Abstract
Purpose
Chronic low back pain is a common clinical problem. As medication, non-steroidal anti-inflammatory drugs are generally used; however, they are sometimes non-effective. Recently, opioids have been used for the treatment of chronic low back pain, and since 2010, transdermal fentanyl has been used to treat chronic non-cancer pain in Japan. The purpose of the current study was to examine the efficacy of transdermal fentanyl in the treatment of chronic low back pain.
Materials and Methods
This study included patients (n=62) that suffered from chronic low back pain and were non-responsive to non-steroidal anti-inflammatory drugs. Their conditions consisted of non-specific low back pain, multiple back operations, and specific low back pain awaiting surgery. Patients were given transdermal fentanyl for chronic low back pain. Scores of the visual analogue scale and the Oswestry Disability Index, as well as adverse events were evaluated before and after therapy.
Results
Overall, visual analogue scale scores and Oswestry Disability Index scores improved significantly after treatment. Transdermal fentanyl (12.5 to 50 µg/h) was effective in reducing low back pain in 45 of 62 patients; however, it was not effective in 17 patients. Patients who experienced the most improvement were those with specific low back pain awaiting surgery. Adverse events were seen in 40% of patients (constipation, 29%; nausea, 24%; itching, 24%).
Low back pain (LBP) is a common clinical problem and is of major socioeconomic importance. Although any of the spinal structures (intervertebral discs, facet joints, vertebral bodies, ligaments, and muscles) may be a source of LBP, the most likely cause is unclear.
Treatment for chronic LBP includes conservative therapy (exercise), intradiscal electrothermal therapy, spinal fusion, and artificial disc replacement. Several randomized trials have compared surgical and nonsurgical treatment of chronic LBP and have arrived at conflicting conclusions.1,2 Typical pharmacologic therapy of LBP begins with non-steroidal anti-inflammatory drug (NSAIDs) administration. NSAIDs are useful for mild to moderate LBP; however, they are not effective for severe LBP. Furthermore, they have a high risk of serious gastrointestinal bleeding.3
Oral morphine has been available for decades and is often used as a reference against which other treatments are compared.4 Patients with severe chronic LBP may require oral morphine for effective pain management. The use of oral morphine for treating chronic LBP has been increasing in recent years. However, adverse events and risk of addiction from the extended use of opioid therapy are concerns with this approach.5
Transdermal fentanyl may offer advantages over oral morphine and may be preferred by patients.6 Several large studies have demonstrated the efficacy and safety of transdermal fentanyl in patients with non-cancer pain.6,7 A controlled-released transdermal therapeutic system can provide systemic delivery of fentanyl at a constant rate for up to 72 hr.8
Since 2010, transdermal fentanyl was available for use in Japan to treat chronic non-cancer pain; however, its use in the treatment of chronic LBP has not been reported. The purpose of the current study was to examine the efficacy and tolerability of transdermal fentanyl for the treatment of chronic LBP in a Japanese population.
The ethics committee of our institution approved the protocol for the human procedures used in this study. Furthermore, the protocol and publication of the study were approved by our institutional review board. This trial was a prospective trial. The patients who participated in this study were selected from outpatients who attended our hospital for LBP. These 62 patients were selected from 412 LBP patients matched to the following criteria.
All patients had LBP for more than three months and were resistant to treatment with oral NSAIDs. Informed consent was obtained from each of the participants. Patients had non-specific chronic LBP, chronic LBP after lumbar surgery, multiple back operations, and specific LBP awaiting surgery (e.g., lumbar disc herniation or spinal stenosis).
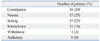
Table 1 shows patient demographic characteristics. The pain score was severe in all patients. All patients used NSAIDs; however, NSAIDs were not effective for LBP. The diagnosis was non-specific chronic LBP in 20 patients, LBP after single lumbar surgery in 15 patients, and multiple back operations in 15 patients. There were 12 patients who were awaiting lumbar surgery, including lumbar disc herniation and spinal canal stenosis, and had severe specific LBP. The patients were enrolled consecutively and were opioid-naïve.
A transdermal fentanyl patch (Janssen, Tokyo, Japan) was applied to all patients for the treatment of LBP. The patch was changed every three days. The starting dose was 12.5 µg/h. If this dose was not effective, it was increased to 25, 37.5 and 50 µg/h, thereafter. If one dose was non-effective for six days, the next highest dose patch was applied for six days. The maximum dose was 50 µg/h. If the patient's visual analogue scale (VAS) score did not decrease by 20%, we defined the medication as "non-effective".
Conservative treatment included exercise (walking, walking in a pool, muscle training, and muscle stretching). Walking and walking in a pool were performed by the patients on their own. Muscle training and stretching was performed for the abdomen and lower extremities by physical therapists. Medications, except for transdermal fentanyl, were allowed. Medications included NSAIDs, vitamins, muscle relaxants, and prostaglandin E1. A physician decided the type of medication for each patient.
