Abstract
Purpose
In Asians, nasal dorsal and tip augmentation procedures are usually performed at the same time, and most dorsal augmentations use implants. In this study, dorsal augmentation was given by various types of grafts using deep temporal fascia (DTF) for primary rhinoplasty cases using only autologous tissues to improve the curve of hump noses and depressions. For secondary rhinoplasty cases, DTF was used to improve implant demarcation and transparency. Such effectiveness and utility of DTF is discussed.
Materials and Methods
Between May 2009 and May 2012, we performed rhinoplasty using DTF in 175 patients, which included 78 secondary surgery patients and 128 female patients. The mean age of the patients was 31.4. DTF was utilized with various types of grafts without implants to improve the curve in dorsal augmentation of hump noses and cases that required curve betterment. DTF was used to improve implant demarcation and transparency for secondary cases.
In Asians, rhinoplasty for nasal dorsal augmentation is usually performed at the same time as tip plasty, unlike in Westerners. However, despite the great developments in tip plasty suitable for Asians through in-depth anatomical studies and various clinical trials, most cases of dorsal augmentation from the supratip to the radix still utilize implants such as silicone implants and Gore-Tex (W.L. Gore Associates, Flagstaff, AZ, USA). However, for the purpose of achieving a natural-looking outcome and minimizing the occurrence of secondary drawbacks such as inflammation, foreign body reaction, contracture, skin change, redness, demarcation, and transparency, dorsal augmentation using autogenous tissues such as various cartilages, including dermofat, and fat grafts have been performed in gradually increasing frequency in recent years. In particular, given that patients with hump relatively do not have much concern for the height of the bridge and would usually rather have the curve irregularity corrected, many patients prefer curve irregularity correction using only autologous tissues instead of implants.
Along with the increase in the use of autogenous tissue-based rhinoplasty, the utilization of deep temporal fascia (DTF) as a material for autogenous tissue grafts has also gradually increased. In addition, DTF can be used as a combined graft with cartilage or as direct augmentation material in free graft form for partial rhinoplastic dorsal and tip augmentation to create natural aesthetic lines or for improvement of undesired dorsum and tip deformity. As implants are still widely applied in overall dorsal augmentation for Asians despite the rapid increase in utilization of autogenous tissues, DTF is also considered very useful as a material that supplements implants and strengthens soft tissues in cases requiring covering of implant demarcation due to thin skin.
Numerous muscles, fascia, musculocutaneous flaps, and fasciocutaneous flaps were used in the reconstruction of soft tissue defects and congenital deformities.1,2,3,4,5,6,7 DTF is also broadly utilized as a material for reconstruction surgery of the face and exposed-tendon injuries. After Smith8 introduced the use of temporal fascia free flaps to cover ligaments, Brent and Byrd9 reported the use of the same for reconstructing ear defects, indicating that DTF had been widely utilized in facial and hand reconstructions.10
In accordance with its usefulness for reconstruction purposes, DTF is commonly used in aesthetic rhinoplasty.11,12 Deep temporal fascia possesses advantages such as sufficient volume for creating a smoother aesthetic dorsal contour, which needs to be achieved in dorsal and tip augmentations, and its natural appearance without irregularity. In addition, DTF is harvested within the same operative field; thus, scars are hidden, making it applicable as a material for various grafts used in rhinoplasty.
In this study, cases of variously applied deep temporal fascia are categorized according to graft methods, and the results are analyzed according to the causes of its application.13
This study included 175 patients (128 women and 47 men) who were eligible for follow up over the course of 6 months among patients who underwent rhinoplasty with DTF between May 2009 and May 2012. Of the patients included, 97 underwent primary surgery and 78 underwent secondary surgery at a mean age of 31.4. For primary surgery cases with no implants, DTF was used in various graft methods for radix and supratip depression augmentation for cases such as hump nose or for improvement of dorsum and tip deformities, depending on patients' conditions. For secondary surgery cases, DTF was used to reinforce thinned skin and soft tissues after removing thickened capsules for improvement of implant demarcation from contracture. Surgical outcomes were compared based on patients' objective pictures obtained before and after the surgery, along with assessments of patient satisfaction.
Rhinoplasty was performed in all 175 patients under sleep-induced local anesthesia. To harvest DTF, a 3-cm to 4-cm incision line was made straight to the temporal regions, along the posterior border of the patients' sideburns. Local infiltration was implemented using 2%lidocaine mixed with epinephrine diluted to 1:100000. After incision, glistening DTF was confirmed by dissecting the subcutaneous tissue and superficial temporal fascia, paying due attention to hair follicles and superficial temporal arteries and veins (Fig. 1). In accordance with graft use or the recipients' characteristics, superficial temporal fascia was included when volume or smoothly movable planes were needed (Fig. 2).14 The size of the DTF to be harvested was determined according to the amount required and then incised, avoiding the vessels in the temporal muscles.
