Abstract
Purpose
This study examined the sparing effect of sufentanil on the median effective concentration (EC50) of epidural ropivacaine in elderly patients undergoing elective transurethral resection of prostate (TURP).
Materials and Methods
This was a prospective randomized double-blind dose-response study. Fifty eight elderly patients with American Society of Anesthesiologists physical status I-II who were scheduled for TURP surgery under epidural anesthesia were randomly allocated to a group receiving 15 mL of ropivacaine (group R) or a group receiving ropivacaine plus 5 µg of sufentanil (group RS). The concentration of ropivacaine was determined by a Dixon's up-and-down sequential allocation. The first participant received 0.3% of ropivacaine in both groups and subsequent concentrations were determined by the response of the previous patient in the same group. The EC50 of epidural ropivacaine was analyzed using the Dixon and Massey method.
Lumbar epidural anesthesia is the most widely used anesthetic regimen in elderly patients during transurethral urological surgery. However, the use of epidural nerve blockade could result in shorter onset and longer duration of anesthesia as well as more intense motor blockade in elder patients.1,2 Ropivacaine is a long-acting amide local anesthetic agent that exerts effects via reversible inhibition of sodium ion influx in nerve fibres with reduced lipophilicity, which is also associated with decreased potential for central nervous system toxicity and cardiotoxicity.3 Furthermore, recent clinical data have shown that ropivacaine is a proper alternate local anesthetic for spinal anesthesia in elderly patients with coexisting systemic disease for transurethral resection of prostate (TURP) operations.4 However, our previous study demonstrated that the EC50 of ropivacaine required to establish motor block decreases significantly with advancing age.5 Also, ropivacaine can still cause obvious cardiotoxicity when used in high concentrations. Therefore, co-administration of other pain relievers with local anesthetics has been tested in the clinic to reduce the concentration of ropivacaine used.
Previous studies have demonstrated that the addition of an opioid allows a lower concentration of local anesthetics to be used, which is beneficial during labour analgesia.6,7,8 Intrathecal addition of a lipophilic opioid to local anesthetics markedly improves the quality of anesthesia, prolongs the duration of analgesia, reduces the dose requirement of local anesthetics, and shortens the onset time of block.9,10,11,12,13 Sufentanil is a more lipophilic opioid with higher affinity for opioid receptors, has lower cephalad spread, and exhibits much higher analgesic potency compared to fentanyl or morphine.14,15,16 However, sufentanil together with local anesthetics is well accepted for the use in spinal anesthesia for cesarean delivery.11,13,17,18 Several previous studies have shown that addition of sufentail to ropivacaine, bupivacaine, or levobupivacaine for labor anesthesia or analgesia reduced minimum local analgesic concentrations (MLAC) of epidural local anesthetics and minimized motor block.6,7,8,19,20,21,22,23,24,25 However, no study has been carried out to determine the sparing effect of sufentanil on the EC50 of epidural ropivacaine for elderly patients.
This study investigated the local-anesthetic-sparing efficacy of sufentanil on the epidural anesthesia of ropivacaine for elderly patients during TURP.
Sixty-six American Society of Anesthesiologists physical status I-II patients scheduled for transurethral prostate and bladder procedures were enrolled in this study from May 2010 to Jun 2012. All patients were between 65 and 85 years of age with body mass index less than 25. The protocol (reference number 201006) was approved by the Ethics Committee of the First Affiliated Hospital, College of Medicine, Zhejiang University (Hangzhou, China). Signed informed consent was acquired from each participant. The exclusion criteria were: 1) patient is hypersensitive to amide local anesthetics or sufentanil, 2) patient exhibits contraindication to epidural anesthesia, and 3) patient received opioids or sedatives during the previous 12 hours.
Sample size was estimated based on an averaged SD of 0.025%. Power was given at 0.80 to detect a 10% difference of 1 SD (0.025%) at p<0.05. Therefore, a minimum of 12 subjects would be needed for each of the two groups. To estimate the EC50, the sample size was doubled and 33 subjects were recruited for each group.
Participants were randomly allocated to one of two groups by a random allocation table to receive 15 mL of ropivacaine (group R) (Naropin®; AstraZeneca, Sodertalje, Sweden) alone or ropivacaine with 5 µg of sufentanil (group RS) before insertion of the epidural catheter. The anesthesiologist performing the procedure and subsequent assessment was blinded to the concentration of anesthetics. All patients were not premedicated before anesthesia. After IV prehydration with 500 mL of lactated Ringer's solution, patients were placed in the flexed lateral position. The epidural space at the L2-3 or L3-4 level was identified with the loss of resistance to air injection. Every puncture was performed with a 16-gauge Tuohy epidural needle. A multiorifice epidural catheter was advanced 3 cm into the epidural space in the cephalad direction. The test dose was omitted due to the study design. After negative aspiration for cerebrospinal fluid or blood, 15 mL of ropivacaine (without epinephrine) was injected within 2 min through the catheter. The patient was then placed in the horizontal supine position.
