Abstract
Purpose
To analyze the results of surgical treatment for pathological fractures at the proximal femur.
Materials and Methods
Nineteen patients with a pathological fracture were included. The mean age was 65.7 years old. The patients comprised 8 males and 11 females. Primary tumors, types of pathological fractures, surgical procedures, and postoperative complications were recorded. Musculoskeletal Tumor Society (MSTS) functional score was used for functional evaluation. A Kaplan-Meier survival analysis was used to determine survival rate.
Results
The primary malignancies were 6 cases of breast cancer, 3 cases of lung cancer, 3 cases of renal cell carcinoma, 2 cases of cholangiocarcinoma, 2 cases of hepatocellular carcinoma, 1 case of esophageal cancer, 1 case of colon cancer, and 1 case of ovarian cancer. Pathological fractures included 8 cases of pertrochanteric fractures and 11 cases of subtrochanteric fractures. Intramedullary nailing was performed in 10 cases, and joint replacement surgery was performed in 9 cases. Postoperative complications included local recurrence in 1 case, infection in 1 case, and nail breakage in 1 case. The mean postoperative MSTS score was 21. The mean survival period was 10.6 months. Patient survival rates were 42.1% after 6 months, 26.3% after 12 months, and 10.5% after 24 months.
Conclusion
Surgical treatment of pathological fractures at the proximal femur provided early ambulation, and excellent pain relief. The surgery was well tolerated emotionally. Surgery is necessary for improving the quality of life in such patients; however, more cases of pathological fractures in these regions should be subjected to detailed analysis.
Since the beginning of the 1990s, advances in cancer diagnosis and various types of treatment have gradually led to increased survival in patients, combined with an increase in the population of elderly patients suffering from bone metastases. Up to 70% of patients suffering from malignant tumors develop bone metastases, which in the appendicular skeleton can cause intractable pain and severe functional impairment. Most of these patients can be treated non-surgically with chemotherapy, radiotherapy, and bisphosphonates. However, surgical treatment is a good option for patients with metastatic or impending pathological fractures, and solitary metastatic lesions.1,2 Malignancies from the breast, prostate, lung, kidney, and colon produce the highest rate of bone metastases.3 Treatment must be tailored individually, considering the estimated life expectancy and general condition of each patient.4 The treatment goals are to reduce pain and restore function for the duration of the expected life span. The proximal femur is a frequent site of bone metastases. Aside from pathological fractures of the femoral head and neck, which are best treated by hemiarthroplasty, surgical treatment of pathological fractures at the proximal femur varies substantially.3,5,6 Intramedullary nailing has been known to be the best treatment option.7,8 However, intralesional, marginal, or wide resection followed by nail, plate combined with polymethylmethacrylate (PMMA), or endoprosthetic joint replacement are also favoured.5,6
The need for a standardized system of end result studies of musculoskeletal tumor reconstructions was clearly recognized during the first International Symposium on Limb Salvage in 1981. Developmental experience increased with systematic and extensive field testing in 1989 by the Musculoskeletal Tumor Society (MSTS). The MSTS functional score system9 has been widely used as a standardized system of end result analysis after tumor reconstruction surgery. The strengths of this system are its ease of use, acceptance after extensive modifications, and field trials. The weaknesses are a degree of subjectivity that allows slight inter-observer variability and the compromises inherent to designing a system without high complexity that is applicable for unrestricted use in a number of different resections, reconstructions, and anatomic sites.
The aim of this study was to analyze patient survival, postoperative complications, and outcomes after surgical treatment for metastatic pathological fractures occurring at the proximal femur.
The study was performed with the approval of the Institutional Review Board at our institution. We performed a retrospective study of patients with pertrochanteric and subtrochanteric metastatic pathological fractures operated on between 2006 and 2012 at a single institution. Data on patient identity, age, sex, and primary tumor, as well as the types of pathological fractures, surgical procedures, and postoperative complications were collected. Patients with femoral head and neck pathological fractures were excluded. Preoperative evaluation included oncological staging in order to acquire information on the primary lesion and the presence of visceral or multiple bone metastases. Primary lesions were identified in all patients before surgery. Inclusion criteria were pathological fractures in the aforementioned region due to histologically proven metastases, resection of metastatic tissue, and joint replacement surgery or stabilization. Exclusion criteria were a primary bone tumor, an impending fracture, and multiple myeloma. No open fractures or direct extensions of metastatic tissue were seen.
Nineteen patients with a pathological fracture were included in this study. The mean age was 65.7 years (range, 42-87), the patients comprised 8 males and 11 females. The primary malignancies were 6 cases of breast cancer, 3 cases of lung cancer, 3 cases of renal cell carcinoma, 2 cases of cholangiocarcinoma, 2 cases of hepatocellular carcinoma, 1 case of esophageal cancer, 1 case of colon cancer, and 1 case of ovarian cancer. Pathological fractures comprised 8 cases in the pertrochanteric region and 11 cases in the subtrochanteric region (Table 1).
