Abstract
Purpose
Studies have shown that diabetes mellitus (DM) is a risk factor for cardiovascular disease, including atrial fibrillation (AF); however, the clinical characteristics and prognostic impact of DM in patients with nonvalvular AF have not been well understood in China.
Materials and Methods
Included were 1644 consecutive patients with nonvalvular AF. Endpoints included all-cause mortality, cardiovascular mortality, stroke, major bleeding, and combined endpoint events (CEE) during a 1-year follow-up.
Results
The prevalence of DM was 16.8% in nonvalvular AF patients. Compared with non-diabetic AF patients, diabetic AF patients were older and tended to coexist with other cardiovascular diseases. Most patients with DM (93.5%) were eligible for anticoagulation, as determined by CHADS2 scores. However, only 11.2% of patients received anticoagulation. During a 1-year follow-up, the all-cause mortality and CEE rate in the DM group were significantly higher than those of the non-DM group, while the incidence of stroke was comparable. After multivariate adjustments, DM was still an independent risk factor for 1-year all-cause mortality [hazard ratio (HR)=1.558; 95% confidence interval (CI) 1.126-2.156; p=0.007], cardiovascular mortality (HR=1.615; 95% CI 1.052-2.479; p=0.028), and CEE (HR=1.523; 95% CI 1.098-2.112; p=0.012), yet not for stroke (HR=1.119; 95% CI 0.724-1.728; p=0.614).
Atrial fibrillation (AF) is the most common cardiac arrhythmia, occurring in 1-2% of the general population.1 The incidence of AF is known to increase with age, and an estimated 8 million people are affected in China.2 Additionally, this number is increasing rapidly due to the accelerated aging of the population. AF is associated with substantial complications, including increased risk of stroke, heart failure, and mortality,3 resulting in a serious health threat and a costly health burden.
Diabetes mellitus (DM) is an established risk factor for cardiovascular diseases such as hypertension, coronary heart disease, and heart failure.4,5 Moreover, DM has been regarded as a risk factor associated with stroke in current stroke risk scores.6,7 In recent years, studies have reported an increased risk of developing AF in patients with DM.8,9,10,11,12 Therefore, AF and DM often coexist and make treatment complicated. Individuals with AF and DM are at increased risk of thromboembolic complications, most notably stroke. It was reported that the incidence of stroke in patients with DM and AF ranges between 3.6% and 8.6% per year.13,14 Furthermore, the presence of DM may enhance the progression from paroxysmal AF to persistent AF15 and mask the cardiac symptoms of AF possibly due to DM neuropathy,16 resulting in delayed diagnosis and treatment.
Previous studies have investigated the impact of DM on the outcomes of patients with acute coronary syndrome,17 heart failure,18 and those undergoing coronary artery bypass surgery.19 However, the clinical characteristics, treatment, and prognostic impact of DM in patients with nonvalvular AF have not been well understood in China. The aim of the present study was therefore to investigate the issue from a prospectively designed multicenter registry study in China.
From November 2008 to October 2011, a total of 2016 consecutive patients presenting to the emergency department (ED) with AF in 20 hospitals around China were recruited. The 20 hospitals were selected to represent different levels of medical care (academic and non-academic, general and specialized, urban and rural). This was a multicenter, prospective registry study with the aim of evaluating the risk factors and treatment of AF, as well as the 1-year outcomes including mortality, stroke, non-central nervous system (non-CNS) embolism, and major bleeding. Study protocols were approved by the appropriate Institutional Review Boards of Fuwai hospital and complied with the declaration of Helsinki. All subjects were provided with written informed consent.
Patients were included in the registry if they had documented (electrocardiographic evidence by electrocardiogram, Holter, and rhythm strip) AF at the time of ED visits, regardless of the reason. Baseline characteristics including sex, age, weight, admission blood pressure, heart rate, and medical histories were collected at admission, and if necessary, related data was also collected from the patients' hospital charts and electronic medical records. The diagnoses of all medical conditions were based on clinical records. The type of AF included paroxysmal, persistent, or permanent AF. Paroxysmal AF was defined as AF episodes that terminate spontaneously. Persistent AF was defined as AF episodes that do not terminate spontaneously, yet do convert with either electrical or pharmacological cardioversion. Cases of AF that did not terminate either spontaneously or with electrical or chemical cardioversion or in which cardioversion had not been attempted were all classified as permanent AF.
