Abstract
A 55-year-old woman presented with frequent episodes of syncope due to sinus pauses. During ambulatory Holter monitoring, atrial fibrillation and first-degree atrioventricular nodal block were observed. Magnetic resonance imaging and CT scans showed a tumor-like mass from the superior vena cava to the right atrial septum. Open chest cardiac biopsy was performed. The tumor was composed of proliferating IgG4-positive plasma cells and lymphocytes with surrounding sclerosis. The patient was diagnosed with IgG4-related sclerosing disease. Because of frequent sinus pauses and syncope, a permanent pacemaker was implanted. The cardiac mass was inoperable, but it did not progress during the one-year follow-up.
IgG4-related sclerosing disease is a systemic disease characterized by extensive IgG4-positive plasma cells and T-lymphocyte infiltration of various organs. Hamano, et al.1 reported that patients with sclerosing pancreatitis had a high serum IgG4 concentration with abundant and diffuse infiltration of IgG4-positive plasma cells in the pancreas. Since that original report, abundant IgG4-positive plasma cell infiltrates have been demonstrated in many extrapancreatic sclerotic lesions.2 Involvement of the heart in IgG4-related sclerosing disease is rare.3 The clinical presentation depends on the involved tissues; however, the histopathologic findings seem to be similar regardless of location.4 We report a case of IgG4-related sclerosing disease involving cardiac conduction system, that induced recurrent syncope in a middle aged female patient.
A 55-year-old woman was admitted to our institution with recurrent episodes of syncope and dizziness. She had no underlying disease, including autoimmune diseases. The patient's past medical history was not significant for any medications or illicit drugs. The electrocardiogram on admission showed first-degree atrioventricular block with a prolonged PR interval of 240 ms (Fig. 1A). Furthermore, the patient demonstrated atrial fibrillation (Fig. 1B) and a sinus pause of six seconds during an exercise test (Fig. 1C). During ambulatory Holter monitoring, frequent episodes of sinus pauses and atrial fibrillation were observed.
Transthoracic echocardiography and magnetic resonance imaging demonstrated a mass extending from the superior venacava (SVC)-right atrium (RA) junction to the right atrium posterior wall and interatrial septum (Fig. 2Aa). Fluorodeoxyglucose positron emission tomography showed increased uptake in a mass involving the RA wall and interatrial septum (Fig. 2Ab). No other evidence of abnormal uptake was noted. Transcutaneous cardiac biopsy was performed, however, failed to obtain enough tissue to confirm the histologic diagnosis. Therefore, the patient underwent open chest biopsy. Histologically, the lesion was composed of proliferating IgG4-positive plasma cells and lymphocytes (Fig. 3). The ratio of IgG4/IgG positive cells was 68% in average. And absolute number of IgG4-positive cells was approximate 146.5 per high-power field in the hottest area. These findings are consistent with IgG4-related sclerosing disease.2
The cardiac mass involved the SVC and interatrial septum, and was inoperable. Additional chemotherapy or steroid therapy was not performed because of patient's preference. A permanent VVI-type pacemaker was implanted due to frequent sinus pauses and syncope. During a one-year follow-up, the patient had no additional episodes of syncope, and the mass showed no evidence of progression (Fig 2Ac and B).
IgG4-related sclerosing disease is a relatively newly found entity with distinct clinicopathologic characteristics. The disease was originally discovered in patients with autoimmune pancreatitis and an elevated serum level of IgG4. It is characterized by extensive IgG4-positive plasma cells and T lymphocyte infiltration of various organs. Cardiac involvement of this disease is extremely rare. Recent reports described cardiovascular IgG4-related sclerosing disease as pericarditis and periarteritis related to heart failure or angina.5-7 However, to our knowledge, involvement of the cardiac conduction system has not been reported.
The cause and clinical progress of IgG4-related sclerosing disease remain undefined. Some studies report a rapidly fatal outcome of this disease.8 As the cause is unknown, there is no consensus on the optimal treatment approach. IgG4-related sclerosing disease has previously been suggested to be managed by corticosteroid and/or immunosuppressive therapies.9-11 In this case, we did not perform chemotherapy or corticosteroid therapy because of patient refusal. Instead, the patient's symptoms were managed by pacemaker implantation. Interestingly, tumor progression was not observed during a one-year follow-up period. Although the follow-up duration was short, we suggest that symptomatic management alone might be a possible option for treatment of this disease.
In summary, there has been no case in the literature of intracardiac IgG4-related sclerosing disease that involves the sinus and atrioventricular nodes. Our report suggests that IgG4-related sclerosing disease has a favorable prognosis and withhold steroid therapy. If there is no deterioration of symptoms, symptomatic management and regular follow-up might be a reasonable treatment option.
Figures and Tables
Fig. 1
(A) ECG taken on admission. First-degree AV block was observed with a PR interval of 240 ms. (B) Recovery phase during an exercise test. (C) Note the six-second sinus pause that was associated with dizziness. ECG, electrocardiogram; AV, atrioventricular.