In hump nose correction without an implant, curve irregularity mostly occurred on the radix above the hump and supratip area. It sometimes occurred on various places, such as the dorsum, tip, lateral wall, or alar crease. Such depressed areas were improved by combined grafts with cartilage or solely by fascia as a free graft method.
For a combined graft, cartilages from all available parts (auricular, septal, and costal cartilages) were diced into 0.5-mm to 1.0-mm sections using blades and then placed in 1-cc syringes with cut tips. The syringes were then wrapped with DTF and sutured with absorbable suture, thereby creating a pocket-like shape. The diced cartilages were injected, and the desired shape was created, followed by the suturing of the entrance of the fascia with a running locking suture (Fig. 3). When the superficial layer of the DTF was wrapped outwardly, it formed a smoothly movable plane that allowed the skin flap to move freely after the healing process.15 When the deep layer was wrapped outwardly, it was well fused with the peripheral tissues and contributed as a semi-structured graft.16 After performing tip plasty and other surgeries such as deviated nose correction and dorsal surgery, the graft was implanted in the necessary recipient and then fixed directly on the bottom surface or fixed by bolster suture after penetrating the glabellar skin with the suture. However, since the amount of cartilage in Asians excluding the rib cartilage is insufficient for whole-dorsal augmentation, using it to replace implants is cumbersome; therefore, a diced cartilage graft was applied only in 5 radix graft cases and 2 tip graft cases.
To improve the demarcation of various pure dorsal cartilage grafts that were already utilized in the dorsum, radix, supratip, or tip and to prevent demarcation of the cartilage without morselization or with slight morselization when these grafts were used in combination, DTF was used to cover the dorsal cartilage graft and thereby create a soft contour (Fig. 4).
When it was applied as a free graft, the harvested DTF was folded in more than 2 layers and fixed with absorbable sutures to maintain the folding, followed by radix augmentation in the hump nose. In the other regions, augmentation was performed for supratip depression and tip deformity using single or double-layered DTF that was fixed on the bottom surface with absorbable sutures (Fig. 5). For the free graft cases, overcorrection by 20-30%was targeted, considering the swollen fascia and possible resorption. For the radix graft cases, the graft was hooked by an absorbable suture and was then fixed transcutaneously through the glabella area with bolster sutures, where it remained until removal 5-7 days later.
Due to the increase in secondary rhinoplasty cases, DTF was applied to reinforce the thinned skin in order to improve implant contour transparency for the cases that required total capsulectomy for the correction of implant demarcation along the implant's lateral margin caused by capsular contracture, which happens frequently due to an infected capsule or inflammation. It was also applied as prevention for the cases that required extremely high implants inserted near the skin, as the skin gets too thin in such cases and frequently causes implant contour transparency.
The DTF was designed to cover beyond the lateral margin of the implant and fixed to the implant with absorbable sutures, followed by implant insertion. In cases where a single-layer free graft was used to cover implants, DTF was harvested by attaching the superficial temporal fascia, on its superficial side if necessary. When the superficial temporal fascia, which is a loose connective tissue, was placed underneath the skin, the soft tissues between the implant and the skin were added, and a smoothly moving plane was formed, which enabled the skin flap to move softly and naturally after healing (Fig. 6).15
The follow-up duration of the patients ranged from 6 months to 4 years, with a mean of 1.5 years. Of the 175 patients with DTF utilization, 142 (81%) manifested satisfactory outcomes for the radix, dorsal, and tip irregularities or implant contour transparency corrections, as intended before surgery (Figs. 7, 8, 9, 10).
In particular, for patients with hump who relatively did not have much concern for the height of the bridge yet generally wanted to correct the curve irregularity, DTF could be utilized as a very effective material for creating a natural contour by partial augmentation in primary cases and for creating a natural aesthetic line by correcting implant transparency or various demarcations related to the implant in secondary cases.
Of the 51 patients with combined grafts, 7 had wrappings with diced cartilage and 44 had combined grafts with cartilage; additionally, 124 had free grafts. The areas requiring correction were the radix (86 patients), the dorsum and tip (54 patients), and demarcation coverage of implant or dorsal rib graft (35 patients) (Table 1).