Follow-up was carried out 1 year±4 weeks after enrolment by telephone, outpatient service, or delivery of medical records. The primary endpoint was all-cause mortality during the 12-month follow-up. Secondary endpoints were cardiovascular mortality, stroke, major bleeding, and combined endpoint events (CEE, including all-cause mortality, stroke, non-CNS embolism, and major bleeding). Outcomes were adjudicated by a committee blinded to the therapy patients according to standardized definitions.
The definitions of every event were as follows. Death and the cause were determined as reported by the relatives of the participants during follow-up by telephone, and if possible, medical records were obtained. Stroke was defined as focal neurological deficits lasting at least 24 h and confirmed by computed tomographic scans or magnetic resonance imaging. The imaging data were collected during follow-up. Non-CNS embolism was defined as an acute loss of blood flow to a peripheral artery, supported by evidence of embolism from ultrasound tests, surgical specimens, angiography, or other objective testing. Major bleeding was defined as bleeding in a critical location such as intracranial bleeding, bleeding leading to surgical intervention, overt bleeding associated with a drop in hemoglobin concentration of ≥20 g/L or leading to transfusion of 2 or more units of blood, or fatal bleeding. These data were also collected during follow-up.
The patients were divided into a DM group and a non-DM group according to coexistent DM. DM was defined as a previous history of diabetes (treated with insulin or an oral hypoglycemic agent), or a non-fasting blood glucose level ≥11.1 mmol/L (200 mg/dL). The group of DM patients was compared with non-DM patients in terms of demographics, clinical characteristics, and 1-year outcomes.
The baseline characteristics of the patients are presented as mean±standard deviation for continuous variables and compared by Student's t-test if the data were normally distributed; otherwise the Wilcoxon signed rank test was used. Categorical variables are presented as percentage and were compared by Pearson's chi-square test. Survival curves and cumulative hazard function were constructed using the Kaplan-Meier method. Log-rank tests were used to compare the curves of the two groups. Univariate and multivariate Cox proportional hazard regression models were performed to identify whether there was an association between DM and the 1-year outcomes, and the models were corrected for age, sex, weight, medical history, vital signs at admission, and main medications. The adjusted hazard ratios (HRs), along with their respective 95% confidence intervals (CIs), were calculated for the two groups. All statistical tests were 2-tailed, and p values were statistically significant at <0.05. All statistical analyses were carried out using SPSS statistical software, version 19.0 (SPSS Inc., Chicago, IL, USA).
Of 2016 AF patients, 331 patients with valvular AF and 41 nonvalvular AF patients with incomplete data were excluded; consequently, 1644 patients were analyzed, of which 277 patients (16.8%) had concomitant DM.
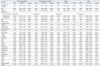
Table 1 summarizes the baseline characteristics in AF patients with and without DM. Compared with non-diabetic patients, patients with DM were more likely to be older (DM: 72.9±10.5 years; non-DM: 69.4±13.3 years; p<0.001) and heavier (DM: 66.6±11.4 kg; non-DM: 64.9±12.1 kg; p=0.029). As for cardiovascular histories, DM tended to coexist with coronary heart disease and hypertension, and the DM group also had a significantly higher percentage of stoke or transient ischemic attack, as well as myocardial infarction (MI) (all p<0.01). The admission systolic blood pressure in the DM group was higher than in the non-DM group (DM: 138.4±23.6 mm Hg; non-DM: 132.8±22.7 mm Hg; p<0.001), while diastolic blood pressure and heart rate was similar between the two groups (all p>0.05).
