importance of analyzing the psychometric properties of the screening questionnaires in different languages, in addition to the linguistic validations. The present study showed two ideal cutoff values of 3/10 and 4/10. However, in view of the screening test, the cutoff value of 4/10 would be more ideal than 3/10, thus slightly differing from other validation finding.121516 These discrepancies may be explained by the differences in study design. As noted earlier, the present study included only patients with lumbar or lumbar-radicular pain. These patients did not present pure neuropathic pain, but rather "mixed pain" with a neuropathic component. Nonetheless, this study showed that the discriminatory ability of the Korean version of the DN4 questionnaire cannot be influenced by disease characteristics such as the mixed nature of pain. This also agrees with previous studies.1216
First, as previously noted, the current study included patients with lumbar or lumbar-radicular pain for the validation of the DN4 questionnaire. This feature is unique to this study. However, because there are many kinds of diseases causing neuropathic pain that should be assessed with the validated DN4 questionnaire, the narrow disease spectrum of the subjects such as degenerative lumbar disease is the main limitation of this study in view of generalizability. Furthermore, a recent study has reported redefinition and grading of neuropathic pain.21 According to this grading system,21 the patients of the neuropathic component group in the present study would range from possible to definite neuropathic pain. Recent studies have consistently emphasized the identification and treatment of neuropathic pain component for the treatment of degenerative spinal disease.223242526 In this perspective, the present study also highlights possible or probable neuropathic pain of degenerative spinal disease. Second, it has not yet been determined whether the DN4 questionnaire can be used to detect possible or probable neuropathic pain. However, since this study also demonstrated the successful implementation of the DN4 questionnaire, it is highly possible that DN4 can be implemented for discriminating possible or probable neuropathic pain even in lumbar or lumbar-radicular pain due to degenerative spinal disease, which is more common in real clinical settings. Furthermore, a previous study has also shown discriminating power for mixed pain.12 Finally, the gold standard decision of neuropathic pain by only one expert is an another limitation of this study. Most of the DN4 validation studies have used two experts to determine whether the pain was neuropathic/nociceptive or mixed.1617
In conclusion, the current study demonstrated the good discriminatory power of the Korean version of DN4 between nociceptive pain and neuropathic component pain in patients with lumbar or lumbar-radicular pain due to degenerative lumbar spine disease.
Figures and Tables
Fig. 1
ROC curve and AUC for the total score of the DN4 questionnaire: the figure shows the cut-off point of optimizing sensitivity and specificity values for discriminating between nociceptive pain and neuropathic component pain in patients with degenerative spinal disease. AUC, area under the curve; ROC, receiver operating characteristics; DN4, Douleur Neuropathique 4.

Table 1
Descriptive Statistics of the Subjects in the Study

Table 2
Cronbach's Alpha to the Items of the Instrument
ACKNOWLEDGEMENTS
This work (Grants No. C0248313) was supported by Business for Cooperative R&D between Industry, Academy, and Research Institute funded Korea Small and Medium Business Administration in 2014.
References
1. Sekiguchi M, Kikuchi S, Myers RR. Experimental spinal stenosis: relationship between degree of cauda equina compression, neuropathology, and pain. Spine (Phila Pa 1976). 2004; 29:1105–1111.
2. Takahashi N, Arai I, Kayama S, Ichiji K, Fukuda H, Kaga T, et al. Therapeutic efficacy of pregabalin in patients with leg symptoms due to lumbar spinal stenosis. Fukushima J Med Sci. 2014; 60:35–42.

3. Yaksi A, Ozgö;nenel L, Ozgönenel B. The efficiency of gabapentin therapy in patients with lumbar spinal stenosis. Spine (Phila Pa 1976). 2007; 32:939–942.

4. Lee SY, Kim TH, Oh JK, Lee SJ, Park MS. Lumbar stenosis: a recent update by review of literature. Asian Spine J. 2015; 9:818–828.

5. Baliga S, Treon K, Craig NJ. Low back pain: current surgical approaches. Asian Spine J. 2015; 9:645–657.

6. Bennett M. The LANSS Pain Scale: the Leeds assessment of neuropathic symptoms and signs. Pain. 2001; 92:147–157.

7. Portenoy R. Development and testing of a neuropathic pain screening questionnaire: ID Pain. Curr Med Res Opin. 2006; 22:1555–1565.