The first patient in each group received 0.3% weight/volume (w/v) of ropivacaine based on our previous study.5 Thereafter, the concentration of ropivacaine for each subsequent patient was determined by the response of the previous patient in the same group using an up-down sequential allocation technique. The testing increment or decrement of ropivacaine was set to 0.025% (w/v) in both groups. The study solution was freshly prepared using 0.9% saline. In the group RS, 1 mL of sufentanil (5 µg/mL) was used instead of equivalent saline volume to achieve the desired ropivacaine concentration in the same final 15 mL volume. Effective or ineffective responses were determined for each concentration, respectively.
Sensory changes were recorded bilaterally along the anterior axillary line by pinprick using a short beveled 25-gauge needle. Sensory level was assessed by the Hollmen scale:26 0=ability to appreciate a pin prick as sharp; 1=ability to appreciate a pin prick as less sharp; 2=inability to appreciate a pin prick as sharp (analgesia); 3=inability to appreciate a pin touching (anesthesia). Onset time was defined as the period from full injection of the dose to the patient showing a Hollmen scale grade 2 at T10, bilaterally. The level of sensory anesthesia was assessed by an independent observer, who was blinded to the allocations.
Motor block in the lower limbs was assessed bilaterally by the same anesthetist 30 minutes after epidural injection with a Bromage scale27 (4=no motor block: complete flexion of knee and foot; 3=partial motor block: reduced flexion of knee, complete flexion of foot; 2=almost complete motor block: no flexion of knee, flexion of foot; and 1=complete motor block: no flexion of knee, no flexion of foot).
Effective: there was no pain and discomfort of the penis when pulling 30 minutes after epidural injection without the need for an epidural rescue bolus. This result elicited a decrement of 0.025% (w/v) ropivacaine for the next patient in the same group.
Ineffective: there was pain or discomfort of the penis when pulling 30 minutes after epidural injection, but the patient responded to a rescue bolus of 10 mL of 2% lidocaine. An increment of 0.025% (w/v) ropivacaine was used for the next patient in the same group.
Rejected: there was pain or discomfort of the penis when pulling 30 minutes after epidural injection, and the patient failed to respond to a rescue bolus. This outcome caused this patient to be excluded from subsequent analysis, and the same concentration of anesthetics was used for the next patient in the same group.
The parameters of pulse-oximetry, electrocardiogram, and non-invasive blood pressure measurements were recorded before epidural injection and at 5-min intervals during the study, and then every 5 min throughout surgery. Hypotension was defined as a decrease in systolic blood pressure by more than 30% of the pre-anesthetic value or a systolic blood pressure <90 mm Hg. Hypotension was treated by intravenous injection of 6 mg of ephedrine and crystalloid fluid. Bradycardia (<55 bpm) was treated by intravenous injection of 0.5 mg of atropine.
Statistical analysis was performed using SPSS 11.5 software (SPSS Inc., Chicago, IL, USA). Student's t-test was used for the normally distributed data, and the Mann-Whitney U test was used for non-normally distributed data. A p<0.05 (two sided) was considered statistically significant. The EC50 and its 95% confidence interval of the up-down sequences were analyzed using the formula of Dixon and Massey.28,29,30
A total of 66 subjects were recruited and 8 patients (4 in each group) were excluded from this study because of vascular puncture during block performance, unilateral block, and no anesthetic effect. Fifty-eight patients were included in the data analysis. No significant differences in pre-test variables such as demographic and surgical data were observed between the two groups (Table 1). No incidence of pruritus, nausea or vomiting was observed in the two groups. No significant differences in sensory block, the onset time to T10, and time to highest level of block were observed between two groups.
Figs. 1 and 2 show the sequences of effective and ineffective anesthesia for patients in group R and RS. The EC50 of ropivacaine without sufentanil for anesthesia during TURP surgery in elderly patients was 0.186% (95% confidence interval, 0.173-0.200%), while the EC50 of ropivacaine with sufentanil was 0.136% (95% confidence interval, 0.127-0.144%). A significant difference in EC50 was observed between the two groups (p<0.01).
Hemodynamic data are shown in Fig. 3. No significant differences in hypotension, bradycardia, and respiratory depression were observed between the two groups. The motor block was determined by the modified Bromage score, and no patient in the two groups developed motor block.