Table 2 shows the treatment during the 1-year follow-up. Those who were evaluated by CHADS2 scores and ≥2 (congestive heart failure=1, hypertension=1, age=1, diabetes=1, and stroke=2) were eligible for anticoagulation treatment. It was shown that a significantly higher percentage of patients with AF and DM needed anticoagulation treatment, compared with those without DM (DM: 93.5%; non-DM: 47.8%; p<0.001). However, anticoagulation with warfarin was adopted by only a small number of patients with DM (11.2%) and without DM (12.8%), and less than half of these patients reached the recommended international normalized ratio (INR) target. In contrast, more patients in the two groups (DM: 61.0%; non-DM: 55.7%) were prescribed with aspirin, and a small fraction of patients were prescribed clopidogrel instead of anticoagulation. In addition, patients in the DM group were more likely to be prescribed with beta-blocker, nondihydropyridine calcium channel blocker, angiotensin receptors blockers (ARB), and lipid-lowering agents (all p<0.05). Furthermore, for achieving and maintaining sinus rhythm, only a small portion of patients were treated with drug cardioversion (e.g., amiodarone), electrical cardioversion, or catheter ablation, and there was no significant difference between the two groups.
Fig. 1 shows the 1-year outcomes of the two groups. The overall 1-year all-cause mortality was 13.9% (228 of 1644 patients) in the present study. The all-cause mortality in the DM group was significantly higher than in the non-DM group (DM: 19.5%; non-DM: 12.7%; p=0.004). The overall incidence of stroke during the 1-year follow-up was 7.8% (129 of 1644 patients). However, the incidences of stroke between the two groups were comparable (DM: 10.1%; non-DM: 7.4%; p=0.141). The incidences of major bleeding were also comparable (DM: 0.3%; non-DM: 1.5%; p=0.166). The CEE rate in the DM group during the 1-year follow-up was significantly higher than that of the non-DM group (DM: 26.4%; non-DM: 20.4%; p=0.023).
The causes of death for the two groups are displayed in Table 3. It was observed that heart failure and infection were the major causes of death in both groups. The proportional mortality rate was similar between the two groups, except that the percentage of those who died of MI was higher in the DM group than in the non-DM group (DM: 9.3%; non-DM: 2.3%; p=0.036).
Fig. 2 shows the 1-year event curves of the two groups. It was observed that there were significant differences between the two groups in the survival curves of all-cause mortality (p=0.002), cardiovascular mortality (p=0.019), and cumulative CEE rates (p=0.004). However, the cumulative incidences of stroke between the two groups during the 1-year follow-up were comparable (p=0.127).
Table 4 displays the predictors of 1-year outcomes by univariate Cox analysis. It was found that DM was associated with increased risk of all-cause mortality (HR=1.596; 95% CI 1.176-2.116; p=0.003), cardiovascular mortality (HR=1.614; 95% CI 1.078-2.416; p=0.020), and CEE (HR=1.570; 95% CI 1.154-2.135; p=0.004), whereas it was not associated with an increased risk of stroke (HR=1.383; 95% CI 0.910-2.102; p=0.129).
Table 5 shows the results of a multivariate Cox analysis of 1-year outcomes. After adjusting the variables related with the outcomes of patients with AF, DM was still an independent risk factor for 1-year all-cause mortality (HR=1.558; 95% CI 1.126-2.156; p=0.007), cardiovascular mortality (HR=1.615; 95% CI 1.052-2.479; p=0.028), and CEE (HR=1.523; 95% CI 1.098-2.112; p=0.012); however, it was not an independent risk factor for stroke (HR=1.119; 95% CI 0.724-1.728; p=0.614).
The major findings from the present study are as follows. First, DM was prevalent among patients with nonvalvular AF, and more than 15% of nonvalvular AF patients suffered from concomitant DM. Clinically, most patients with nonvalvular AF and DM were at high risk for stroke; however, only a small amount of patients received anticoagulation treatment in China. Second, AF patients with DM had higher 1-year all-cause mortality, cardiovascular mortality, and CEE rates, yet had a similar incidence of stroke compared with those without DM. Third, after multivariate adjustment, DM was still an independent risk factor for 1-year all-cause death, cardiovascular death, and CEE, although it was not a risk factor for stroke.
