Abstract
Healthcare-associated infections caused by methicillin-resistant Staphylococcus aureus (MRSA) have recently become an important issue for healthcare facilities due to high rates of infection, mortality, and high treatment costs. We investigated the frequency of MRSA in healthcare workers (HCWs) via nasal carriage and assessed the performance of the LightCycler® MRSA Advanced test. We tested nasal swabs from the anterior nares of participating HCWs at an intensive care unit. Nasal swabs were identified as S. aureus, methicillin-sensitive or methicillin-resistant coagulase-negative staphylococci (MSCoNS or MRCoNS), or MRSA by using conventional culture and the LightCycler® MRSA Advanced test. Of the 142 HCWs who participated in this study, only 11 participants (7.8%) were MRSA-positive by conventional culture and MRSA ID, and 24 (16.9%) were positive for mecA by real time polymerase chain reaction (PCR). In terms of diagnostic performance, the LightCycler® MRSA Advanced test had a sensitivity of 100%, a specificity of 90.1%, a positive predictive value of 45.8%, and a negative predictive value of 100% compared with conventional culture method. The detection limit of the LightCycler® MRSA Advanced test was 103 colony/mL. We concluded that real-time PCR was able to rapidly and sensitively detect MRSA in HCWs. However, MRSA must be confirmed by culture due to false positivity.
Methicillin-resistant Staphylococcus aureus (MRSA) is a major pathogen that causes worldwide healthcare and community-acquired infections.1 MRSA infections are associated with high morbidity and mortality rates, prolonged hospital stays, increased costs, and increased use of medical and personnel resources.2,3
The primary sources of MRSA infections are infected patients, healthcare personnel, and medical devices in healthcare settings.4 According to meta-analysis, the average rate of MRSA colonization among healthcare workers (HCWs) is approximately 4.6% worldwide, and evidence suggests that HCWs are likely to play a large role in MRSA transmission.5 Rapid and accurate identification of HCWs and patients carrying MRSA would, therefore, be helpful for preventing transmission and early therapeutic decisions.
Resistance of S. aureus to methicillin is primarily mediated by the mecA gene, which codes for the modified penicillin-binding protein 2a (PBP2a) or PBP2'.6 The LightCycler® MRSA Advanced test (Roche Diagnostics GmbH, Mannheim, Germany) is a qualitative assay used for nasal swab specimens, and involves amplification of the mecA gene by polymerase chain reaction (PCR) and detection of amplified DNA using fluorogenic target-specific hybridization probes.
In this study, we investigated the prevalence of Staphylococcus nasal carriage among HCW and assessed the performance of the LightCycler® MRSA Advanced test.
Nasal swab samples were collected from the anterior nares of participating HCWs at an intensive care unit (ICU). A double-headed swab (double-headed BBL culture swab, Liquid Stuart, Becton-Dickinson; Sparks, MD, USA) was inserted into the nostril and rotated against the mucosa five times.
One swab head was directly streaked onto a MRSA ID (bioMeriuex, La Balme et Craponne, France) and blood agar medium to identify MRSA. The plates were incubated at 35℃ in O2 and reviewed after 24 hr and 48 hr. Suggestive MRSA colonies were confirmed as S. aureus by coagulase and DNase tests. Methicillin resistance was confirmed using the cefoxitin disk diffusion method according to Clinical and Laboratory Standards Institute guidelines.7
The LightCycler® MRSA Advanced test was performed on the LightCycler 2.0 instrument using the manufacturer's instructions. The swab extraction and mechanical lysis performed using the MagNA Lyser instrument. The real-time PCR amplification use fluorogenic target-specific hybridization probes for detection of amplified DNA. Each LightCycler MRSA advanced test reaction mixture contained an internal control to detect specimen inhibition and to monitor reagent integrity. The technologist hands-on time was 45 min for the LightCycler® MRSA Advanced test (Roche Diagnostics GmbH, Mannheim, Germany).1
The limits of detection were evaluated using S. aureus ATCC33591, a methicillin-resistant strain. The isolate was prepared as 106 CFU/mL saline suspension and absorbed onto double-headed swabs. The 106 suspension was then diluted 10-fold from 10 to 106 CFU/mL and also absorbed onto double headed swabs. Each suspension was subjected to duplicate tests.
The LightCycler® MRSA Advanced test was performed twice for each sample to determine specificity using reference strains ATCC33591 (MRSA), ATCC29213 (MSSA), ATCC14990 (MS S. epidermidis), ATCC25922 (E. coli), ATCC27853 (P. aeruginosa), ATCC700323 (E. cloacae), ATCC29212 (E. faecalis), ATCC34449 (C. listiniae), ATCC700327 (E. casseliflavus), and ATCC49619 (S. pneumoniae), and five clinical MRSA isolates, five methicilin-susceptible S. aureus (MSSA) isolates, five methicilin-resistnat coagulase-negative Staphylococcus (MRCoNS) isolates, and five methicilin-susceptible coagulase-negative Staphylococcus (MSCoNS) isolates.
Of the 142 HCWs who participated in this study, 51 were resident physicians, 51 were nurses, 19 were nursing auxiliaries, and 21 were physicians. Eleven participants (7.8%) were MRSA-positive according to conventional culture and MRSA ID, while 24 (16.9%) were positive for mecA according to real-time PCR. Among the 13 discordant specimens, 6 were MRCoNS, 4 were MSSA, and 3 were MSCoNS. These 13 isolates were retested with coagulase, DNase and cefoxitin disk diffusion test for distinguising from MRSA. The results of these biochemical tests were same as the results of the first tests. Additionally, we tested mecA PCR using following primers: primer MR1: ATG AGA TTA GGC ATC GTT CC (645-664); primer MR2: TGG ATG ACA GTA CCT GAG CC (1992-1173).8 Six MRCoNS among them showed resistance to 4 ug/mL cefoxitin disk and 4 MRCoNS were positive for mecA PCR. Therefore, we must consider further workup such as conventional culture, coagulase, and DNase for distinguising them from MRCoNS when positive in the LightCycler® MRSA Advanced test. However, we had a limitation about the accuracy of this PCR assay because we performed additional PCR using in-house primer. These in-house primers were not as good as the LightCycler® MRSA Advanced test. Further studies on the prevalence and clinical importance of mecA-positive MRCoNS are needed.
In terms of diagnostic performance, the LightCycler® MRSA Advanced test demonstrated 100% sensitivity, 90.1% specificity, 45.8% positive predictive value, and 100% negative predictive value compared with the conventional culture method. The detection limit of the LightCycler® MRSA Advanced test was 103 CFU/mL. As for analytical specificity, all tested non-S. aureus species were found negative for mecA by using the LightCycler® MRSA Advanced test.
Culture-based MRSA detection methods, even those that utilize screening agar, are time consuming and result in a 2-4 day turnaround time for accurate results. Because carriers can spread MRSA during this time period, rapid detection of personnel who has been colonized by this pathogen is crucial in MRSA surveillance programs.1 A variety of commercial molecular tests for detecting MRSA colonization that have high sensitivity and specificity and have potential for rapid detection were developed.9-13 In the present study, the LightCycler® MRSA Advanced test was found to be a rapid detection assay of MRSA with high sensitivity. Furthermore, the LightCycler® MRSA Advanced test had high sensitivity (100%) and good specificity (90.1%) compared with conventional culture methods (Table 1). However, the test demonstrated a high rate of false positives. Therefore, the presence of MRSA must be confirmed by culture.
We observed that 34 (23.9%) of the HCWs in our sample were carriers of S. aureus strains, and that MRSA represented 11 (32.4%) of these cases (i.e., 7.8% of HCWs surveyed) (Table 1). The carriage rate of S. aureus and MRSA in the present study was slightly higher than those reported by previous studies,4 however, our findings cannot be generalized because our sample consisted of ICU personnel.
In conclusion, the qualitative PCR amplification of mecA is a rapid and sensitive method for detecting MRSA in HCW. However, cultures must also be conducted to confirm results because of high rate of false positives when the PCR method is needed.
Figures and Tables
Table 1
Performance of the LightCycler® MRSA Advanced Test and ChromID MRSA Compared with Conventional Culture Methods
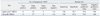
MRSA, Methicillin-resistant Staphylococcus aureus.
*S. aureus were 34 (23.9%) cases in conventional culture and 11 (32.4%) of these cases were MRSA.
†4 Methicillin-resistant coagulase negative staphylococci (MRCoNS) were positive for mecA PCR among 6 MRCoNS.
‡These isolates show pale green colony and identified as coagulase-negative staphylococci by futher biochemical tests.
ACKNOWLEDGEMENTS
This work was supported by a grant from the Kyung Hee University in 2011 (KHU-20110666).
References
1. Peterson LR, Liesenfeld O, Woods CW, Allen SD, Pombo D, Patel PA, et al. Multicenter evaluation of the LightCycler methicillin-resistant Staphylococcus aureus (MRSA) advanced test as a rapid method for detection of MRSA in nasal surveillance swabs. J Clin Microbiol. 2010; 48:1661–1666.