Plain radiographs, CT, and MRI scans were checked in all patients preoperatively to determine the optimal surgical approach (intramedullary nailing or joint replacement surgery), and the extent of tumor involvement around the fracture site and surrounding soft tissues. Endoprosthetic joint replacement surgery in the pertrochanteric pathological fractures was indicated in two main situations: 1) the bone destruction was large enough that intramedullary nailing could not be expected to provide a stable reconstruction; and 2) the patient's other systemic tumor burden was low or absent, and the metastases in question were not expected to respond to adjuvant treatment.
The MSTS functional score9 was used for clinical and functional evaluation after surgery. This score assigns numerical values (0-5) for each of the 6 categories; thus, the score ranges from 0 to 30. It is composed of three general categories (pain, function, and emotional acceptance) and three lower extremity specific categories (support, walking, and gait). A Kaplan-Meier survival analysis was used to determine the probability of patient survival. A p-value of less than 0.05 was considered significant.
Intramedullary nailing was performed in 10 cases. Intralesional resection by curettage and intralesional resection of extraosseous metastatic tissue via an additional incision at the fracture site was performed before inserting the intramedullary nail. The defect of the metastatic lesion was filled with PMMA in the bonding technique. Long proximal femoral nail antirotation (PFNA; Synthes, Solothurn, Switzerland) of the cephalomedullary nail device was used in all cases. The nail could be used to protect the entire femur by appropriately positioning the anti-rotational blade into the femoral head and neck proximally and through the distal femur. Intralesional curettage was performed before reaming and nailing to minimize direct tumor cell spreading along the femoral canal. Cementation was carried out after the final nailing, when the anti-rotational blade and distal interlocking screw insertions had been completed. We routinely added antibiotics to the cement used, as these patients had a high risk of infection. Partial weight bearing was allowed immediately after postoperative day 1, and full weight bearing was allowed within the first postoperative weeks.
Joint replacement surgery was performed in 9 cases using cemented hemiarthroplasties (MUTARS, Buxtehude, Germany). Extra-articular resection of the proximal femur including fracture site was performed via a posterior approach of the hip. Upon cementing femoral components and repairing appropriate soft tissue, patients were allowed bear weight by postoperative days 3-5.
The mean postoperative MSTS functional score was 21 (range, 16-25). The scores for pain (4.1) and emotional acceptance (4.0) revealed excellent results among the six categories of the scoring system. Function, support, walking, and gait showed more than moderate results (Table 2). There were no statistically significant differences between intramedullary nailing and joint replacement surgery (p>0.05). Twelve patients (63%) regained their preoperative mobility level.
A total of three postoperative complications (16%) occurred. These were 1 case of local recurrence, 1 case of infection, and 1 case of nail breakage. The case of local recurrence was detected at postoperative 5 months, and treated by adjuvant radiation therapy to control the locally recurred mass. The case of infection was controlled by incision and debridement, while the case of nail breakage occurred in a 45-year-old female patient with a subtrochanteric pathological fracture due to disseminated breast cancer. In this case, long PFNA (Synthes, Solothurn, Switzerland) was used for stable fixation with additional bone cement injections. As the proximal part of the nail just above the insertion site of antirotation blade had broken at two and a half months postoperatively, the broken intramedullary nail was removed, and resection of the proximal part of the femur was followed by joint replacement surgery with a bipolar hemiarthroplasty.
Mean survival period was 10.6 months (range, 1-53). Patient survival rates measured using the Kaplan-Meier method were 42.1% after 6 months, 26.3% after 12 months, and 10.5% after 24 months (Fig. 1).
Pathological fractures of the long bones are a common complication of bone metastases caused by various types of primary malignancies. The reported incidence of bone metastasis is up to 50% of all cancer patients.10 Approximately 50% of primary malignant tumors may affect the skeleton, which is subsequently the third most frequent site of metastases after the lung and liver.11 The reported incidence of bone metastases in breast, multiple myeloma, lung, prostate, and kidney cancers is up to 25% and 100%.12
The life expectancy of patients with bone metastases has remarkably increased over recent years due to improvements in chemotherapy, radiation therapy, and other oncological treatments. This increased life expectancy has led to a higher incidence of bone metastases and an increased risk of pathological fractures.11 The incidence of pathological fractures of the long bones is approximately 10% in patients with bone metastases.6,12,13,14 Pathological fractures of the long bone may be indicative of the terminal stage in the malignant process. It is the ultimate progression of the primary disease and the cause of death; as such, the majority of these patients have a limited life expectancy. Therefore, a realistic estimation of patient life expectancy is essential for planning an appropriate fracture treatment strategy for each patient.