The role of DM in cardiovascular risk and disease has been widely investigated. The adverse influence of DM on the cardiovascular system not only increases the risk of developing cardiovascular diseases but also exacerbates the outcome. Indeed, cardiovascular diseases are the most prevalent cause of morbidity and mortality in patients with DM.20 AF is the most common sustained cardiac arrhythmia in the population, and several epidemiologic studies have reported that DM is an independent risk factor for AF.2,4,5,9,10 Although the causal relationship between DM and AF remains to be elucidated,21 one likely explanation is that DM, directly or indirectly, affects cardiac electrophysiology supposedly by means of autonomic, electrical, and structural remodeling.22 Given the intimate relationship between AF and DM, further studies on the clinical characteristics of patients with AF and DM, as well as the impact of DM on clinical outcome in patients with AF, are of great importance for risk stratification and clinical management.
In our study, the prevalence of DM in patients with AF was 16.8%, similar to previous reports from western countries,23,24,25 though higher than data reported several years ago from China.26 With the development of social economy and an aging population, lifestyle changes related obesity, eating behavior, and physical activity may contribute to the increased prevalence of DM in general population, consistent with the findings in our study that patients with DM were more likely to be older and heavier. Meanwhile, patients with AF and DM had a higher prevalence of traditional cardiovascular risk factors such as hypertension, coronary heart disease, and stroke, which also demonstrated the association between DM and cardiovascular disease.
Anticoagulation is an important component in the management of AF, in that this arrhythmia is associated with an increased risk for stroke. In the present study, up to 93.5% of patients with AF and DM belonged to a high risk population stratified by CHADS2 risk scores.6 However, only 11.2% of these patients received warfarin for anticoagulation, and the number was even lower than those without DM (12.8%), in which the percentage of patients eligible for anticoagulation (47.8%) was lower than that of the patients with AF and DM (93.5%). Furthermore, less than half of the patients that received warfarin for anticoagulation reached the recommended INR target, indicating that the use and monitoring of warfarin remain to be improved. Although the overall proportion of patients that received anticoagulation with warfarin was low (12.5%) compared with that of the western countries,27 the number has been improved notably compared with several years ago in China (2.7%),2 reflecting progress in developing awareness for anticoagulation. However, more than half of the patients, regardless of whether they had DM or not, were prescribed aspirin or clopidogrel, which were confirmed to be ineffective in preventing thrombus.28 Moreover, about 20% of patients did not receive any prophylactic anticoagulation therapy, reflecting a huge gap between clinical guidelines and real-world practice in China. Fear of bleeding, the inconvenience of frequent INR monitoring, and excessive interaction between warfarin and other medications or foods may result in hesitating to select warfarin. It is expected that more AF patients will receive anticoagulation according to current guidelines by means of propaganda and education for both clinicians and patients. Moreover, it is anticipated that new oral anticoagulants characterized by safety, effectiveness, convenience, and also inexpensiveness will be widely available in China.
The prognostic impact of DM in patients with AF deserves critical attention. In our data, the overall 1-year mortality was 13.9%, similar to a previous report from the Framingham Heart Study.29 However, patients with AF and DM had higher all-cause mortality, cardiovascular mortality, and CEE rates during the 1-year follow-up in patients with DM than those without DM, demonstrating the serious macrovascular damage of DM. Indeed, cardiovascular disease is the major cause of morbidity and mortality for individuals with DM. Although the precise pathophysiological and clinical relationships between DM and cardiovascular disease are not completely understood, it has been suggested that an association between hyperglycemia and intracellular metabolic changes can result in oxidative stress, low-grade inflammation, and endothelial dysfunction, which may accelerate atherosclerosis and increase cardiovascular risk.20 Moreover, DM may mask the cardiac symptoms during an ischemic heart attack and also influence the cardiac symptoms related to AF,16 which may lead to delayed treatment and poor outcome in patients with DM.