Previous studies have demonstrated that addition of intrathecal sufentanil to ropivacaine reduced local ropivacaine concentrations or ED50 during labor or caesarean delivery.21,22,23 However, there has been no study on the effect of sufentanil on the EC50 of epidural ropivacaine in elderly patients undergoing TURP. This study demonstrated that the EC50 of epidural ropivacaine coadministered with 5 µg of sufentanil was 0.136% in elderly patients during TURP surgery, which was significantly lower than the EC50 of ropivacaine without sufentanil (0.186%). To our best knowledge, this is the first study to provide evidence that 5 µg of sufentanil can significantly reduce the amount of epidural ropivacaine required for elderly patients undergoing TURP.
TURP is most often performed on elderly patients who have hypertension, other cardiovascular problems, problems in breathing, and problems in kidney functions. The mortality rate was 0.2% in the patients who underwent TURP, and increased morbidity was found in elderly patients.28 Local anesthesia is highly preferable in elderly patients undergoing TURP due to the observation that general anesthesia causes more hemodynamic differences.29,30 However, epidural local anesthetics can still produce high sensory and sympathetic block in elderly patients.1,2 Although reducing the dose of local anesthetic can decrease the hemodynamic side effects during cesarean delivery,31 a stable anesthesia regimen would be more beneficial for these patients. The addition of opioids to local anesthetics has been demonstrated to be an alternative method to establish sufficient sensory and motor block, while reducing hemodynamic side effects in elderly patients and patients with cardiovascular disease.32 In this study, the addition of sufentanil to ropivacaine provided sufficient anesthesia, but decreased the EC50 of epidural ropivacaine in elderly patients during TURP surgery.
The addition of opioids to local anesthetics has become a well-accepted practice in the management of spinal anesthesia for caesarean delivery. Sufentanil is a lipophilic opioid. Epidural sufentanil injected can penetrate the lipid filled subarachnoid and epidural space and enhances the local anesthetic effect by blocking the pain impulses. Co-administration of sufentanil with epidural ropivacaine exhibits rapid onset, long duration of analgesia, and motor block in a short time.33 Previous studies have shown that the local anesthetic sparing ability of sufentanil can be established using epidural infusions of local anesthetic with varying doses of sufentanil ranging from 2.5 to 20 µg. However, the effect of sufentanil on the EC50 of epidural ropivacaine in elderly patients undergoing TURP has not been reported. In this study, 5 µg of sufentanil was selected based on previous studies in caesarean delivery.12,22 However, a significant limitation of the current study is that only one dose of sufentanil was investigated, and this may not be the most effective dose. Therefore, studies on the effect of different doses of epidural sufentanil on EC50 of epidural ropivacaine for the transurethral procedure are needed to provide more accurate choices for clinicians.
In this study, the EC50 for ropivacaine is significantly lower than that of another study group.29 It is always difficult to compare EC50 values from different centers because the patient characteristics, anesthetic practice, and surgical practice may vary. Also, differences in MLAC methodology and clinical endpoints may contribute to the observed variations. Our previous study revealed that the EC50 of ropivacaine for motor blockade in elderly patients who underwent transurethral procedure was 0.383%.5 The EC50 was higher in our previous study than in this study (0.186%). This difference may be due to the fact that the protocol in the present study focused on exploring the EC50 of anesthesia, which might have less anesthetic requirements.
In this study, the dose of ropivacaine was adjusted according to up-down sequential allocation. The main advantage of this study design is the accuracy in determining the EC50. However, the starting ropivacaine concentration was 0.3% based on our previous study.5 This ropivacaine concentration is significantly different from the actual observed value of EC50. It would be ideal to start at a concentration close to the actual value of EC50, such as 0.2% to improve the validity of the results. This is because ropivacaine begins to be effective at 0.125% in patients who were administered ropivacaine and sufentanil and 0.175% in patients who were administered ropivacaine only.
In conclusion, the addition of 5 µg of sufentanil significantly decreased the EC50 of epidural ropivacaine for transurethral surgery without motor block on the lower limbs. More studies are needed to further investigate the ideal dose of sufentanil that should be coadministered epidurally with ropivacaine in elderly patients.
Figures and Tables
Fig. 1
The median effective concentration (EC50) of epidural ropivacaine for transurethral resection of prostate surgery is 0.186% (95% confidence interval, 0.173-0.200%) determined by the formula of Dixon and Massy. The testing interval was 0.025% (w/v). The vertical bar shows the concentration of ropivacaine (% w/v), and the horizontal bar shows the consecutive number of patients. w/v, weight/volume.