2. Francois P, Bento M, Renzi G, Harbarth S, Pittet D, Schrenzel J. Evaluation of three molecular assays for rapid identification of methicillin-resistant Staphylococcus aureus. J Clin Microbiol. 2007; 45:2011–2013.

3. Peterson LR, Hacek DM, Robicsek A. 5 Million Lives Campaign. Case study: an MRSA intervention at Evanston Northwestern Healthcare. Jt Comm J Qual Patient Saf. 2007; 33:732–738.

4. Safdar N, Bradley EA. The risk of infection after nasal colonization with Staphylococcus aureus. Am J Med. 2008; 121:310–315.

5. Albrich WC, Harbarth S. Health-care workers: source, vector, or victim of MRSA? Lancet Infect Dis. 2008; 8:289–301.

6. Berger-Bächi B, Rohrer S. Factors influencing methicillin resistance in staphylococci. Arch Microbiol. 2002; 178:165–171.

7. National Committee for Clinical Laboratory Standards. Performance standards for antimicrobial susceptibility testing: twenty-first informational supplement. Wayne, PA: Clinical and Laboratory Standards Institute M100-S21;2011.
8. Yang HY, Suh JT, Lee HJ. Evaluation of commercial selective agars in screening for methicillin-resistant Staphylococcus aureus. Ann Clin Lab Sci. 2010; 40:252–256.
9. Bischof LJ, Lapsley L, Fontecchio K, Jacosalem D, Young C, Hankerd R, et al. Comparison of chromogenic media to BD GeneOhm methicillin-resistant Staphylococcus aureus (MRSA) PCR for detection of MRSA in nasal swabs. J Clin Microbiol. 2009; 47:2281–2283.

10. Kelley PG, Grabsch EA, Howden BP, Gao W, Grayson ML. Comparison of the Xpert methicillin-resistant Staphylococcus aureus (MRSA) assay, BD GeneOhm MRSA assay, and culture for detection of nasal and cutaneous groin colonization by MRSA. J Clin Microbiol. 2009; 47:3769–3772.

11. Paule SM, Hacek DM, Kufner B, Truchon K, Thomson RB Jr, Kaul KL, et al. Performance of the BD GeneOhm methicillin-resistant Staphylococcus aureus test before and during high-volume clinical use. J Clin Microbiol. 2007; 45:2993–2998.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download