In the present study, the 1-year incidence of stroke was 7.8% in whole patients and 10.1% in patients with DM, higher than previous reports.14 One possible explanation was the low level of anticoagulation treatment in patients with AF. Furthermore, as was found in our study, DM was not associated with an increased risk of stroke during the 1-year follow-up. Although certain previous studies30,31 also came to similar conclusions, pooled data from earlier stroke trials32 all identified DM as an independent risk factor for stroke. Indeed, the presence of DM predisposes patients to hypercoagulability characterized by platelet activation, increased production and activation of clotting factors, and hyperviscosity status.13 Currently, DM is included in commonly used, validated stroke risk scores that are incorporated in international guidelines.6,7 A possible interpretation for our results is that a relatively short follow-up period (median: 1 year) may not detect a significant difference in the incidences of stroke between DM and non-DM groups, whereas in other studies, such as the Framingham Heart Study,33 the mean follow-up period was 4 years, and most other studies had more than 2 years of follow-up.14 However, a trend toward increased incidence of stroke was observed in patients with DM at the end of the follow-up from the Kaplan-Meier curves, and a long period of follow-up is required to further detect the long-term impact of DM on risk of stroke.
In view of the high prevalence of DM in patients with AF, the high risk for embolism among patient characteristics, and the adverse prognostic influence, aggressive strategies are required for those with DM and AF. The risk of stroke varies among DM patients with AF, and treatment relies on risk stratification [CHADS2 or CHA2DS2-VASc (vascular disease, age 65-74, sex category) scores] and appropriate anticoagulation therapy. Currently, catheter ablation may be beneficial in the treatment of AF-associated DM.7 Additionally, upstream therapy such as ARBs34 and thiazolidinediones35 may also be beneficial for patients with DM and AF. Our study also suggests that use of ARBs was associated with a decreased risk of all-cause mortality and CEE. Moreover, use of lipid-lowering agents was associated with a decreased risk of stroke in our study. Therefore, more studies are required to further evaluate the impact of these agents on long-term outcomes.
There are some limitations in our study that should be noted. First, hemoglobin A1c percentages and fasting blood sugars were not recorded, limiting insight into glucose control, a factor that may have an effect on outcomes. Second, the duration of DM prior to study enrolment was also not known, which may reflect the severity of DM and associated co-morbid conditions; such a potential confounder may also affect the prognosis. Third, DM status in patients with AF was evaluated at enrollment only; we did not ascertain cases of DM that developed during the study follow-up. In addition, despite multivariate adjustments, residual confounding may remain. Finally, in our study, the period of follow-up was relatively short. Therefore, the long-term prognostic impact of DM in patients with nonvalvular AF needs to be evaluated by a long-term follow-up.
In conclusion, DM was found to be a common morbidity coexisting with nonvalvular AF and was associated with increased 1-year all-cause and cardiovascular mortality, as well as a higher CEE rate. A 1-year follow-up identified the association of DM with increased risk for all-cause mortality, cardiovascular mortality, and CEE; however, there was no increased risk for stroke.
Figures and Tables
Fig. 1
1-year outcomes of nonvalvular AF patients with and without DM. AF, atrial fibrillation; DM, diabetes mellitus; CEE, combined endpoint events (including all-cause mortality, stroke, non-CNS embolism, and major bleeding); CNS, central nervous system.
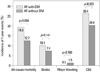
Fig. 2
The Kaplan-Meier event rates of nonvalvular AF patients with and without DM. (A) Survival curves of all-cause mortality. (B) Survival curves of cardiovascular mortality. (C) Cumulative incidence of stroke. (D) Cumulative incidence of CEE (including all-cause mortality, stroke, non-CNS embolism, and major bleeding). AF, atrial fibrillation; DM, diabetes mellitus; CEE, combined endpoint events; CNS, central nervous system.
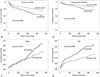
Table 1
Baseline Characteristics in Nonvalvular AF Patients with and without DM

