Abstract
Purpose
To investigate the symptoms of attention deficit hyperactivity disorder (ADHD) as reported by parents in children with intermittent exotropia [X(T)] and to determine whether strabismus surgery for X(T) affects ADHD symptoms.
Materials and Methods
Fifty-one consecutive children undergoing muscle surgery for X(T) were prospectively recruited. One parent of each child completed the ADHD rating scale IV (ADHD RS-IV) assessment consecutively before and one year after surgery. Patients whose preoperative scores were above the cut-off point, the 90th percentile based on a Korean sample, were regarded as demonstrating the ADHD trait. The impact of muscle surgery on ADHD symptoms was assessed by comparing the preoperative scores with the post-operative scores.
Results
Eight (15.7%) of the 51 patients demonstrated the ADHD trait. ADHD RS-IV scores following strabismus surgery significantly decreased in patients with the ADHD trait (p=0.014), while they did not differ in patients without the ADHD trait. Seven (87.5%) of the 8 patients with the ADHD trait showed improvement in their ADHD RS-IV scores after surgery. There was no difference in surgical success rates between X(T) patients with and without the ADHD trait.
Surgical intervention in childhood intermittent exotropia [X(T)] aims to improve binocular function, appearance, and well-being.1-6 However, little attention has been given to the psychosocial effects of childhood strabismus surgery, because the methodology is not well developed and is more difficult to apply in children than in adults.7 A few investigators have started to explore the social and emotional status of strabismic children through parental surveys.7-11 Borsting, et al.9 and the convergence insufficiency treatment trial (CITT) study group11 used parental ratings of attention deficit hyperactivity disorder (ADHD) symptoms to evaluate school performance and the general quality of life in children with symptomatic convergence insufficiency (CI). They reported that children with CI had a higher frequency of parent-reported ADHD and/or learning problems, but their studies were limited to patients with CI and did not include the changes after correcting the CI.
Unlike other forms of strabismus, i.e. constant exotropia, there have been no reports of an increased prevalence of neurodevelopmental abnormalities in children with X(T).12,13 However, recently, one report suggested that children with X(T) may be at a higher risk for later psychiatric illness.14 As ADHD is one of the most common neuropsychiatric disorders in children and is thought to be associated with some forms of adulthood mental illness,15 investigating ADHD symptoms in children with X(T) is warranted. The present study, therefore, set out to examine the frequency of ADHD symptoms as rated by parents in children with untreated X(T) and after successful surgery thereof.
This study followed the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of Ajou University School of Medicine, Suwon, Korea. One parent provided written informed consent, and each child provided assent.
Fifty-one consecutive children undergoing muscle surgery for X(T) were prospectively recruited in this study. There were 22 boys and 29 girls ranging in age from 3 to 9 years (mean, 5.96±1.76 years). All patients had either divergence excess or basic type intermittent exotropia. Patients with convergence insufficiency type exotropia [near an angle greater than distance by more than 10 prism diopters (PD)]were excluded to eliminate possible confusion between CI-related symptoms and ADHD symptoms. Patients were also excluded if they had coexisting ocular pathology, such as amblyopia, anisometropia, congenital anomalies, or neurologic disorders. Patients with an existing diagnosis of a learning disability or ADHD were also excluded to eliminate potential bias. No patients had a history of previous ocular surgery.
One parent of each child was asked to complete the ADHD rating scale IV (ADHD RS-IV), based on the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition home version, in a separate room while the child performed other activities. The ADHD RS-IV consists of 18 questions to evaluate a broad range of school-related behaviors such as inattention (9 odd-numbered items) and hyperactivity (9 even-numbered items). We chose the ADHD RS-IV because it is one of the most commonly used scales for evaluating ADHD; has cut-off points for age, gender and setting; and has normalized data based on Korean samples.16 Parents were asked to rate the frequency of behaviors observed during the last month as follows: never, sometimes, often, or always. Each item was scored on an ordinal scale from 0 (never) to 3 (always), with a total score ranging from 0 to 54. Patients whose preoperative scores were above the cut-off point, the 90th percentile based on an age- and gender-matched Korean sample, were regarded to have the ADHD trait.17 This assessment was performed before and one year after surgery. The questionnaire was completed by the same parent of each patient and the results were masked to parents, patients, and the surgeon up to the final assessment.
All patients underwent symmetric lateral rectus recession on both eyes under general anesthesia, all of which were performed by the same strabismus specialist (JBL). The angles of deviation were measured with the alternating prism cover test before and one year after surgery. Surgical success was defined as an angle of deviation within 8 PD of orthophoria one year after surgery.
The Mann-Whitney U test, Wilcoxon signed rank test, and Fisher exact test were used to compare the preoperative and postoperative characteristics between the groups. SPSS software for Windows (Version 15.0, LEAD Technology, Inc., Chicago, IL, USA) was used to conduct these analyses. Linear logistic regression was performed to identify clinical factors related to the presence of the ADHD trait in patients with X(T). Probability values of less than 0.05 were considered to be statistically significant.
Preoperatively, the angle of exodeviation at distance fixation ranged from 18 to 50 PD (mean angle, 23.67±5.25 PD). All patients demonstrated visual acuity of better than 0.20 logMAR in either eye. Forty-five parents (88%) were able to provide a history of the duration of X(T).
