Abstract
Purpose
Materials and Methods
Results
Conclusion
Figures and Tables
Fig. 1
Study flow diagram. The actual revascularization was performed in 600 (68%) of the 877 patients indicated for revascularization and in 285 (29%) of the 969 patients not indicated for revascularization. CCTA, coronary computed tomographic angiography.

Fig. 2
Representative false positive cases for needing revascularization based on the coronary computed tomographic angiography (CCTA). (A) CCTA falsely identified this patient as a candidate for revascularization, based on the diffuse calcification of left anterior descending artery (LAD). (B) A second false-positive was indicated for revascularization because of a heavily calcified lesion within the LAD. (C) LAD was falsely identified as requiring revascularization because of lesion severity overestimation (arrow). (D) This right coronary artery was falsely indicated for revascularization because of a motion artifact (arrow). Right images of each panel (A, B, and C) are CCTA and left images are conventional coronary angiography. In panel (D), right and left upper images are CCTA and left lower image is conventional coronary angiography.

Fig. 3
Example of discordance between the coronary computed tomographic angiography (CCTA)-indicated therapy and the actual conducted therapy. Panel (A) and (B) are the CCTA and conventional coronary angiography images, respectively, from the same patient. (A) This patient was originally referred for need of revascularization of the left anterior descending artery based on the CCTA images (white arrow); however, revascularization was not performed (black arrow). Right image is CCTA and left image is conventional coronary angiography. (B) The same patient actually underwent revascularization of the left circumflex artery, which was not originally indicated based on CCTA images (white arrow); however, revascularization was performed (black arrow with solid line, before revascularization; black arrow with dotted line, after revascularization). Right image is CCTA, and middle and left images are conventional coronary angiography (before and after percutaneous coronary intervention, respectively).

Table 1
Baseline Clinical Characteristics

Table 2
The Ability of CCTA to Predict the Therapeutic Decision Making

CCTA, coronary computed tomographic angiography.
Data are presented as number (row percentage).
*The segments with more than 70% luminal narrowing of the coronary artery diameter were considered as a significantly stenosis with need of revascularization, †The segments with more than 50% luminal narrowing were considered as a significantly stenosis with need of revascularization.
Table 3
The Ability of CCTA to Predict the Therapeutic Decision Making

Table 4
The Accuracy of CCTA to Predict the Therapeutic Decision Making
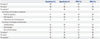
CCTA, coronary computed tomographic angiography; PPV, positive predictive value; NPV, negative predictive value.
*The segments with more than 70% luminal narrowing of the coronary artery diameter were considered as a significantly stenosis with need of revascularization, †The segments with more than 50% luminal narrowing were considered as a significantly stenosis with need of revascularization.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download