Fig. 2
(Aa) Heart MRI showing a low-density mass lesion from the SVC and RA junction (left panel) to the right atrium of the heart (right panel). (Ab and Ac) Positron emission tomography-computed tomography showing increased FDG uptake at the SVC-RA junction and interartrial septum. (B) Heart multidetector computed tomography taken one year after diagnosis. No remarkable change of the mass. SVC, superior venacava; RA, right atrium; FDG, fluorodeoxyglucose.

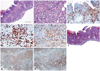
Fig. 3
(A) Low-power view showing multifocal vague lymphoid follicle formations (H-E ×40). (B) High-power view showing dense extensive lymphoplasmacytic infiltrations (H-E ×200). (C) IgG4 immunohistochemical staining shows many positive plasma cells (IgG4, ×100). (D and E) More than 50 IgG4-positive plasma cells are observed (D, IgG4 ×400). The ratio of IgG4/IgG positive cells is greater than 40% (E, IgG ×400). (F) Trichrome staining does not show markedly abundant collagen deposition. (G and H) The immunohistochemical staining for CD20 and CD3 reveals a lot of T cell infiltration, mainly in paracortical area.
ACKNOWLEDGEMENTS
This study was supported in part by research grants from Yonsei University College of Medicine (6-2009-0176, 6-2010-0059, 7-2009-0583, 7-2010-0676) and the Basic Science Research Program through the National Research Foundation of Korea, funded by the Ministry of Education, Science and Technology (2010-0021993 & 2010-0021092).
References
1. Hamano H, Kawa S, Horiuchi A, Unno H, Furuya N, Akamatsu T, et al. High serum IgG4 concentrations in patients with sclerosing pancreatitis. N Engl J Med. 2001; 344:732–738.

2. Cheuk W, Chan JK. IgG4-related sclerosing disease: a critical appraisal of an evolving clinicopathologic entity. Adv Anat Pathol. 2010; 17:303–332.
3. Ishizaka N, Sakamoto A, Imai Y, Terasaki F, Nagai R. Multifocal fibrosclerosis and IgG4-related disease involving the cardiovascular system. J Cardiol. 2012; 59:132–138.

4. Neild GH, Rodriguez-Justo M, Wall C, Connolly JO. Hyper-IgG4 disease: report and characterisation of a new disease. BMC Med. 2006; 4:23.

5. Inoue D, Zen Y, Abo H, Gabata T, Demachi H, Yoshikawa J, et al. Immunoglobulin G4-related periaortitis and periarteritis: CT findings in 17 patients. Radiology. 2011; 261:625–633.

6. Omura Y, Yoshioka K, Tsukamoto Y, Maeda I, Morikawa T, Konishi Y, et al. Multifocal fibrosclerosis combined with idiopathic retro-peritoneal and pericardial fibrosis. Intern Med. 2006; 45:461–464.

7. Baur M, Hulla W, Kienzer H, Klimpfinger M, Dittrich Ch. [Pericarditis as the initial manifestation of retroperitoneal fibrosis--a case report]. Wien Med Wochenschr. 2002; 152:230–232.
8. Sakamoto A, Nagai R, Saito K, Imai Y, Takahashi M, Hosoya Y, et al. Idiopathic retroperitoneal fibrosis, inflammatory aortic aneurysm, and inflammatory pericarditis--retrospective analysis of 11 case histories. J Cardiol. 2012; 59:139–146.

9. Kamisawa T, Egawa N, Nakajima H, Tsuruta K, Okamoto A. Morphological changes after steroid therapy in autoimmune pancreatitis. Scand J Gastroenterol. 2004; 39:1154–1158.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download