A total of 33 patients (19%) complained about undercorrection; 21 cases involved the radix and 12 involved the supratip. Out of these 33 patients, 27% underwent a combined graft, and 73% underwent a free graft. During surgery, most of the DTF itself was swollen; in considering the possibility of partial absorption, overcorrection by 20-30% immediately after the surgery was targeted; however, hardly any patients showed overcorrection. For the patients with undercorrection, 28 later underwent filler injection, fat grafting, AlloDerm grafting in the radix, and AlloDerm and cartilage grafting in the supratip and tip. There was one case of hematoma in the DTF donor site; the hematoma was removed on the first day after the surgery. Two patients complained of temporal traumatic alopecia, which improved 6 months later. Besides these cases, no complications or sequelae associated with the DTF harvest were encountered.
Regarding rhinoplasty, Asians differ from Westerners in terms of anatomical characteristics.17 They possess a low and flat nasal dorsum, a less-projected nasal tip, a retracted nasal columella, and wide nasal alae, with a non-aesthetic line due to weak alar cartilages and thick nasal tip skin formation.
To improve these features among Asians, cartilage-supported structural reconstruction, nasal tip plasty, and nasal dorsal augmentation are performed during rhinoplasty at the same time. In particular, nasal septum extension and several different columella graft methods are performed to improve the less-projected nasal tip and retracted columella,18 and alar spreader and nasal tip grafts were used to improve retracted nasal alar cartilages.19 Likewise, surgeries using various autogenous tissues with various tip plasty procedures have overcome several limitations in recent years, resulting in remarkable developments.
Despite the development of surgical methods using autogenous tissues, low nasal dorsal augmentations in Asians are still highly dependent on implants made of silicone or Gore-Tex. Although such implants are the most convenient, simple, and economically beneficial for obtaining an aesthetically acceptable nasal dorsum without donor site morbidity, drawbacks such as implant displacement, excessive skin tension, and skin discoloration lower patients' satisfaction and do not meet their expectations of ideal nasal shape. In particular, patients with thin skin often have implant demarcation and transparency issues, and more cases of secondary infection are being reported compared to surgeries with autogenous tissue. Moreover, with the possibilities of adverse effects, complications, and an unnatural appearance due to unfeasible and unreasonable insertion of the implants in a hump or deviated nose, many patients tend to minimize the utilization of implants and want a natural-looking outcome even when using implants.
DTF is a safe autogenous tissue material that has been considered useful not only for nasal dorsal irregularity corrections but also for implants in patients with thin skin. When a natural appearance is desired, DTF is also useful for improving radix depression, supratip depression in hump nose, and tip deformity using autogenous tissues only, without implants. In addition, this autogenous tissue material is considerably effective for reducing implant visibility and demarcation when implants are used; thus, DTF, which is abundant in Asians, can be used with several grafting methods.
Anatomically, temporal fascia is thin yet resistant to severe inflammation due to its sufficient blood volume. It is easy to harvest and can be harvested from the same operation field; additionally, the scar can be hidden by hair. Also, its thickness can be controlled by harvesting superficial temporal fascia together with it. Moreover, its histological cell-supportive properties minimize the absorption of grafted cartilages and play a role as a cast that provokes fusion with the other tissues.20,21
In rhinoplastic surgery, grafts using temporal fascia can be utilized in two forms, namely as a combined graft using cartilages together and as a free graft using DTF only.
A combined graft that wraps diced cartilages or covers pure cartilages using DTF minimizes edge palpability and visibility when grafting conventional pure cartilages. In addition, fascia acts as a scaffold, thereby improving the viability of cartilages, and displacement is decreased due to the rearrangement of the torque in the fascia, while displacement by the asymmetric bottoms of the graft surface is reduced.22
Among the combined grafts, the diced cartilage-fascia graft, first reported by Daniel,23 is widely utilized for nasal dorsal and radix augmentation. Cartilage harvested from any of the regions during surgery can be utilized. In the absence of infection, there was no absorption of the grafted cartilages, allowing the volume to be maintained. Also, all of the DTF used to wrap the cartilages survived with good blood circulation,22 a result likely attributable to the finding that fascia plays a role in the neoperichondrium.24 Given that the volume can be maintained due to the cell-supportive properties of fascia, which aid cartilage survival, overcorrection is almost unnecessary. In this process, the deep surface of temporal fascia is rougher and less slippery than the superficial surface; thus, creating pockets that allow the deep surface to be located outside to prevent the graft from moving results in better fusion with peripheral tissues.16 However, even if the cartilages are wrapped by temporal fascia, it is important to consider the possibility that the patient with a history of injury can show an unexpected irregularity after surgery due to a reduction in the survival rate of diced cartilages.25 When diced cartilage is wrapped in the tensor fascia lata, it is easier to handle because it is thicker than temporal fascia; however, tissues must be obtained from a different operation field and visible scars are left in the lateral thigh.26 When the diced cartilage is casted using fibrin glue without DTF and then inserted into the recipient site, no donor site morbidity would occur and surgery duration would be shortened as well; however, the casted cartilage dices can be breakable, and the use thereof is more expensive than using fascia.27
