Abstract
Purpose
To compare preoperative and postoperative ocular biometry in patients with iris-fixated phakic intraocular lens (pIOLs): Artisan and Artiflex.
Materials and Methods
This study included 40 eyes with Artisan and 36 eyes with Artiflex pIOL implants. Anterior chamber depth (ACD) and axial length (AL) were measured by applanation ultrasonography (A-scan) and partial coherence interferometry (IOLMaster) preoperatively and 3 months after pIOL implantation.
Results
ACD measurements after Artisan or Artiflex pIOL implantation were smaller than preoperative measurements. Specifically, the difference after Artisan pIOL implantation was -1.07±0.17 mm by A-scan and -0.08±0.08 mm by IOLMaster. The difference after Artiflex pIOL implantation was -1.31±0.15 mm by A-scan and -0.05±0.07 mm by IOLMaster. After Artisan pIOL implantation, differences in AL measurements by A-scan were insignificant (difference: -0.03±0.15 mm), whereas postoperative AL measurements by IOLMaster were significantly longer than preoperative measurements (difference: 0.12±0.07 mm). After Artiflex pIOL implantation, AL measurements by both A-scan and IOLMaster were significantly longer than preoperative measurements (difference: 0.09±0.16 mm by A-scan and 0.07±0.10 mm by IOLMaster). In the Artiflex group, differences in AL measurements by A-scan correlated with the central thickness of the Artiflex pIOL.
Phakic intraocular lenses (pIOLs) have become common for correcting high refractive errors and these lenses were proven an effective and safe option to treat high myopia.1-3 However, complications have also been reported after pIOL implantation, which include endothelial cell loss,4 retinal detachment,5 traumatic aniridia,6 IOL dislocation, pigment dispersion syndrome, and glaucoma.7 PIOL implantations may increase the speed of cataract development due to intraoperative surgical trauma, postoperative inflammation, and the postoperative use of topical steroids.7-9 There is a direct relationship between the development of lens opacity and high myopia.7 With an increasing number of pIOL implantations, there will also be an increase in the number of patients presenting with cataracts; whether induced by the pIOLs or aging alone.
In patients with a history of iris-fixated pIOL implantation, explantation of the pIOL and cataract surgery can be done simultaneously or cataract extraction can be performed separately after adequate healing from the pIOL explantation. Combined surgery requires a shorter rehabilitation period but the surgeon should determine the IOL power with biometry measured with the pIOL implantation condition. Therefore, the surgeon needs to be aware of potential ocular biometry measurement errors in eyes with pIOLs.
The presence of a pIOL is known to affect ocular biometric measurement because the speed of the ultrasound through the various materials of pIOLs is different from the average velocity used to measure the eye. Although Hoffer10 published a formula by which to correct this error, some studies suggested that use of the correction factor may be inadvisable.7,11-13 One study reported that the axial length (AL) measured by IOLMaster is not significantly affected by Visian Implantable Collamer Lens (ICL) implantation.11 Other authors concluded that the change in AL, as measured by the immersion A-scan after Visian ICL implantation, is statistically insignificant.12 Another report reviewed several studies and found that the biometry and IOL power calculations are not distorted by the presence of a pIOL except in the case of silicone posterior chamber pIOLs.7
The aim of this study was to determine whether any biometric measurement errors occur in two types of iris-fixated pIOLs made of different materials: Artisan and Artiflex pIOLs made of polymethylmethacrylate (PMMA) and silicone, respectively. In addition, we used both A-scan ultrasonography and IOLMaster to measure ocular biometry. These devices use different techniques for measuring ocular biometry, which aids in determining how the measurement errors are different based on the measuring device and pIOL materials.