Pathological fracture of a long bone, especially the femur, is one of the debilitating complications in a patient with an advanced stage of malignancy. Metastatic locations of the femur can be divided into five regions: the femoral head and neck, the pertrochanteric region, the subtrochanteric region, the femoral diaphysis, and the distal femoral region. Surgical options of pathological fractures should be tailored based on anatomical locations. Pathological fractures of femoral head and neck are best treated by hemiarthroplasty.3,5,6 Conversely, intramedullary nail is the procedure of choice for diaphyseal pathological fractures of the femur.7,8 However, conventional nailing is not enough to protect the femoral neck; thus, a reconstruction nail with a cephalic screw or endoprosthetic reconstruction is needed to cover the femoral neck and pertrochanteric region. There are a number of newly designed nails with reports of satisfactory results, such as the Russell-Taylor reconstruction nail, long proximal femoral nail antirotation, and the long gamma nail. The main indications of these nails are low and extended subtrochanteric fractures, ipsilateral trochanteric fractures, combined proximal and femoral shaft fractures, and pathological fractures. Among them, long proximal femoral nail antirotation has a helical blade. Antirotation action offers optimal stability with one single-locking implant into the femoral neck; thus, excellent anchorage of the blade is achieved in the femoral head without bone removal. The helical blade has better cut-out resistance; therefore, cases of cut-out or pull-out are far less common than other types.
Pathological fractures in the pertrochanteric region combined with severe bone loss and extraosseous metastatic tissue or large bone destruction are selectively treated by marginal or wide resection followed by endoprosthetic joint replacement surgery. Proximal femoral replacement surgery can be performed as a hemiarthroplasty or total hip arthroplasty (THA). Hemiarthroplasty has been favored due to satisfactory function, favorable expectancy, suitability for patients, and a lower risk of dislocation than THA.15,16,17 Selek, et al.18 advocate that, endoprosthetic reconstruction may be the optimal choice for metastatic lesions of the proximal femur. The goals of this procedure are independent of bone healing, increased functional capacity, pain relief, and provision of stable reconstruction. The patient can walk and bear weight on the bone, returning to daily activities early in the postoperative period, whereas patients treated by osteosynthesis with or without cement generally do not obtain satisfactory results. The causes of insufficient rigid fixation in the proximal femur with osteosynthesis include the weakness of the tumor region, heavy loading to the proximal femur, systemic effects of the primary cancer, and fusion failure due to adjuvant radiotherapy.19 Zacherl, et al.20 performed a comparative, retrospective double-center study to analyze the survival and influences on outcome according to the surgical technique (resection or stabilization) used to treat pathological proximal femoral fractures. They concluded that the median survival rates were not different between groups. Surgical complications were higher in the resection group (n=7) than in the stabilization group (n=3) without statistical significance.
We experienced one case of nail breakage, which was converted to resection of the proximal femur followed by joint replacement surgery with a bipolar hemiarthroplasty. We analyzed the probable mechanisms of nail fracture and submitted the case report to a journal with the literature review.21 It was the first reported failure of long proximal femoral nail antirotation. Zafiropoulos and Pratt22 reported a gamma nail fracture which occurred at a position similar to our case, at the insertion point of a lag screw into the intramedullary portion of the nail. They offered several hypotheses for the failure of the gamma nail, identifying voids and troughs in the fracture surface of the nail by scanning electron microscopy. These voids would have weakened the implants, and the troughs may have caused a ductile-type fracture of the implant. Our observations generally agreed with those by Zafiropoulos and Pratt22 in that our nail was also fractured at the weakest part, the antirotational blade-intramedullary nail intersurface, as was in their case of gamma nail fracture.
We agree with the opinion of Tillman23 that the orthopedic surgeon's role is to undertake prophylactic stabilization of at-risk lesions as well as stabilization or reconstruction of pathological fractures. Pathological fractures and limb bones at a high risk of fracture require recovery of activities of daily living and quality of life (QOL). Patients with solitary metastases in whom long survival is expected are also candidates for surgery performed to obtain local control.24 Surgical treatment of pathological fractures at the proximal femur provided excellent pain relief, restored the function of affected limb, and improved the QOL. Additional benefits after surgery were improvements in emotional acceptance, psychosocial well-being, and the ability for families to care for patients themselves. Appropriate care and support for most patients with pathological fractures at the proximal femur by optimal surgical options, is achievable by following the operative indications. Care and precaution are also necessary in the event of implant failure, which may occasionally require revision surgery.
Figures and Tables
Fig. 1
The Kaplan-Meier survival rates of patients at postoperative month 6, month 12, and month 24 (95% confidence interval).
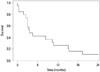
Table 1
Demographic Data of Patients