However, this diced cartilage-fascia procedure is cumbersome; securing a sufficient volume of cartilage needs to be considered first in rhinoplasty for Asians using autogenous tissues, except for rib cartilage, as Asians have a lower volume of septum cartilage than Westerners.28 For such reasons, methods have also been introduced that support the remaining L-strut using an absorbable plate as batten after harvesting as much as septal cartilage as possible.15,29,30 Likewise, even when the maximum amount of septal cartilage is obtained in Asians, grafting diced cartilage with DTF for the full length of the dorsum without utilizing rib cartilage is vastly insufficient in many cases, as most of the cartilage would be consumed for tip plasty. Furthermore, patients who undergo reoperation or who have had septal injury lack septal cartilage; thus, most of the diced cartilage graft with DTF is mainly utilized in the correction of radix graft or dorsal tip irregularity.
Cartilage graft with AlloDerm is advantageous in that it does not lead to donor site morbidity and it is convenient to handle; however, cartilage loss occurred in 30% of the cases. Wrapping the cartilages with Surgicel also reduced the viability of the cartilages owing to foreign body reaction, resulting in the increase of reoperation frequency.31,32,33
DTF free graft is used for correcting visible irregularities. In the past, many surgeons used pure cartilages to improve nasal dorsal irregularity and contour deformity. There were problems of palpable and visible contour of grafted cartilages. In addition, crushing cartilage in order to prevent these problems showed a maximum of 90% cartilage loss, depending on the crushing strength; therefore, unexpected irregularity and demarcation occurred in the long-term follow-up.31 To compensate for such disadvantages, DTF was used. Contour deformities and lack of volume were also resolved via grafting by covering or overlapping the temporal fascia in the areas of contour irregularity, radix depression, and supratip depression. Soft tissues can be reinforced with AlloDerm and CG CryoDerm; however, their use cannot prevent complications from reactions to foreign body.34
DTF free graft can be remarkably useful for improving implant demarcation. Capsular contracture induces the symptoms of implant contour visibility due to the thick contracted capsules and the widened borders on both sides of the implants. When the infected or thickened capsules from chronic inflammation are removed, the skin gets even thinner, suggesting that the demarcation and transparency of the inserted implant are possibly worsened. In such cases, soft tissues can be reinforced via free grafting of DTF, and the adverse effects such as implant transparency or contour demarcation or visibility are prevented by the wrapping of the implant.16 In cases using DTF for the purpose of improving implant demarcation, including more superficial fascia during DTF harvest is important, as superficial fascia reinforces soft tissues and acts as a smoothly moving plane. It is especially useful in the reoperation of patients with secondary infection due to exposed implant as DTF is resistant to wounds with severe inflammation. One study showed superior outcomes without secondary infection when using dorsal augmentation by covering silicone implants with DTF in cases of reconstruction immediately after foreign body removal due to infection that occurred from augmentation rhinoplasty with industrial silicone.14
The anatomical characteristics of DTF have many advantages for rhinoplasty. As it is thin, easy to shape, and strong without tearing, cartilage wrapping is convenient, regardless of whether diced or non-diced cartilage is used, irregularities are easily corrected by folding or covering, and it can be hidden naturally owing to its smooth edge. It also promotes a higher survival rate of grafted cartilages and provides resistance to wound infection. Moreover, fascia can very easily be harvested in the same operation field, and the superficial temporal fascia can be contained as well, depending on the required amount, size, and characteristics. Donor site scars are also acceptable, as they are hidden by the hair.
In Asian rhinoplasty, deep temporal fascia can be used in a combined graft method with various cartilages or used alone as a free graft for the improvement of radix, dorsal, and tip irregularities and shape in primary rhinoplasty and for the improvement of implant contour demarcation and transparency in secondary rhinoplasty. Hence, deep temporal fascia may be considered as a useful graft material for creating natural noses for Asians.
Figures and Tables
Fig. 1
DTF harvest. (A) The incision design for the harvest on the temporal region, located vertically upward in a straight line along the posterior border of the sideburn. (B) Glistening DTF can be identified when subcutaneous tissue and superficial temporal fascia are uncovered. In this image, the superficial temporal fascia is lifted up. The STF can be contained in the harvest. DTF, deep temporal fascia; STF, superficial temporal fascia.