Fig. 2
The median effective concentration (EC50) of epidural ropivacaine with 5 µg of sufentanil for transurethral resection of prostate surgery is 0.136% (95% confidence interval, 0.127-0.144%) determined by the formula of Dixon and Massy. The testing interval was 0.025% (w/v). The vertical bar shows the concentration of ropivacaine (% w/v), and the horizontal bar shows the consecutive number of patients. w/v, weight/volume.
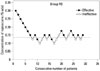
Fig. 3
Hemodynamic changes before (0 minutes) and after epidural injection. Values are mean (SD). There was no significant difference between group R and group RS. MAP, mean arterial blood pressure; HR, heart rate.

Table 1
Demographic Data of Patients and Characteristics of Epidural Anesthesia Administration

ACKNOWLEDGEMENTS
This study was supported by the Qianjiang talents project granted by the Department of Technology, Zhejiang province (No.: 2012R10033).
We thank Hanjian Chen, one anesthesiologist, for assistance during the experiments.
References
1. Nydahl PA, Philipson L, Axelsson K, Johansson JE. Epidural anesthesia with 0.5% bupivacaine: influence of age on sensory and motor blockade. Anesth Analg. 1991; 73:780–786.
2. Simon MJ, Veering BT, Stienstra R, van Kleef JW, Burm AG. The effects of age on neural blockade and hemodynamic changes after epidural anesthesia with ropivacaine. Anesth Analg. 2002; 94:1325–1330.

3. Kuthiala G, Chaudhary G. Ropivacaine: a review of its pharmacology and clinical use. Indian J Anaesth. 2011; 55:104–110.

4. Chaudhary A, Bogra J, Singh PK, Saxena S, Chandra G, Verma R. Efficacy of spinal ropivacaine versus ropivacaine with fentanyl in transurethral resection operations. Saudi J Anaesth. 2014; 8:88–91.

5. Li Y, Zhu S, Bao F, Xu J, Yan X, Jin X. The effects of age on the median effective concentration of ropivacaine for motor blockade after epidural anesthesia with ropivacaine. Anesth Analg. 2006; 102:1847–1850.

6. Lyons G, Columb M, Hawthorne L, Dresner M. Extradural pain relief in labour: bupivacaine sparing by extradural fentanyl is dose dependent. Br J Anaesth. 1997; 78:493–497.

7. Polley LS, Columb MO, Wagner DS, Naughton NN. Dose-dependent reduction of the minimum local analgesic concentration of bupivacaine by sufentanil for epidural analgesia in labor. Anesthesiology. 1998; 89:626–632.

8. Robinson AP, Lyons GR, Wilson RC, Gorton HJ, Columb MO. Levobupivacaine for epidural analgesia in labor: the sparing effect of epidural fentanyl. Anesth Analg. 2001; 92:410–414.

9. Lee YY, Ngan Kee WD, Muchhal K, Chan CK. Randomized double-blind comparison of ropivacaine-fentanyl and bupivacaine-fentanyl for spinal anaesthesia for urological surgery. Acta Anaesthesiol Scand. 2005; 49:1477–1482.

10. Unlugenc H, Ozalevli M, Gunduz M, Gunasti S, Urunsak IF, Guler T, et al. Comparison of intrathecal magnesium, fentanyl, or placebo combined with bupivacaine 0.5% for parturients undergoing elective cesarean delivery. Acta Anaesthesiol Scand. 2009; 53:346–353.

11. Braga Ade F, Braga FS, Potério GM, Pereira RI, Reis E, Cremonesi E. Sufentanil added to hyperbaric bupivacaine for subarachnoid block in Caesarean section. Eur J Anaesthesiol. 2003; 20:631–635.

12. Oğün CO, Kirgiz EN, Duman A, Okesli S, Akyürek C. Comparison of intrathecal isobaric bupivacaine-morphine and ropivacaine-morphine for Caesarean delivery. Br J Anaesth. 2003; 90:659–664.
13. Wang LZ, Zhang YF, Tang BL, Yao KZ. Effects of intrathecal and i.v. small-dose sufentanil on the median effective dose of intrathecal bupivacaine for Caesarean section. Br J Anaesth. 2007; 98:792–796.