Table 2
Treatment during 1-Year Follow-Up in Nonvalvular AF Patients with and without DM

Table 3
Causes of Death during 1-Year Follow-Up in Nonvalvular AF Patients with and without DM

Table 4
Predictors of 1-Year Events by Univariate Cox Analysis
CEE, combined endpoint events; AF, atrial fibrillation; DM, diabetes mellitus; MI, myocardial infarction; TIA, transient ischemic attack; COPD, chronic obstructive pulmonary disease; SBP, systolic blood pressure; DBP, diastolic blood pressure; CCB, calcium channel blocker; ACEI, angiotensin-converting enzyme inhibitors; ARB, angiotensin receptors blockers; HR, hazard ratio; CI, confidence interval.
Table 5
Predictors of 1-Year Events by Multivariate Cox Analysis

ACKNOWLEDGEMENTS
We thank the investigators from every hospital for providing data and all the study coordinators, as well as the patients who participated in the multicenter study.
References
1. Chinitz JS, Castellano JM, Kovacic JC, Fuster V. Atrial fibrillation, stroke, and quality of life. Ann N Y Acad Sci. 2012; 1254:140–150.

2. Hu D, Sun Y. Epidemiology, risk factors for stroke, and management of atrial fibrillation in China. J Am Coll Cardiol. 2008; 52:865–868.

3. Stewart S, Hart CL, Hole DJ, McMurray JJ. A population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley study. Am J Med. 2002; 113:359–364.

4. Benjamin EJ, Levy D, Vaziri SM, D'Agostino RB, Belanger AJ, Wolf PA. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA. 1994; 271:840–844.

5. Ostgren CJ, Merlo J, Råstam L, Lindblad U. Atrial fibrillation and its association with type 2 diabetes and hypertension in a Swedish community. Diabetes Obes Metab. 2004; 6:367–374.

6. Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA. 2001; 285:2864–2870.

7. European Heart Rhythm Association. European Association for Cardio-Thoracic Surgery. Camm AJ, Kirchhof P, Lip GY, Schotten U, et al. Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Europace. 2010; 12:1360–1420.
8. Huxley RR, Filion KB, Konety S, Alonso A. Meta-analysis of cohort and case-control studies of type 2 diabetes mellitus and risk of atrial fibrillation. Am J Cardiol. 2011; 108:56–62.

9. Movahed MR, Hashemzadeh M, Jamal MM. Diabetes mellitus is a strong, independent risk for atrial fibrillation and flutter in addition to other cardiovascular disease. Int J Cardiol. 2005; 105:315–318.

10. Nichols GA, Reinier K, Chugh SS. Independent contribution of diabetes to increased prevalence and incidence of atrial fibrillation. Diabetes Care. 2009; 32:1851–1856.

11. Huxley RR, Alonso A, Lopez FL, Filion KB, Agarwal SK, Loehr LR, et al. Type 2 diabetes, glucose homeostasis and incident atrial fibrillation: the Atherosclerosis Risk in Communities study. Heart. 2012; 98:133–138.

12. Johansen OE, Brustad E, Enger S, Tveit A. Prevalence of abnormal glucose metabolism in atrial fibrillation: a case control study in 75-year old subjects. Cardiovasc Diabetol. 2008; 7:28.

13. Asghar O, Alam U, Hayat SA, Aghamohammadzadeh R, Heagerty AM, Malik RA. Obesity, diabetes and atrial fibrillation; epidemiology, mechanisms and interventions. Curr Cardiol Rev. 2012; 8:253–264.

14. Stroke Risk in Atrial Fibrillation Working Group. Independent predictors of stroke in patients with atrial fibrillation: a systematic review. Neurology. 2007; 69:546–554.
15. Sakamoto H, Okamoto E, Imataka K, Ieki K, Fujii J. Prediction of early development of chronic nonrheumatic atrial fibrillation. Jpn Heart J. 1995; 36:191–199.

16. Sugishita K, Shiono E, Sugiyama T, Ashida T. Diabetes influences the cardiac symptoms related to atrial fibrillation. Circ J. 2003; 67:835–838.