We evaluated LBP before treatment, one month after treatment, and at final follow-up. Pain scores in patients with specific LBP awaiting surgery was evaluated at seven days before their surgery, which was considered as their final follow-up. If a patient stopped the medication (e.g., non-responder), the pain evaluation from seven days before the last dose was administered was recorded. For the evaluation of pain in all patients, scores from the VAS score (0, no pain; 10, worst pain) and the Oswestry Disability Index (ODI) score (0, no pain; 100, worst pain) were recorded and compared.
At four months after treatment, patients were asked to choose one of the following responses regarding their satisfaction with the treatment: 1) the medication met my expectations; 2) I did not improve as much as I had hoped, but I would undergo the same medication for the same outcome; 3) the medication helped, but I would not undergo the same medication for the same outcome; or 4) I am the same as or worse than I was before the medication.
All adverse events were reported together with an assessment of their severity (mild, moderate, severe) and the investigator's opinion of their relationship to treatment with transdermal fentanyl (none, unlikely, possible, or probable). Antiemetics were used in all patients. Laxatives were prescribed for constipation. Addiction was measured according to previous reports.9
Table 2 shows the dosage of transdermal fentanyl administered. The patients were administered doses from 12.5 to 50 µg/h. Most patients were administered 12.5 µg/h of transdermal fentanyl. The average dosage was 19.6±1.8 µg/h (mean±S.E.M.).
Table 3 shows the results of the evaluation of LBP after treatment in all 62 patients. VAS and ODI one month after treatment were 5.0±0.3 (mean±S.E.M.) and 32±6, respectively, and were significantly less than that before treatment (p<0.01). Mean VAS score and ODI score at final follow-up were 4.6±0.3 and 28±6, respectively, and were significantly lower than values obtained before treatment (p<0.01).
Transdermal fentanyl was very effective, especially in all patients with specific LBP awaiting surgery, so we divided the patients into the following three groups: 1) transdermal fentanyl was effective (responders), n=32; 2) transdermal fentanyl was effective in patients awaiting surgery (responders), n=12; and 3) transdermal fentanyl was not effective (non-responders), n=18 (Table 4). VAS scores and ODI scores were significantly lower after treatment than before treatment in the two responder groups (p<0.05). Also, VAS scores and ODI scores after treatment in the two responder groups were significantly lower than those of the non-responder group (p<0.05). However, pain scores one month after treatment and at final follow-up were not significantly lower than those of the non-responder group before treatment (p>0.05) (Fig. 1). On the other hand, transdermal fentanyl was more effective in the responders awaiting surgery compared with the other responders (p<0.05) (Fig. 2).
The average duration of treatment was significantly shorter in the non-responder group compared with the responder groups, because non-responders did want to continue with the transdermal fentanyl therapy (p<0.05) (Table 4). The average dosage of transdermal fentanyl in the non-responder group was significantly higher than that in each of the responder groups, because of the insufficiency of the drug (p<0.05) (Table 4).
Details of subjective outcomes after treatment are presented in Table 5. Subjective outcomes were good and fair in 27 and 15 patients, respectively; however, 12 patients and 8 patients reported an unexpected or poor outcome.
Table 6 shows the adverse events reported throughout follow-up. Adverse events were seen in 40% of all 62 patients. The most common adverse events were constipation, nausea, itching, and somnolence. Adverse events were mild in all patients. Itching was seen as a local reaction to the transdermal fentanyl patch. One patient (2%) showed withdrawal symptoms (loss of appetite and motivation) after stopping the transdermal fentanyl patch. However, addiction was not seen in any patient.
This is first study to evaluate the efficacy of transdermal fentanyl for the treatment of chronic LBP in a Japanese population. In general, transdermal fentanyl significantly improved folVAS scores and ODI scores in patients with chronic LBP, especially in patients with specific LBP awaiting surgery; however, it did not decrease pain in 27% of the patients with non-specific LBP or multiple back operations. Adverse events were seen in 40% of patients; however, no addiction was seen.
It has been reported that both weak and strong opioids are effective in the treatment of chronic LBP. Three double-blind RCTs compared opioids to an inactive placebo in the management of chronic LBP.10-12 In one US trial, 380 outpatients with chronic LBP were enrolled in an open-label phase study and treated with tramadol, followed by enrollment of those who tolerated tramadol into a double-blind, placebo-controlled phase study.10 Patients treated with tramadol scored significantly better on the VAS, the McGill Pain Questionnaire and the Roland Disability Questionnaire.10 In another US trial, patients with LBP were randomized to receive either tramadol/acetaminophen or a placebo for 91 days. Tramadol/acetaminophen significantly improved the final scores for VAS, the Roland Disability Questionnaire, and a 36-Item Short-Form Health Survey from baseline levels.11 In the third trial, 333 patients with chronic LBP were randomized to receive tramadol/acetaminophen or a placebo in Canada. The tramadol/acetaminophen combination showed efficacy in pain reduction, measures of physical functioning and quality of life.12