8. Krause SJ, Backonja MM. Development of a neuropathic pain questionnaire. Clin J Pain. 2003; 19:306–314.

9. Bouhassira D, Attal N, Alchaar H, Boureau F, Brochet B, Bruxelle J, et al. Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4). Pain. 2005; 114:29–36.

10. Freynhagen R, Baron R, Gockel U, TÖlle TR. painDETECT: a new screening questionnaire to identify neuropathic components in patients with back pain. Curr Med Res Opin. 2006; 22:1911–1920.

11. Harifi G, Ouilki I, El Bouchti I, Ouazar MA, Belkhou A, Younsi R, et al. Validity and reliability of the Arabic adapted version of the DN4 questionnaire (Douleur Neuropathique 4 questions) for differential diagnosis of pain syndromes with a neuropathic or somatic component. Pain Pract. 2011; 11:139–147.

12. Perez C, Galvez R, Huelbes S, Insausti J, Bouhassira D, Diaz S, et al. Validity and reliability of the Spanish version of the DN4 (Douleur Neuropathique 4 questions) questionnaire for differential diagnosis of pain syndromes associated to a neuropathic or somatic component. Health Qual Life Outcomes. 2007; 5:66.
13. Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976). 2000; 25:3186–3191.

14. Van Seventer R, Vos C, Meerding W, Mear I, Le Gal M, Bouhassira D, et al. Linguistic validation of the DN4 for use in international studies. Eur J Pain. 2010; 14:58–63.

15. Santos JG, Brito JO, de Andrade DC, Kaziyama VM, Ferreira KA, Souza I, et al. Translation to Portuguese and validation of the Douleur Neuropathique 4 questionnaire. J Pain. 2010; 11:484–490.

16. Sykioti P, Zis P, Vadalouca A, Siafaka I, Argyra E, Bouhassira D, et al. Validation of the Greek Version of the DN4 diagnostic questionnaire for neuropathic pain. Pain Pract. 2015; 15:627–632.

17. van Seventer R, Vos C, Giezeman M, Meerding WJ, Arnould B, Regnault A, et al. Validation of the Dutch version of the DN4 diagnostic questionnaire for neuropathic pain. Pain Pract. 2013; 13:390–398.

18. Bouhassira D. Neuropathic Pain 4 Questions (DN4). accessed on 2015 Feb 1. Available at: http://www.proqolid.org/instruments/neuropathic_pain_4_questions_dn4?fromSearch=yes&text=yes.
19. Lohr KN, Aaronson NK, Alonso J, Burnam MA, Patrick DL, Perrin EB, et al. Evaluating quality-of-life and health status instruments: development of scientific review criteria. Clin Ther. 1996; 18:979–992.

20. Freynhagen R, Baron R, TÖlle T, Stemmler E, Gockel U, Stevens M, et al. Screening of neuropathic pain components in patients with chronic back pain associated with nerve root compression: a prospective observational pilot study (MIPORT). Curr Med Res Opin. 2006; 22:529–537.

21. Treede RD, Jensen TS, Campbell JN, Cruccu G, Dostrovsky JO, Griffin JW, et al. Neuropathic pain: redefinition and a grading system for clinical and research purposes. Neurology. 2008; 70:1630–1635.

22. Miekisiak G, Kollataj M, Dobrogowski J, Kloc W, Libionka W, Banach M, et al. Validation and cross-cultural adaptation of the Polish version of the Oswestry Disability Index. Spine (Phila Pa 1976). 2013; 38:E237–E243.

23. Baron R, Freynhagen R, TÖlle TR, Cloutier C, Leon T, Murphy TK, et al. The efficacy and safety of pregabalin in the treatment of neuropathic pain associated with chronic lumbosacral radiculopathy. Pain. 2010; 150:420–427.

24. Kasimcan O, Kaptan H. Efficacy of gabapentin for radiculopathy caused by lumbar spinal stenosis and lumbar disk hernia. Neurol Med Chir (Tokyo). 2010; 50:1070–1073.

25. Kaye AD, Beuno FR, Katalenich B, Stell C, Liu H, Rosinia FA, et al. The effects of gastroretentive gabapentin (Gralise®) on spinal stenosis patients with radicular pain. Pain Physician. 2014; 17:169–178.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download