17. Alnemer KA, Alfaleh HF, Alhabib KF, Ullah A, Hersi A, Alsaif S, et al. Impact of diabetes on hospital adverse cardiovascular outcomes in acute coronary syndrome patients: data from the Saudi project of acute coronary events. J Saudi Heart Assoc. 2012; 24:225–231.

18. Sarma S, Mentz RJ, Kwasny MJ, Fought AJ, Huffman M, Subacius H, et al. Association between diabetes mellitus and post-discharge outcomes in patients hospitalized with heart failure: findings from the EVEREST trial. Eur J Heart Fail. 2013; 15:194–202.

19. Zhang X, Wu Z, Peng X, Wu A, Yue Y, Martin J, et al. Prognosis of diabetic patients undergoing coronary artery bypass surgery compared with nondiabetics: a systematic review and meta-analysis. J Cardiothorac Vasc Anesth. 2011; 25:288–298.

20. Matheus AS, Tannus LR, Cobas RA, Palma CC, Negrato CA, Gomes MB. Impact of diabetes on cardiovascular disease: an update. Int J Hypertens. 2013; 2013:653789.

21. Sun Y, Hu D. The link between diabetes and atrial fibrillation: cause or correlation. J Cardiovasc Dis Res. 2010; 1:10–11.

22. Lin Y, Li H, Lan X, Chen X, Zhang A, Li Z. Mechanism of and therapeutic strategy for atrial fibrillation associated with diabetes mellitus. ScientificWorldJournal. 2013; 2013:209428.

23. Klem I, Wehinger C, Schneider B, Hartl E, Finsterer J, Stöllberger C. Diabetic atrial fibrillation patients: mortality and risk for stroke or embolism during a 10-year follow-up. Diabetes Metab Res Rev. 2003; 19:320–328.

24. EAFT (European Atrial Fibrillation Trial) Study Group. Secondary prevention in non-rheumatic atrial fibrillation after transient ischaemic attack or minor stroke. Lancet. 1993; 342:1255–1262.
25. Hart RG, Pearce LA, McBride R, Rothbart RM, Asinger RW. The Stroke Prevention in Atrial Fibrillation (SPAF) Investigators. Factors associated with ischemic stroke during aspirin therapy in atrial fibrillation: analysis of 2012 participants in the SPAF I-III clinical trials. Stroke. 1999; 30:1223–1229.

26. Sun Y, Hu D, Li K, Zhou Z. Predictors of stroke risk in native Chinese with nonrheumatic atrial fibrillation: retrospective investigation of hospitalized patients. Clin Cardiol. 2009; 32:76–81.

27. Lip GY, Brechin CM, Lane DA. The global burden of atrial fibrillation and stroke: a systematic review of the epidemiology of atrial fibrillation in regions outside North America and Europe. Chest. 2012; 142:1489–1498.

28. Lip GY. The role of aspirin for stroke prevention in atrial fibrillation. Nat Rev Cardiol. 2011; 8:602–606.

29. Benjamin EJ, Wolf PA, D'Agostino RB, Silbershatz H, Kannel WB, Levy D. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation. 1998; 98:946–952.
30. Aronow WS, Gutstein H, Hsieh FY. Risk factors for thromboembolic stroke in elderly patients with chronic atrial fibrillation. Am J Cardiol. 1989; 63:366–367.

31. Seidl K, Hauer B, Schwick NG, Zellner D, Zahn R, Senges J. Risk of thromboembolic events in patients with atrial flutter. Am J Cardiol. 1998; 82:580–583.

32. Risk factors for stroke and efficacy of antithrombotic therapy in atrial fibrillation. Analysis of pooled data from five randomized controlled trials. Arch Intern Med. 1994; 154:1449–1457.
33. Wang TJ, Massaro JM, Levy D, Vasan RS, Wolf PA, D'Agostino RB, et al. A risk score for predicting stroke or death in individuals with new-onset atrial fibrillation in the community: the Framingham Heart Study. JAMA. 2003; 290:1049–1056.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download