Fig. 2
Harvested DTF. (A) DTF harvested alone. (B) DTF harvested with STF. As loose connective tissue is attached to the superficial surface, it can be utilized as a soft tissue supplement that can form a smoothly movable plane. DTF, deep temporal fascia; STF, superficial temporal fascia.

Fig. 3
Wrapping diced cartilage with DTF. (A) Injecting diced septal cartilage into DTF bag. (B) Radix graft. DTF, deep temporal fascia.

Fig. 4
Combined graft with cartilage. (A) Taking out and wrapping the rib cartilage with DTF. (B) Combined radix graft with conchal cartilage. (C) Combined graft with the derotation graft placed in supratip area. (D) Combined onlay graft with conchal cartilage. DTF, deep temporal fascia.

Fig. 5
DTF free graft. (A) Preparing radix graft by folding DTF into several layers. (B) Fixing radix graft by penetrating the suture through nose root skin with a needle. (C) Free DTF graft on radix. (D) Inserting DTF as a free graft in a case of supratip break. DTF, deep temporal fascia.

Fig. 6
DTF free graft for implant coverage. (A) After total capsulectomy, biofilm is visible inside the infected capsule. (B) Thinned dorsal skin after total capsulectomy. (C) DTF being grafted together covering the implant. DTF, deep temporal fascia.

Fig. 7
Case 1. Patient with deviated nose correction. Combined graft with diced cartilage as radix graft. (A and C) Preoperative photos. (B and D) 6 month postoperative photos.
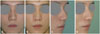
Fig. 8
Case 2. Patient with demarcated dorsal rib cartilage correction. Combined graft with full length rib cartilage. (A and C) Preoperative photos. (B and D) 6 month postoperative photos.

Fig. 9
Case 3. Patient with hump nose and broad bony vault correction. Free radix graft. (A and C) Preoperative photos. (B and D) 7 month postoperative photos.

Fig. 10
Case 4. Patient with contracted nose correction. Free graft for coverage of implant demarcation. (A and C) Preoperative photos. (B and D) 6 month postoperative photos.

Table 1
Summary of Patients According to Type of Graft

References
1. Aum JH, Kang DH, Oh SA, Gu JH. Orthodromic transfer of the temporalis muscle in incomplete facial nerve palsy. Arch Plast Surg. 2013; 40:348–352.
2. Jeong W, Son D, Yeo H, Jeong H, Kim J, Han K, et al. Anatomical and functional recovery of neurotized remnant rectus abdominis muscle in muscle-sparing pedicled transverse rectus abdominis musculocutaneous flap. Arch Plast Surg. 2013; 40:359–366.

3. Kang MJ, Chung CH, Chang YJ, Kim KH. Reconstruction of the lower extremity using free flaps. Arch Plast Surg. 2013; 40:575–583.

4. Kua EH, Leo KW, Ong YS, Cheng C, Tan BK. Vascularisation of urethral repairs with the gracilis muscle flap. Arch Plast Surg. 2013; 40:584–588.

5. Yoon SH, Burm JS, Yang WY, Kang SY. Vascularized bipedicled pericranial flaps for reconstruction of chronic scalp ulcer occurring after cranioplasty. Arch Plast Surg. 2013; 40:341–347.

6. Zayakova Y, Stanev A, Mihailov H, Pashaliev N. Application of local axial flaps to scalp reconstruction. Arch Plast Surg. 2013; 40:564–569.

7. Kim JH, Oh WS, Park SW, Kim KH. Various surgical procedures in the scale of upturned nose. J Korean Soc Aesthetic Plast Surg. 2010; 16:21–34.
9. Brent B, Byrd HS. Secondary ear reconstruction with cartilage grafts covered by axial, random, and free flaps of temporoparietal fascia. Plast Reconstr Surg. 1983; 72:141–152.
10. Abul-Hassan HS, von Drasek Ascher G, Acland RD. Surgical anatomy and blood supply of the fascial layers of the temporal region. Plast Reconstr Surg. 1986; 77:17–28.
11. Besharatizadeh R, Ozkan BT, Tabrizi R. Complete or a partial sheet of deep temporal fascial graft as a radix graft for radix augmentation. Eur Arch Otorhinolaryngol. 2011; 268:1449–1453.