Before surgery, 8 (15.6%) of the 51 patients demonstrated the ADHD trait. A greater proportion of the patients with X(T) demonstrated the ADHD trait than is reported in normal Korean children (11%).17 The clinical baseline characteristics were not different between the patients with and without the ADHD trait (Table 1). However, linear logistic regression analysis controlling for age and gender showed that having the ADHD trait was associated with a longer duration of X(T), as recognized by the parents (odds ratio=1.110, 95% confidence interval: 1.009-1.222; p=0.033), but was not associated with preoperative angle of deviation or refractive error in X(T) children. Demographic details of the patients with the ADHD trait are shown in Table 2.
After surgery, ADHD RS-IV scores of the patients with the ADHD trait decreased significantly (p=0.025, Wilcoxon signed rank test). Also, both inattention and hyperactivity subscales improved significantly (p=0.044 for inattention, p=0.016 for hyperactivity) (Fig. 1). In one half of the patients with the ADHD trait, the postoperative scores were within the normal range, as shown in Table 2. However, the patients without the ADHD trait showed no change in ADHD RS-IV scores following surgery.
There was no difference in surgical success rates between patients with and without the ADHD trait [6/8 (75%) vs. 31/43 (72.1%); p=0.865, Fisher exact test]. ADHD RS-IV scores tended to decrease with successful muscle surgery and tended to increase with unsuccessful surgery, but this result was not statistically significant (Table 3). Patients 3 and 4 (Table 2) demonstrated improvement in their scores despite unsuccessful surgical outcomes, and Patient 8 demonstrated an increase in his score despite surgical success.
This study indicates that a greater proportion of children with X(T) have the ADHD trait, as measured by the ADHD RS-IV, than the age- and gender-matched normal Korean sample. Our results are consistent with previous studies9,10,14 in the evaluation of the connection between exotropia or convergence insufficiency and ADHD. Mohney, et al.14 found that children, who were monitored up to a mean age of 20.3 years, with exotropia were 3.1 times more likely to develop a psychiatric disorder. As a subgroup in their study, 25 (17.7%) of the 141 exotropic patients were diagnosed with ADHD. However, their study made no distinction between the various forms of exotropia and simply described exotropia as a whole. Granet, et al.10 reported a three-fold greater incidence of ADHD among patients with CI, when compared with that of the general US population. Borsting, et al.9 found that school-aged children with symptomatic accommodative dysfunction or CI had a higher frequency of behaviors related to school under-performance and inattention, compared to a normative sample. It has been suggested that, because some of the symptoms of ADHD overlap with those of CI, the two conditions can be confused.9,10 Because patients with X(T) may also suffer from symptoms of CI and/or ADHD, this study investigated the relationship between ADHD and X(T) by comparing ADHD RS-IV scores before and after amelioration of X(T) and by excluding patients with CI.
In the present study, scores representing ADHD-related symptoms improved following muscle surgery for X(T). This improvement was particularly evident in patients with the ADHD trait. As the scores of ADHD were not changed in patients without the ADHD trait during the same follow-up, the effect of age on ADHD symptoms can be excluded in this study. Furthermore, the postoperative scores of half of the patients with the ADHD trait fell to within the normal range. This suggests that the presence of X(T) may lead to misdiagnosis, diagnostic confusion, and/or exacerbation of the symptoms of ADHD.
On the other hand, the surgical results did not affect the ADHD RS-IV scores after surgery. This finding was consistent with two previous studies7,8 that investigated the improvement in quality of life after childhood strabismus surgery. In those studies, improvement in quality of life dimension scores was not statistically different for patients with successful and unsuccessful surgical outcomes. Mruthyunjaya, et al.8 postulated that parental satisfaction can be good, even with unsuccessful outcomes, because some children may have an improved appearance relative to their preoperative state. Another possible explanation for subjective outcomes that are better than the objective outcomes is that a placebo effect of the surgery may also contribute to parental satisfaction.
Negative perception of strabismic individuals has been reported to develop in children at an early age and to affect how adult caretakers view children with whom they interact.5,6 Additionally, this study showed that higher scores on the ADHD RS-IV were associated with a longer duration of strabismus, as reported by parents. These findings, along with improvement in binocular function, support early surgical intervention for X(T).
The present study has several limitations. First, we evaluated ADHD-related symptoms, not the diagnosis of ADHD. To make the diagnosis of ADHD, a number of complex processes need to be undertaken, including psychiatric interviews. Therefore, our findings need to be treated with a degree of caution. Second, we relied upon parental reports for the presence of ADHD, and we did not confirm that a diagnosis had been made by a qualified professional. Additionally, the improvement of scores may be attributed to parental bias because the parents were not masked from the fact that their children underwent surgery. Third, our sample represented a pre-selected group of children with X(T) who were already scheduled to undergo muscle surgery. Our results may not apply to children who have milder cases of X(T). Fourth, our sample size was relatively small.
Further studies with a larger sample size or in subjects with a clinical diagnosis of ADHD are warranted.
Based on the results of our present study, children with X(T) have a higher frequency of ADHD-related symptoms, and these symptoms can improve with strabismus surgery. This suggests that childhood X(T) may contribute to ADHD-related symptoms.
Figures and Tables
Fig. 1
Box and whisker plots of scores on the ADHD rating scale based on DSM-IV diagnostic criteria (ADHD RS-IV) for exotropic children who had the ADHD trait and for those who did not. The scores were assessed before surgery (dark box) and one year after surgery (bright box). (A) Total ADHD RS-IV scores. (B) ADHD RS-IV scores in inattention. (C) ADHD RS-IV scores in hyperactivity. ADHD, attention deficit hyperactivity disorder; X(T), intermittent exotropia.