14. Leysen JE, Gommeren W, Niemegeers CJ. [3H]Sufentanil, a superior ligand for mu-opiate receptors: binding properties and regional distribution in rat brain and spinal cord. Eur J Pharmacol. 1983; 87:209–225.

15. Grass JA, Sakima NT, Schmidt R, Michitsch R, Zuckerman RL, Harris AP. A randomized, double-blind, dose-response comparison of epidural fentanyl versus sufentanil analgesia after cesarean section. Anesth Analg. 1997; 85:365–371.

16. Olofsson C, Nygårds EB, Bjersten AB, Hessling A. Low-dose bupivacaine with sufentanil prevents hypotension after spinal anesthesia for hip repair in elderly patients. Acta Anaesthesiol Scand. 2004; 48:1240–1244.

17. Meininger D, Byhahn C, Kessler P, Nordmeyer J, Alparslan Y, Hall BA, et al. Intrathecal fentanyl, sufentanil, or placebo combined with hyperbaric mepivacaine 2% for parturients undergoing elective cesarean delivery. Anesth Analg. 2003; 96:852–858.
18. Dahlgren G, Hultstrand C, Jakobsson J, Norman M, Eriksson EW, Martin H. Intrathecal sufentanil, fentanyl, or placebo added to bupivacaine for cesarean section. Anesth Analg. 1997; 85:1288–1293.

19. Polley LS, Columb MO, Lyons G, Nair SA. The effect of epidural fentanyl on the minimum local analgesic concentration of epidural chloroprocaine in labor. Anesth Analg. 1996; 83:987–990.

20. Palm S, Gertzen W, Ledowski T, Gleim M, Wulf H. Minimum local analgesic dose of plain ropivacaine vs. ropivacaine combined with sufentanil during epidural analgesia for labour. Anaesthesia. 2001; 56:526–529.

21. Buyse I, Stockman W, Columb M, Vandermeersch E, Van de Velde M. Effect of sufentanil on minimum local analgesic concentrations of epidural bupivacaine, ropivacaine and levobupivacaine in nullipara in early labour. Int J Obstet Anesth. 2007; 16:22–28.

22. Chen X, Qian X, Fu F, Lu H, Bein B. Intrathecal sufentanil decreases the median effective dose (ED50) of intrathecal hyperbaric ropivacaine for caesarean delivery. Acta Anaesthesiol Scand. 2010; 54:284–290.

23. Parpaglioni R, Baldassini B, Barbati G, Celleno D. Adding sufentanil to levobupivacaine or ropivacaine intrathecal anaesthesia affects the minimum local anaesthetic dose required. Acta Anaesthesiol Scand. 2009; 53:1214–1220.

24. Boulier V, Gomis P, Lautner C, Visseaux H, Palot M, Malinovsky JM. Minimum local analgesic concentrations of ropivacaine and levobupivacaine with sufentanil for epidural analgesia in labour. Int J Obstet Anesth. 2009; 18:226–230.

25. Wulf HF. Up-down sequential allocation technique to investigate the influence of opioids on the efficacy of epidural local anesthetics in labor pain. Anesthesiology. 1999; 90:1788–1789.

26. Capogna G, Celleno D, Laudano D, Giunta F. Alkalinization of local anesthetics. Which block, which local anesthetic? Reg Anesth. 1995; 20:369–377.
27. Bromage PR. A comparison of the hydrochloride and carbon dioxide salts of lidocaine and prilocaine in epidural analgesia. Acta Anaesthesiol Scand Suppl. 1965; 16:55–69.

28. Mebust WK, Holtgrewe HL, Cockett AT, Peters PC. Writing Committee, the American Urological Association. Transurethral prostatectomy: immediate and postoperative complications. Cooperative study of 13 participating institutions evaluating 3,885 patients. J Urol, 141: 243-247, 1989. J Urol. 2002; 167:5–9.

29. Ozmen S, Koşar A, Soyupek S, Armağan A, Hoşcan MB, Aydin C. The selection of the regional anaesthesia in the transurethral resection of the prostate (TURP) operation. Int Urol Nephrol. 2003; 35:507–512.

30. Dobson PM, Caldicott LD, Gerrish SP, Cole JR, Channer KS. Changes in haemodynamic variables during transurethral resection of the prostate: comparison of general and spinal anaesthesia. Br J Anaesth. 1994; 72:267–271.

31. Meyer RA, Macarthur AJ, Downey K. Study of equivalence: spinal bupivacaine 15 mg versus bupivacaine 12 mg with fentanyl 15 µg for cesarean delivery. Int J Obstet Anesth. 2012; 21:17–23.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download