12. Harel M, Margulis A. Dorsal augmentation with diced cartilage enclosed with temporal fascia in secondary endonasal rhinoplasty. Aesthet Surg J. 2013; 33:809–816.
13. Guerrerosantos J. Temporoparietal free fascia grafts in rhinoplasty. Plast Reconstr Surg. 1984; 74:465–475.

14. Lee KC, Ha SU, Park JM, Kim SK, Park SH, Kim JH. Foreign body removal and immediate nasal reconstruction with superficial temporal fascia. Aesthetic Plast Surg. 2006; 30:351–355.

15. Han K, Yeo HJ, Choi TH, Kim J, Son D. Rhinoplasty using various autogenous tissues. J Korean Soc Plast Reconstr Surg. 2010; 37:37–45.
16. Calvert J, Brenner K. Autogenous dorsal reconstruction: maximizing the utility of diced cartilage and fascia. Semin Plast Surg. 2008; 22:110–119.

17. Son D, Kwak M, Yun S, Yeo H, Kim J, Han K. Large auricular chondrocutaneous composite graft for nasal alar and columellar reconstruction. Arch Plast Surg. 2012; 39:323–328.

18. Dhong ES, Kim YJ, Suh MK. L-shaped columellar strut in East asian nasal tip plasty. Arch Plast Surg. 2013; 40:616–620.

19. Kim JH, Park SW, Oh WS, Lee JH. New classification for correction of alar retraction using the alar spreader graft. Aesthetic Plast Surg. 2012; 36:832–841.

20. Dubay DA, Wang X, Kirk S, Adamson B, Robson MC, Franz MG. Fascial fibroblast kinetic activity is increased during abdominal wall repair compared to dermal fibroblasts. Wound Repair Regen. 2004; 12:539–545.

21. Walter AJ, Morse AN, Leslie KO, Hentz JG, Cornella JL. Histologic evaluation of human cadaveric fascia lata in a rabbit vagina model. Int Urogynecol J Pelvic Floor Dysfunct. 2006; 17:136–142.

22. Kelly MH, Bulstrode NW, Waterhouse N. Versatility of diced cartilage-fascia grafts in dorsal nasal augmentation. Plast Reconstr Surg. 2007; 120:1654–1659.

23. Daniel RK. Diced cartilage grafts in rhinoplasty surgery: current techniques and applications. Plast Reconstr Surg. 2008; 122:1883–1891.

24. Calvert JW, Brenner K, DaCosta-Iyer M, Evans GR, Daniel RK. Histological analysis of human diced cartilage grafts. Plast Reconstr Surg. 2006; 118:230–236.

25. Arslan E, Majka C, Polat A. The fate of diced cartilage grafts of traumatized versus nontraumatized origin. Aesthetic Plast Surg. 2007; 31:365–371.

26. Kim YH, Kim JT. Nasal reconstruction with double-layer tensor fascia lata-wrapped diced rib cartilage in a patient with severe dorsal collapse. J Craniofac Surg. 2011; 22:628–630.

27. Tasman AJ. Advances in nasal dorsal augmentation with diced cartilage. Curr Opin Otolaryngol Head Neck Surg. 2013; 21:365–371.

28. McCurdy JA, Lam SM. Cosmetic surgery of the Asian face. 2nd ed. New York: Thieme;2005.
29. Kim JG, Rhee SC, Cho PD, Kim DJ, Lee SH. Absorbable plate as a perpendicular strut for acute saddle nose deformities. Arch Plast Surg. 2012; 39:113–117.

30. Kim JN, Choi HG, Kim SH, Park HJ, Shin DH, Jo DI, et al. The efficacy of bioabsorbable mesh as an internal splint in primary septoplasty. Arch Plast Surg. 2012; 39:561–564.

31. Cakmak O, Bircan S, Buyuklu F, Tuncer I, Dal T, Ozluoglu LN. Viability of crushed and diced cartilage grafts: a study in rabbits. Arch Facial Plast Surg. 2005; 7:21–26.
32. Erol OO. The Turkish delight: a pliable graft for rhinoplasty. Plast Reconstr Surg. 2000; 105:2229–2241.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download