References
1. Bauer HC. Controversies in the surgical management of skeletal metastases. J Bone Joint Surg Br. 2005; 87:608–617.

3. Clarke HD, Damron TA, Sim FH. Head and neck replacement endoprosthesis for pathologic proximal femoral lesions. Clin Orthop Relat Res. 1998; 210–217.
4. Bauer HC, Wedin R. Survival after surgery for spinal and extremity metastases. Prognostication in 241 patients. Acta Orthop Scand. 1995; 66:143–146.

5. Capanna R, Campanacci DA. The treatment of metastases in the appendicular skeleton. J Bone Joint Surg Br. 2001; 83:471–481.

6. Wedin R, Bauer HC. Surgical treatment of skeletal metastatic lesions of the proximal femur: endoprosthesis or reconstruction nail. J Bone Joint Surg Br. 2005; 87:1653–1657.
7. van Doorn R, Stapert JW. Treatment of impending and actual pathological femoral fractures with the long Gamma nail in The Netherlands. Eur J Surg. 2000; 166:247–254.

8. Sarahrudi K, Hora K, Heinz T, Millington S, Vécsei V. Treatment results of pathological fractures of the long bones: a retrospective analysis of 88 patients. Int Orthop. 2006; 30:519–524.

9. Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993; 241–246.

10. Landis SH, Murray T, Bolden S, Wingo PA. Cancer statistics, 1998. CA Cancer J Clin. 1998; 48:6–29.

11. Hage WD, Aboulafia AJ, Aboulafia DM. Incidence, location, and diagnostic evaluation of metastatic bone disease. Orthop Clin North Am. 2000; 31:515–528.

13. Böhm P, Huber J. The surgical treatment of bony metastases of the spine and limbs. J Bone Joint Surg Br. 2002; 84:521–529.

14. Wedin R, Bauer HC, Wersäll P. Failures after operation for skeletal metastatic lesions of long bones. Clin Orthop Relat Res. 1999; 128–139.

15. Steinbrink K. Total femoral prosthesis: 18 years experience in 147 cases. In : Tan SK, editor. Limb Salvage: Current trends. Singapore: International Society of Limb Salvage;1993. p. 411–412.
16. Ward WG, Dorey F, Eckardt JJ. Total femoral endoprosthetic reconstruction. Clin Orthop Relat Res. 1995; 1:195–206.

17. Ward WG, Johnston KS, Dorey FJ, Eckardt JJ. Loosening of massive proximal femoral cemented endoprostheses. Radiographic evidence of loosening mechanism. J Arthroplasty. 1997; 12:741–750.
18. Selek H, Başarir K, Yildiz Y, Sağlik Y. Cemented endoprosthetic replacement for metastatic bone disease in the proximal femur. J Arthroplasty. 2008; 23:112–117.

19. Wedin R, Bauer HC, Rutqvist LE. Surgical treatment for skeletal breast cancer metastases: a population-based study of 641 patients. Cancer. 2001; 92:257–262.

20. Zacherl M, Gruber G, Glehr M, Ofner-Kopeinig P, Radl R, Greitbauer M, et al. Surgery for pathological proximal femoral fractures, excluding femoral head and neck fractures: resection vs. stabilisation. Int Orthop. 2011; 35:1537–1543.

21. Choy WS, Kim KJ, Lee SK, Yang DS. Implant failure of long proximal femoral nail antirotation in patient with subtrochanteric pathologic fracture. Eur J Orthop Surg Traumatol. 2012; 22:609–612.
22. Zafiropoulos G, Pratt DJ. Fractured Gamma nail. Injury. 1994; 25:331–336.
23. Tillman RM. The role of the orthopaedic surgeon in metastatic disease of the appendicular skeleton. Working Party on Metastatic Bone Disease in Breast Cancer in the UK. J Bone Joint Surg Br. 1999; 81:1–2.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download