Several authors have reported the effectiveness of transdermal fentanyl for the treatment of chronic LBP.11,12 Allan, et al.13 compared the efficacy and safety of transdermal fentanyl and sustained-release morphine in strong-opioid-naïve patients with chronic LBP. Transdermal fentanyl was effective in the treatment of chronic LBP and was associated with less constipation compared with sustained-release morphine. Kosinski, et al.14 reported the efficacy of transdermal fentanyl in patients with chronic LBP and compared pain relief and patient's health-related quality of life score improvement. Health-related quality of life score improvement was greatest among patients experiencing the greatest pain relief from transdermal fentanyl. In the current study, transdermal fentanyl significantly improved VAS scores and ODI scores in Japanese patients with chronic LBP, and these findings are similar to those of other studies.
In the current study, transdermal fentanyl was more effective in patients who were awaiting surgery and had specific LBP due to apparent disc herniation or spinal stenosis, compared with the other responders or non-responders. Non-responders included patients with non-specific LBP and LBP after surgery, but did not include patients with specific LBP. Transdermal fentanyl was not effective at one month and final follow-up in non-responders. Furthermore, the average dosage of transdermal fentanyl was significantly higher in the non-responder group than in the responder groups because of the insufficiency of the drug. In a previous study, it was reported that there were no differences in age, sex, and type or duration of pain between responders and non-responders after the application of transdermal fentanyl.15 The difference in response to treatment between responders and non-responders could be detected at three weeks.15 Lack of response after one month had a stronger negative predictive value than the presence of response after one month. The most influential factors for predicting a response were employment status and use of high doses of opioids.15 Considering previous reports and the results of the current study, a lack of response after one month and use of a high dosage of opioids may have a negative predictive value for response to opioids.
Kalso, et al.16 analyzed available randomized, placebo-controlled trials of opioids for efficacy and safety in patients with chronic non-cancer pain. About 80% of patients experienced at least one adverse event, with constipation (41%), nausea (32%) and somnolence (29%) being the most common.16 As most of the studies analyzed were short-term follow-up studies, they did not allow for conclusions to be made concerning problems with tolerance and addiction.16 A systematic review revealed that opioids are commonly prescribed for chronic LBP and may be efficacious for short-term pain relief, but their long-term efficacy is unclear.17 Substance use disorders are common in patients taking opioids for back pain, and aberrant medication-taking behaviors occur in 5 to 24% of cases.15 In the current study, the most common adverse events reported were constipation, nausea, itching, and somnolence; however, addiction was not documented in any patient. The current results may be due to the short-term follow-up period of the study.
In conclusion, we evaluated the efficacy of transdermal fentanyl for severe chronic LBP in a Japanese population. Transdermal fentanyl significantly improved pain scores in 73% of patients with LBP; however, about 27% of patients demonstrated a non-response. Non-responders included patients with non-specific LBP and pain after lumbar surgery. Treatment was most effective in patients with specific LBP awaiting surgery, and pain relief was seen in all patients in that group. Adverse events were reported in 40% of all of the patients. In patients with chronic LBP resistant to NSAIDs, transdermal fentanyl may be a good therapeutic agent to reduce pain.
Figures and Tables
Fig. 1
VAS scores in responders and non-responders. Month 0=before treatment. VAS scores after treatment were significantly lower than those before treatment in the responder group at each time point (p<0.01). However, pain scores one month after treatment and at final follow-up did not differ significantly from those before treatment in the non-responder group (p>0.05). VAS, visual analogue scale.
Fig. 2
VAS scores in responders and non-responders. Month 0=before treatment. VAS scores after treatment in the two responder groups were significantly lower than those in the non-responder group at each time point (p<0.05). VAS scores after treatment indicated that transdermal fentanyl was more effective in the responders awaiting surgery compared with the other responders at each time point (p<0.05). VAS, visual analogue scale.
References
1. Mirza SK, Deyo RA. Systematic review of randomized trials comparing lumbar fusion surgery to nonoperative care for treatment of chronic back pain. Spine (Phila Pa 1976). 2007. 32:816–823.