This study included 40 eyes from 24 patients with Artisan pIOL implants and 36 eyes from 20 patients with Artiflex pIOL implants. Both surgical treatments were performed by a single surgeon (J. B. L.). Before surgery, patients were given a detailed explanation of the surgery process and medical implications. All patients signed a written consent form in accordance with the Helsinki Declaration. Local Institutional Review Board approval was obtained. Inclusion criteria consisted of patients with preoperative manifested refractive errors of -3.0 to -15.0 diopter with no history of glaucoma, no history of corneal, lenticular, or retinal diseases, or any medical disease likely to alter vision. Patients who had contraindications for pIOL implantation were excluded. These included patients with anterior chamber depth less than 3.2 mm, patients who had any angle and iris abnormalities, or corneal endothelial density less than 2000 cells/mm2. Ophthalmic examinations were performed preoperatively, including slit lamp microscopy, cycloplegic and manifest refractions, fundus examination, and intraocular pressure measurement with Goldmann applanation tonometry. Uncorrected visual acuities and best-corrected visual acuities were checked. Two weeks before surgery, patients received a peripheral iridectomy incision with a Nd:YAG laser, generally at the 12 o'clock position.
The Artisan pIOLs used in the study (models 206 and 204, Ophtec BV, Groningen, the Netherlands) are convex-concave iris-fixated lenses. The biomaterial of the single-piece compression-molded IOL is CQ-ultraviolet absorbing PMMA. Both models have an overall length of 8.5 mm. The central thickness of the myopic Artisan pIOL (-3 D to 23 D) is 0.14 mm.
All procedures were done using topical anesthesia with 0.5% proparacaine hydrochloride. A scleral tunnel incision was made at the 12 o'clock position with a width of 5.2 or 6.2 mm, depending on the IOL diameter. Two lateral paracenteses were created in the cornea at the 10 o'clock and a 2 o'clock position with a width of 1.5 mm. Acetylcholine was injected and the anterior chamber was filled with an 1% sodium hyaluronate. The Artisan pIOL was inserted from the 12 o'clock position and rotated into a horizontal position. The lens haptic was enclavated to a fold of the midperipheral iris stroma using an enclavation needle at the 3 o'clock and 9 o'clock meridians. The Artisan pIOL was centered over the pupil, and the remaining viscoelastic material was irrigated out of the anterior chamber. The incision was closed with a continuous 10-0 nylon suture.
Postoperative treatment included topical antibiotics and 0.1% fluorometholone applied four times daily for 2 weeks and then tapered.
The Artiflex pIOL (Ophtec BV, Groningen, the Netherlands) used in the study is a three piece lens. The flexible optic is made of ultraviolet absorbing silicone and the rigid haptics are made of Perspex CQ-ultraviolet absorbing PMMA. The optical part of the Artiflex pIOL has a 6.0-mm diameter. The lens has an overall length of 8.5 mm and a slight anterior and posterior vault. The central thickness of the myopic Artiflex pIOL is variable from 0.14 to 0.52 mm (0.33±0.10 mm).
A 3.2-mm clear corneal incision was performed at the 12 o'clock position, and two stab incisions were placed at the 10 o'clock and 2 o'clock positions in the direction of the enclavation sites. Acetylcholine was injected, and the anterior chamber was filled with a 1% sodium hyaluronate. The Artiflex pIOL was inserted from the 12 o'clock position and rotated into a horizontal position. The lens haptic was enclavated to a fold of the midperipheral iris stroma using an enclavation needle at the 3 o'clock and 9 o'clock meridians. The Artiflex pIOL was centered over the pupil, and remaining viscoelastic material was irrigated out of the anterior chamber. The clear corneal incision site was self-sealed with hydration.
Postoperative treatment included topical antibiotics and 0.1% fluorometholone applied four times a day for 2 weeks and then tapered.
Ocular biometry was measured by two devices: applanation ultrasonography A-scan (Sonomed A/B scan 5500, Sonomed Inc., Lake Success, NY, USA) and partial coherence interferometry (IOLMaster, Carl Zeiss Meditec AG, Jena, Germany). A-scan measures the time it takes the sound to traverse the eye and convert it to a linear value using a velocity formula where distance equals the velocity multiplied by the time. The velocity of sound through various materials is widely different and the average velocity for a normal range axial length eye is 1555 m/s. In contrast, IOLMaster uses partial coherence interferometry (PCI) to assess the AL and anterior chamber depth (ACD) by calculating the distance between the corneal and lens surfaces through lateral slit illumination. With the PCI technique, it is known that the AL measurement is less influenced by intraocular material (such as silicone oil) compared to A-scan ultrasonography.