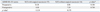
Table 1
Comparison of Baseline Clinical Characteristics of Children with Intermittent Exotropia Who Had the ADHD Trait with Children Who Did Not Have the Trait

Table 2
Demographic Details, Duration of X(T), Angle of Deviation, and ADHD RS-IV Scores of the 8 Exotropic Children with the ADHD Trait

References
1. Hatt SR, Leske DA, Adams WE, Kirgis PA, Bradley EA, Holmes JM. Quality of life in intermittent exotropia: child and parent concerns. Arch Ophthalmol. 2008. 126:1525–1529.
2. Wright K. Wright K, editor. Exotropia. Pediatric Ophthalmology and Strabsimus. 1995. 2nd ed. St Louis: Mosby Year Book;195–202.

3. Santiago AP, Ing MR, Kushner BJ, Rosenbaum AL. Rosenbaum AL, Santiago AP, editors. Intermittent exotropia. Clinical Strabismus Management: Principles and Surgical Techniques. 1999. Philadelphia: WB Saunders Co.;163–175.

4. von Noorden GK. von Noorden GK, Campos EC, editors. Exodeviations. Binocular Vision and Ocular Motility Theory and Management of Strabismus. 2002. 6th ed. St Louis: Mosby;356–376.
5. Paysse EA, Steele EA, McCreery KM, Wilhelmus KR, Coats DK. Age of the emergence of negative attitudes toward strabismus. J AAPOS. 2001. 5:361–366.

6. Uretmen O, Egrilmez S, Kose S, Pamukçu K, Akkin C, Palamar M. Negative social bias against children with strabismus. Acta Ophthalmol Scand. 2003. 81:138–142.

7. Archer SM, Musch DC, Wren PA, Guire KE, Del Monte MA. Social and emotional impact of strabismus surgery on quality of life in children. J AAPOS. 2005. 9:148–151.

8. Mruthyunjaya P, Simon JW, Pickering JD, Lininger LL. Subjective and objective outcomes of strabismus surgery in children. J Pediatr Ophthalmol Strabismus. 1996. 33:167–170.

9. Borsting E, Rouse M, Chu R. Measuring ADHD behaviors in children with symptomatic accommodative dysfunction or convergence insufficiency: a preliminary study. Optometry. 2005. 76:588–592.

10. Granet DB, Gomi CF, Ventura R, Miller-Scholte A. The relationship between convergence insufficiency and ADHD. Strabismus. 2005. 13:163–168.

11. Rouse M, Borsting E, Mitchell GL, Kulp MT, Scheiman M, Amster D, et al. Academic behaviors in children with convergence insufficiency with and without parent-reported ADHD. Optom Vis Sci. 2009. 86:1169–1177.

12. Buck D, Powell C, Cumberland P, Davis H, Dawson E, Rahi J, et al. Presenting features and early management of childhood intermittent exotropia in the UK: inception cohort study. Br J Ophthalmol. 2009. 93:1620–1624.

13. Robaei D, Rose KA, Kifley A, Cosstick M, Ip JM, Mitchell P. Factors associated with childhood strabismus: findings from a population-based study. Ophthalmology. 2006. 113:1146–1153.
14. Mohney BG, McKenzie JA, Capo JA, Nusz KJ, Mrazek D, Diehl NN. Mental illness in young adults who had strabismus as children. Pediatrics. 2008. 122:1033–1038.

15. Goldman LS, Genel M, Bezman RJ, Slanetz PJ. Council on Scientific Affairs, American Medical Association. Diagnosis and treatment of attention-deficit/hyperactivity disorder in children and adolescents. JAMA. 1998. 279:1100–1107.

16. Kim YS, So YK, Noh JS, Choi NK, Kim SJ, Koh YJ. Normative data on the Korean ADHD Rating Scales (K-ARS) for parents and teacher. J Korean Neuropsychiatr Assoc. 2003. 42:352–359.
17. Kim JW, Park KH, Choi MJ. Screening for attention deficit/hyperactivity disorder in community mental health services for children. J Korean Neuropsychiatr Assoc. 2004. 43:200–208.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download