2. Ohtori S, Koshi T, Yamashita M, Yamauchi K, Inoue G, Suzuki M, et al. Surgical versus nonsurgical treatment of selected patients with discogenic low back pain: a small-sized randomized trial. Spine (Phila Pa 1976). 2011. 36:347–354.

3. Wolfe MM, Lichtenstein DR, Singh G. Gastrointestinal toxicity of nonsteroidal antiinflammatory drugs. N Engl J Med. 1999. 340:1888–1899.

5. McNairy SL, Maruta T, Ivnik RJ, Swanson DW, Ilstrup DM. Prescription medication dependence and neuropsychologic function. Pain. 1984. 18:169–177.

6. Allan L, Hays H, Jensen NH, de Waroux BL, Bolt M, Donald R, et al. Randomised crossover trial of transdermal fentanyl and sustained release oral morphine for treating chronic non-cancer pain. BMJ. 2001. 322:1154–1158.
7. Franco ML, Seoane A. Usefulness of transdermal fentanyl in the management of nonmalignant chronic pain: a prospective, observational, multicenter study. Pain Clinic. 2002. 14:99–112.

8. Jeal W, Benfield P. Transdermal fentanyl. A review of its pharmacological properties and therapeutic efficacy in pain control. Drugs. 1997. 53:109–138.
9. Adams LL, Gatchel RJ, Robinson RC, Polatin P, Gajraj N, Deschner M, et al. Development of a self-report screening instrument for assessing potential opioid medication misuse in chronic pain patients. J Pain Symptom Manage. 2004. 27:440–459.

10. Schnitzer TJ, Gray WL, Paster RZ, Kamin M. Efficacy of tramadol in treatment of chronic low back pain. J Rheumatol. 2000. 27:772–778.
11. Ruoff GE, Rosenthal N, Jordan D, Karim R, Kamin M. Protocol CAPSS-112 Study Group. Tramadol/acetaminophen combination tablets for the treatment of chronic lower back pain: a multicenter, randomized, double-blind, placebo-controlled outpatient study. Clin Ther. 2003. 25:1123–1141.

12. Peloso PM, Fortin L, Beaulieu A, Kamin M, Rosenthal N. Protocol TRP-CAN-1 Study Group. Analgesic efficacy and safety of tramadol/acetaminophen combination tablets (Ultracet) in treatment of chronic low back pain: a multicenter, outpatient, randomized, double blind, placebo controlled trial. J Rheumatol. 2004. 31:2454–2463.
13. Allan L, Richarz U, Simpson K, Slappendel R. Transdermal fentanyl versus sustained release oral morphine in strong-opioid naïve patients with chronic low back pain. Spine (Phila Pa 1976). 2005. 30:2484–2490.

14. Kosinski MR, Schein JR, Vallow SM, Ascher S, Harte C, Shikiar R, et al. An observational study of health-related quality of life and pain outcomes in chronic low back pain patients treated with fentanyl transdermal system. Curr Med Res Opin. 2005. 21:849–862.

15. Kalso E, Simpson KH, Slappendel R, Dejonckheere J, Richarz U. Predicting long-term response to strong opioids in patients with low back pain: findings from a randomized, controlled trial of transdermal fentanyl and morphine. BMC Med. 2007. 5:39.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download