Measurements were performed by an experienced technician at baseline and 3 months after surgery with default settings for the phakic eye (phakic mode). Ocular biometry measurements were first performed by IOLMaster and then by A-scan.
A paired t-test was used to compare the difference between preoperative and postoperative anterior chamber depth and axial length measurements. Measurement differences were calculated by subtracting the preoperative biometry measurement from the postoperative biometry measurement. Pearson correlation was used to analyze the relationship between the AL measurement difference, preoperative AL, and Artiflex pIOL central thickness. Chi-squared tests were used for the categorical variables sex and age. All analyses were conducted using SPSS for Windows (Statistical Product and Services Solutions, version 15.0, SPSS Inc., Chicago, IL, USA). A p-value less than 0.05 was considered to indicate statistical significance.
Clinical data before and after iris-fixated pIOL implantation are shown in Table 1. The preoperative spherical equivalent and postoperative spherical equivalent were different between the Artisan group and the Artiflex group (p<0.001 and p=0.014, respectively), whereas the difference for postoperative logarithm of the minimal angle of resolution uncorrected visual acuity (LogMAR UCVA) was not significant (p=0.509).
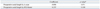
ACD measurements after Artisan and Artiflex pIOL implantation were smaller than preoperative ACD measurements (p<0.001). The measurement differences of both pIOLs by A-scan were more than 1 mm, whereas those for IOLMaster were less than 0.1 mm (Table 2).
Artisan pIOL implantation did not result in significant differences in AL measurement by A-scan (p=0.202), whereas postoperative AL measurements by IOLMaster were significantly longer than preoperative AL measurements (p<0.001). After Artiflex pIOL implantation, AL measurements by A-scan and IOLMaster were significantly longer than preoperative measurements (p=0.002 and p=0.001, respectively) (Table 3).
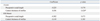
In the Artisan implantation group, there was no correlation between measurement differences in AL and preoperative AL measurements (p=0.971 by A-scan and p=0.108 by IOLMaster) (Table 4). In the Artiflex implantation group, pIOL central thickness measured by A-scan correlated with the difference in the AL measurement (coefficient: 0.356, p=0.028) (Fig. 1). Meanwhile, there was no correlation between measurement differences between AL and preoperative AL (p=0.174 by A-scan and p=0.073 by IOLMaster). There was also no correlation between the measurement difference in AL and the central thickness of Artiflex pIOL measured by IOLMaster (p=0.385) (Table 5).
Acquiring exact ocular biometry is critical in determining accurate IOL power in cataract surgery. In eyes with pIOL implants, possible errors in ocular biometric measurements caused by the presence of a pIOL may influence the IOL power calculation. A previous study showed that cataract surgery combined with explantation of the iris-fixated pIOL yielded acceptable predictability of spherical equivalents of -0.28±1.11 diopters.14 Moreover, some studies suggested that the correction factor may be inadvisable when measuring ocular biometry after pIOL implantation.7,11-13 However, to our knowledge, no biometry analysis completed after Artiflex pIOL implantation has been published until now.
We evaluated ACD before and after iris-fixated pIOL implantation. The ACD measured by A-scan after iris-fixated pIOL implantation was approximately 1 mm (1.07 mm in the Artisan group and 1.31 mm in the Artiflex group) shallower than the preoperative ACD. A-scan automatically calculates ACD from the first ultrasound peak to the aqueous/anterior lens interface peak.15 In eyes with pIOLs, this instrument was thought to detect the aqueous/phakic IOL interface as a second peak instead of the crystalline lens. Using the IOLMaster, ACD measurement differences after Artisan and Artiflex implantation were smaller than by A-scan (-0.08 mm in the Artisan group and -0.05 mm in the Artiflex group). The IOLMaster measures the ACD through lateral slit illumination and cannot measure recent pseudophakes.16 Considering the quantity of measurement differences, the IOLMaster calculated the distance between the corneal and crystalline lens surface-not the anterior surface of the iris-fixated pIOL. However, there were also significant changes in ACD measurements after pIOL implantation. These changes may be derived from pIOL reflections that influenced IOLMaster ACD measurements.
