Abstract
Korea is not known as an endemic area for Histoplasma. However, we experienced a case of histoplasmosis in a person who had never been abroad. A 65-year-old female was admitted to the hospital for evaluation of multiple lung nodules. A computed tomography (CT) scan of the chest showed multiple ill-defined consolidations and cavitations in all lobes of both lungs. The patient underwent a CT-guided lung biopsy, and a histopathology study showed findings compatible with histoplasmosis. Based on biopsy results and clinical findings, the patient was diagnosed with chronic cavitary pulmonary histoplasmosis. The patient recovered completely following itraconazole treatment. This is the first case report of pulmonary histoplasmosis unconnected with either HIV infection or endemicity in Korea.
Histoplasmosis is an endemic disease that mainly occurs in the Ohio and Mississippi River Valleys of the United States and certain areas of North, Central, and South America.1 When people visit an endemic area or are engaged in outdoor activities such as caving, they could aspirate spores and run the risk of infection.2 Korea is not known as an endemic area for Histoplasma. However, we experienced a case of a 65-year-old woman who had never been abroad and presented with multiple pulmonary cavitary lesions, which were finally identified as chronic cavitary histoplasmosis. She was non-human immunodeficiency virus (HIV) patient, but she had a medication history of corticosteroid. We report herein this case.
A 65-year-old woman was admitted to the hospital for evaluation of multiple lung nodules. The patient had been living in an urban area of Korea. She denied any previous overseas travel history. The patient was seronegative for hepatitis B surface antigen, and for antibodies to hepatitis C, and HIV. She was diagnosed with autoimmune hemolytic anemia 2 years before the admission, and had been receiving corticosteroid monotherapy of 20 mg/day prednisolone. The patient was admitted because a chest X-ray showed new nodular opacities in both lungs, compared with a chest X-ray taken 6 months ago (Fig. 1). She did not report cough, dyspnea, hemoptysis, or pleuritic chest pain. She denied fever, night sweats, anorexia, or weight loss. Body temperature was 36.8℃, respiratory rate was 18/min, and blood pressure was 120/80 mm Hg. The chest was clear to auscultation. The laboratory results were as follows: hemoglobin, 11.7 g/dL; white blood cell count, 6230/uL (88.4% neutrophils, 5.9% lymphocytes); platelet count, 152000/µL; erythrocyte sedimentation rate, 12 mm/hr; C-reactive protein, 11.94 mg/dL; blood urea nitrogen, 23 mg/dL; creatinine, 0.87 mg/dL; aspartate aminotransferase, 15 IU/L; alanine aminotransferase, 19 IU/L; total bilirubin, 0.61 mg/dL; and reticulocyte count, 4.39%. Blood and sputum cultures were negative for any pyogenic bacteria. Sputum was negative for acid-fast bacilli by smear. A computed tomography (CT) scan of the chest showed multiple ill-defined consolidations and cavitations in all lobes of both lungs with the absence of mediastinal lymphadenopathy (Fig. 2). The patient underwent a CT-guided lung biopsy. A histopathology study revealed many oval shaped, budding yeast-form fungal micro-organisms in the cytoplasm of CD68(+) alveolar macrophages (Fig. 3), which was clearly identified by Periodic acid-Schiff and Gomori Methenamine Silver stains. The patient was diagnosed with chronic cavitary pulmonary histoplasmosis. Therapy was initiated with 200 mg itraconazole orally three times per day for 3 days and maintained with 200 mg orally twice per day for 12 months. She was well following treatment, and the follow-up chest X-ray taken 1 year later revealed complete resolution (Fig. 1).
Histoplasmosis is very rare in Korea, and only three cases have been reported. The first case was diagnosed on a peripheral blood smear from a newborn.3 The second case was a foreign worker diagnosed with Histoplasma peritonitis based on a laparoscopic biopsy.4 Third, a case of disseminated histoplasmosis in a patient with HIV infection, was reported.5 In the first case, the evaluation did not include complete immunological work-ups, nor was there a medical history to reveal possible exposure to histoplasmosis. In the second case, the patient was a 25-year-old man from Bangladesh. He was negative for HIV-antibody and was not immunocompromised. In the third case, a patient with HIV infection had been living in Guatemala for 5 years. Our patient had neither a history of recent travel abroad nor residence, and the serum HIV-antibody test was negative. The first case in newborn is also not connected with either HIV infection or travel history, but when it comes to a case of histologically confirmed cavitary histoplasmosis in adult, our patient might be the first report of histoplasmosis unconnected with either HIV infection or endemicity in Korea.
The most frequent sources for histoplasmosis in non-endemic areas are thought to be prior exposure to endemic areas through living or travelling abroad. Histoplasma may be found in isolated microfoci even in non-endemic areas, and patients can acquire histoplasmosis during activities that disturb these microfoci, as in endemic areas.2 The distribution of H. capsulatum in the environment varies; the highest concentrations of organisms exist in soil and nitrogen-bearing environments, including old chicken coops, decaying trees, river or creek banks, and caves contaminated with bat guano.6 Infection occurs by aerosol aspiration of spores, and a histoplasmosis outbreak can be accompanied with caving or exposure to an area where buildings are being demolished.7 Bat infested caves can be a source of human exposure to fungal spores, causing outbreaks of "cave disease" if inhalation exposure is heavy.8 The soil from a bird roost may contain fungal spores. Accordingly, disturbing the soil by cleaning may infect people who participate or live nearby. Although Korea is not an endemic area, there may be an environmental source of Histoplasma in Korea.
Fungal infections are becoming a serious problem to the elderly or immunocompromised patients. In this case, the patient was receiving corticosteroid for 2 years and it was assumed to be a predisposing factor in this case of histoplasmosis. Steroids have a depressant effect on host defense, particularly on cellular immunity, which appears to be the most important defense against fungal disease.9 Many cases of opportunistic histoplasmosis have been reported in the patients with long-term steroid use and many cases within those undergoing tumor necrosis factor blocker therapy for rheumatologic disorders or Crohn's disease.10,11,12
Most cases of opportunistic histoplasmosis occur in patients who are inhabitants of an endemic area or have been to infected places; thus, it is easier to infer infectious routes from their history.13,14,15 However, our case did not have any history of exposure to an endemic area.
Until recently, few studies have been conducted on domestic systemic mycoses in Korea, including histoplasmosis. Clinicians, therefore, have little experience with histoplasmosis, and no systemic guidelines are available for prompt diagnosis and treatment. The chance to develop imported mycosis is increasing according to the increase in the number of travelers and immigrant workers. Imported mycoses can become naturalized in Korea due to climate change and global warming. This case indicates that more investigations are needed to prepare guidelines for an early and accurate diagnosis.
Figures and Tables
Fig. 1
Chest X-ray images. (A) A chest X-ray taken 6 months before a diagnosis. (B) A chest X-ray taken before the start of treatment shows multiple nodules in both lungs. (C) A chest X-ray taken 12-month after treatment shows complete resolution of the nodules.