We compared AL before and after iris-fixated pIOL implantation. The optics biomaterials are different between Artisan and Artiflex pIOLs PMMA and silicone, respectively. The ultrasound velocities traveling through pIOLs are based on the pIOL material. Hoffer10 published a method to correct this error by using the following formula: ALcorrected=AL1555+(C×T), where AL1555=the measured AL of the eye at a sound velocity of 1555 m/s, T=the central thickness of the pIOL, and C=the material specific correction factor. The correction factor was +0.42 for PMMA and -0.59 for silicone. Using this formula, the AL measurement difference (postoperative AL minus preoperative AL) by A-scan after myopic Artisan pIOL implantation would be approximately -0.06 mm, whereas the AL measurement difference by A-scan after myopic Artiflex pIOL implantation would be approximately 0.08 to 0.31 mm (depending on the central thickness).
Additionally, Holladay17 has offered an optional method to measure AL through any implant by using following formula: Corrected AL Factor=T×(1-1532/V), where T=the central thickness of the pIOL, V=the sound velocity through that lens (PMMA 2660 m/sec, silicone 980 m/sec). Using this formula, the AL measurement difference (postoperative AL minus preoperative AL) after myopic Artisan pIOL implantation would be approximately -0.06 mm, whereas myopic Artiflex pIOL implantation would be approximately 0.08 to 0.29 mm (depending on the central thickness). In our study, the AL measurement difference after Artisan pIOL implantation by A-scan was -0.03±0.15 mm and that of Artiflex was 0.09±0.16 mm. Our findings were similar to those derived from the formula,10,17 although the difference in the Artisan group was not statistically significant. Additionally, AL measurement differences by A-scan correlated with the central thickness of the Artiflex pIOL. Thus, surgeons need to consider potential measurement errors especially in eyes with pIOLs and a high central thickness.
However, considering the measurement error of the A-scan, these differences were small and the average AL measurement differences may not have a major effect on IOL power. Other than the effect of ultrasound velocity, this result may be derived from the limitation of the errors in applanation ultrasound technique, which may be more difficult to accomplish.18 To eliminate the limitation of applanation ultrasonography, immersion A-scan can be performed.
IOLMaster partial coherence interferometry is a highly precise, contact-free, and observer-independent technique.19,20 Intraocular filling materials such as silicone oil affect the AL measured by IOLMaster less than by ultrasonography.21 In this study, AL measurement differences by IOLMaster after Artisan and Artiflex implantation were 0.12±0.07 mm and 0.07±0.10 mm, respectively. AL measurements were lengthened after the surgery and the differences between Artisan and Artiflex pIOL were statistically insignificant (p=0.155). These results indicated that AL measurements after pIOL implantation were longer than preoperative measurements by IOLMaster and that the pIOL material seems to have a relative lack of influence. Further studies investigating various pIOLs would be helpful. In addition, the standard deviation of the measurement difference determined by IOLMaster was smaller than that of the A-scan. These results show the advantage of IOLMaster over A-scan in terms of the effect of corneal indentation and patient cooperation.
In conclusion, ACD and AL measurements by A-scan and IOLMaster were influenced by iris-fixated pIOL implantation. Surgeons should consider potential errors caused by iris-fixated pIOLs when measuring ocular biometry.
Figures and Tables
Fig. 1
Correlation with measurement difference in axial length and central thickness of the Artiflex lens. *p<0.05.
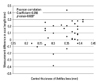
Table 1
Patient Characteristics and Clinical Outcomes
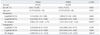
M, male; F, female; LogMAR, logarithm of the minimal angle of resolution; UCVA, uncorrected visual acuity; BCVA, best corrected visual acuity; SE, spherical equivalent.
Data are presented as mean±standard deviation; ( ) indicates the range of values.
*Statistically significant difference between groups (p<0.05, chi-squared test).
Table 2
Anterior Chamber Depth Measurements before and after Iris-Fixated Phakic Intraocular Lens Implantation