Fig. 2
Chest contrast-enhanced computed tomography (CT) scan images. (A) The chest CT scan shows well-defined multiple nodules of various sizes in both lung fields. (B) Some nodules have low internal attenuation or cavitation.

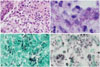
Fig. 3
Histopathologic examination of the lung. (A) Hematoxylin and eosin stain (×400). (B) Periodic acid-Schiff stain (×1000). (C) Gomori Methenamine Silver (GMS) stain (×1000). (D) Many budding yeast-form fungal microorganisms are observed in the cytoplasm of alveolar macrophages, which are clearly identified by the GMS stain (×1000).
References
1. Wheat LJ, Freifeld AG, Kleiman MB, Baddley JW, McKinsey DS, Loyd JE, et al. Clinical practice guidelines for the management of patients with histoplasmosis: 2007 update by the Infectious Diseases Society of America. Clin Infect Dis. 2007; 45:807–825.

2. Wheat LJ. Histoplasmosis: a review for clinicians from non-endemic areas. Mycoses. 2006; 49:274–282.

3. Jeon DS, Kim JR, Chun HJ, Hong YA, Kim WT. A case of histoplasmosis diagnosed on peripheral blood smear. Korean J Hematol. 1991; 26:391–396.
4. Kim HS, Kim KA, Kwon KS, Cho HG, Kim PS, Lee DH, et al. A case of histoplasma peritonitis. Inha Med J. 1999; 6:135–141.
5. Jeong HW, Sohn JW, Kim MJ, Choi JW, Kim CH, Choi SH, et al. Disseminated histoplasmosis and tuberculosis in a patient with HIV infection. Yonsei Med J. 2007; 48:531–534.

6. McKinsey DS, McKinsey JP. Pulmonary histoplasmosis. Semin Respir Crit Care Med. 2011; 32:735–744.

7. Goodwin RA, Loyd JE, Des Prez RM. Histoplasmosis in normal hosts. Medicine (Baltimore). 1981; 60:231–266.

8. Sénéchal A, Ferry T, Boibieux A, Brion JP, Epaulard O, Chidiac C, et al. Imported pulmonary histoplasmosis in three French cavers after a trip to Cuba. J Travel Med. 2012; 19:64–65.

9. Dismukes WE, Royal SA, Tynes BS. Disseminated histoplasmosis in corticosteroid-treated patients. Report of five cases. JAMA. 1978; 240:1495–1498.

10. Lan N, Patil DT, Shen B. Histoplasma capsulatum infection in refractory Crohn's disease of the pouch on anti-TNF biological therapy. Am J Gastroenterol. 2013; 108:281–283.

11. Bourré-Tessier J, Fortin C, Belisle A, Desmarais E, Choquette D, Senécal JL. Disseminated Histoplasma capsulatum infection presenting with panniculitis and focal myositis in rheumatoid arthritis treated with etanercept. Scand J Rheumatol. 2009; 38:311–316.
12. Hage CA, Bowyer S, Tarvin SE, Helper D, Kleiman MB, Wheat LJ. Recognition, diagnosis, and treatment of histoplasmosis complicating tumor necrosis factor blocker therapy. Clin Infect Dis. 2010; 50:85–92.

13. Tseng TC, Liaw SJ, Hsiao CH, Wang CY, Lee LN, Huang TS, et al. Molecular evidence of recurrent histoplasmosis with 9-year latency in a patient with Addison's disease. J Clin Microbiol. 2005; 43:4911–4913.

14. Murray PJ, Sladden RA. Disseminated histoplasmosis following long-term steroid therapy for reticulosarcoma. Br Med J. 1965; 2:631–632.

15. Kosseifi SG, Nassour DN, Shaikh MA, Sarubbi FA, Jordan RM, Peiris AN. Nodular pulmonary histoplasmosis in Cushing's disease: a case report and literature review. Tenn Med. 2007; 100:44–46.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download