Table 3
Axial Length Measurements before and after Iris-Fixated Phakic Intraocular Lens Implantation

ACKNOWLEDGEMENTS
This study was supported by grant MEST (2010-0022006) from the National Research Foundation of Korea and the Converging Research Center Program funded by the Ministry of Education, Science and Technology (2012K001354).
References
1. Huang D, Schallhorn SC, Sugar A, Farjo AA, Majmudar PA, Trattler WB, et al. Phakic intraocular lens implantation for the correction of myopia: a report by the American Academy of Ophthalmology. Ophthalmology. 2009; 116:2244–2258.

2. Stulting RD, John ME, Maloney RK, Assil KK, Arrowsmith PN, Thompson VM. U.S. Verisyse Study Group. Three-year results of Artisan/Verisyse phakic intraocular lens implantation. Results of the United States Food And Drug Administration clinical trial. Ophthalmology. 2008; 115:464–472.e1.

3. Dick HB, Budo C, Malecaze F, Güell JL, Marinho AA, Nuijts RM, et al. Foldable Artiflex phakic intraocular lens for the correction of myopia: two-year follow-up results of a prospective European multicenter study. Ophthalmology. 2009; 116:671–677.

4. Saxena R, Boekhoorn SS, Mulder PG, Noordzij B, van Rij G, Luyten GP. Long-term follow-up of endothelial cell change after Artisan phakic intraocular lens implantation. Ophthalmology. 2008; 115:608–613.e1.

5. Georgalas I, Petrou P, Papaconstantinou D, Koutsandrea C, Ladas I. Bilateral giant tear-associated retinal detachment following Artisan phakic intraocular lens implantation for correction of moderate myopia. Acta Ophthalmol. 2010; 88:e143–e144.

6. Lee SJ. Traumatic aniridia and aphakia after Artisan intraocular lens implantation. J Cataract Refract Surg. 2007; 33:1341–1342.

7. Chen LJ, Chang YJ, Kuo JC, Rajagopal R, Azar DT. Metaanalysis of cataract development after phakic intraocular lens surgery. J Cataract Refract Surg. 2008; 34:1181–1200.

8. Moshirfar M, Mifflin M, Wong G, Chang JC. Cataract surgery following phakic intraocular lens implantation. Curr Opin Ophthalmol. 2010; 21:39–44.

9. Kohnen T, Kook D, Morral M, Güell JL. Phakic intraocular lenses: part 2: results and complications. J Cataract Refract Surg. 2010; 36:2168–2194.
10. Hoffer KJ. Ultrasound axial length measurement in biphakic eyes. J Cataract Refract Surg. 2003; 29:961–965.

11. Sanders DR, Bernitsky DA, Harton PJ Jr, Rivera RR. The Visian myopic implantable collamer lens does not significantly affect axial length measurement with the IOLMaster. J Refract Surg. 2008; 24:957–959.

12. Khokhar SK, Agarwal T, Dave V. Comparison of preoperative and postoperative axial length measurement with immersion A-scan in ICL cases. J Cataract Refract Surg. 2009; 35:2168–2169.

13. Pitault G, Leboeuf C, Leroux les Jardins S, Auclin F, Chong-Sit D, Baudouin C. [Optical biometry of eyes corrected by phakic intraocular lenses]. J Fr Ophtalmol. 2005; 28:1052–1057.
14. de Vries NE, Tahzib NG, Budo CJ, Webers CA, de Boer R, Hendrikse F, et al. Results of cataract surgery after implantation of an iris-fixated phakic intraocular lens. J Cataract Refract Surg. 2009; 35:121–126.

15. Vetrugno M, Cardascia N, Cardia L. Anterior chamber depth measured by two methods in myopic and hyperopic phakic IOL implant. Br J Ophthalmol. 2000; 84:1113–1116.

16. Sheng H, Bottjer CA, Bullimore MA. Ocular component measurement using the Zeiss IOLMaster. Optom Vis Sci. 2004; 81:27–34.

17. Holladay JT. Standardizing constants for ultrasonic biometry, keratometry, and intraocular lens power calculations. J Cataract Refract Surg. 1997; 23:1356–1370.

18. Hong JP, Nam SM, Kim TI, Seo KY, Lee SY, Meduri A, et al. Reliability of RTVue, Visante, and slit-lamp adapted ultrasonic pachymetry for central corneal thickness measurement. Yonsei Med J. 2012; 53:634–641.

19. Eleftheriadis H. IOLMaster biometry: refractive results of 100 consecutive cases. Br J Ophthalmol. 2003; 87:960–963.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download