Abstract
Purpose
We performed this study to evaluate the safety of permissive hypotension management in extremely low birth weight infants (ELBWIs).
Materials and Methods
Medical records of all inborn ELBWIs admitted to Samsung Medical Center from January 2004 to December 2008 were reviewed retrospectively. Of a total of 261 ELBWIs, 47 (18%) required treatment for hypotension (group T), 110 (42%) remained normotensive (group N), and 104 (40%) experienced more than one episode of hypotension without treatment (group P) during the first 72 hours of life. Treatment of hypotension included inotropic support and/or fluid loading.
Results
Birth weight and Apgar scores were significantly lower in the T group than the other two groups. In the N group, the rate of pathologically confirmed maternal chorioamnionitis was significantly higher than other two groups, and the rate was higher in the P group than the T group. After adjusting for covariate factors, no significant differences in mortality and major morbidities were found between the N and P groups. However, the mortality rate and the incidence of intraventricular hemorrhage (≥stage 3) and bronchopulmonary dysplasia (≥moderate) were significantly higher in the T group than the other two groups. Long term neurodevelopmental outcomes were not significantly different between the N and P groups.
Early hypotension during the initial 3 days of life is common in preterm infants and the incidence of early hypotension has been reported to range between 20-50% in very low birth weight infants.1-3 Many studies have reported that hypotension might be related to cerebral hemorrhage and ischemia, and have demonstrated that hypotension is associated strongly with intraventricular hemorrhage (IVH) and periventricular leukomalacia.4,5 Fanaroff, et al.6 showed that infants treated for hypotension have higher mortality and worse morbidities, including delayed motor development and hearing loss, than their non-hypotensive counterparts. However, despite the significant consequences of hypotension, even the definition of hypotension in extremely low birth weight infants (ELBWIs) is controversial.1 In addition, the guidelines for the treatment of hypotension have not clearly been defined and are still somewhat arbitrary.7 In one study, hypotension was defined as a mean arterial pressure (MAP) <30 mm Hg,4 while hypotension in another study, was defined as <10th percentile of MAP for birth weight and postnatal age based on published normative data.8 In practice, an infant with a MAP less than his/her gestational age (GA) in weeks is generally accepted to have hypotension. Treatment regimens for early hypotension for ELBWI infants depend on the neonatal intensive care units (NICU) in which they are treated.4 Intervention rates vary from 29-98% and include volume expansion, inotropic support and corticosteroids.9 Al-Aweel, et al.10 reported that some units used vasopressors 5- to 30-fold more frequently than other units. Dempsey, et al.7 advocated the concept of permissive hypotension to treat hypotension in ELBWIs. Preterm infants with a mean arterial blood pressure lower than their number of gestational weeks often have no clinical signs of shock, presumably have adequate tissue oxygen delivery, and may therefore not need treatment. This approach to manage hypotension in ELBWIs involves the overall assessment of perfusion signs (skin color, capillary refill rate, urine output, blood lactate level, and acidosis), not just an assessment of numerical blood pressure.9 However, only a handful of studies have investigated permissive hypotension management of ELBWIs. We have used permissive hypotension to manage hypotensive ELBWIs in the Samsung Medical Center NICU for the past 7 years. Therefore, we designed the present study to investigate blood pressure trends during the initial 72 hours from birth and to compare the mortality and morbidities among ELBWIs within permissive hypotension, treated hypotension or normotension.
We retrospectively reviewed the medical records of ELBWIs, weighing less than 1000 g, who were born at Samsung Medical Center between January 2004 and December 2008 and admitted to the neonatal intensive care unit. Patients were excluded if they had lethal congenital malformations. We grouped infants according to their lowest MAP level and management during the first 72 hours of life into 1) a normotension group (N group; MAP >gestational age), 2) a permissive hypotension group (P group; MAP <gestational age with signs of good perfusion and no intervention), and 3) a treated hypotension group (T group; MAP <gestational age and intervention including volume pushes, vasopressors or corticosteroids).
GA was defined as the time from the date of the last menstrual period to birth. Hypotension was defined as a blood pressure in mm Hg less than gestational age in weeks. We collected blood pressure (BP) data during the first 72 hours after birth at intervals of 6 hours and included the lowest blood pressure records, regardless of the interval during which they were taken. Peripheral blood pressure was measured using an oscillometric technique (M1866A, Philips Medical Systems, Inc., WA, USA) and invasive blood pressure was measured using a calibrated pressure transducer (42584, ICU Medical, Inc., UT, USA) connected to an umbilical arterial catheter, which was positioned between thoracic vertebrae 6 to 10 in the abdominal aorta. End organ perfusion status was assessed by skin color, capillary refill rate, urine output, blood lactate level, and acidosis.
We analyzed the following potentially confounding variables: gestational age, birth weight, gender, 1- and 5-minute Apgar scores, antenatal steroid use, mode of delivery, pregnancy-induced hypertension, pathologically confirmed chorioamnionitis, small for gestational age (SGA),11 and respiratory distress syndrome (RDS). SGA was defined as a birth weight less than ten percentile. RDS was defined as respiratory difficutly requiring surfactant and mechanical ventilation with endotracheal intubation. In addition, we evaluated the following outcome measures: death before discharge, bronchopulmonary dysplasia (≥moderate, need for oxygen or positive pressure support at 36 weeks postmenstrual age),12 IVH (≥grade 3),13 periventricular leukomalacia, necrotizing enterocolitis (≥Bell's stage 2b),14 and retinopathy of prematurity15 requiring laser treatment.
Long-term, 2-year outcomes including hearing impairment and cerebral palsy were investigated. Cerebral palsy, as diagnosed by a pediatric rehabilitation specialist or a pediatric neurologist, was defined as a non-progressive neurological disorder characterized by an inability to control posture and movement and abnormal tone in the limbs.16 Hearing impairment was defined as the need for a hearing aid as recommended by an otolaryngologist. Finally, the Bayley Scales of Infant Development-II17 mental development index (MDI) and psychomotor development index (PDI) at a corrected age of 18 months were assessed.
The software package SPSS version 17 was used for all statistical analyses. ANOVA was used for continuous variables with normal distributions. To compare nominal variables such as mortality and morbidity, chi-square tests with binary logistic regression analysis were performed. Data are expressed as mean+SEM; and p-values less than 0.05 were considered significant.
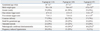
During the 4-year study period, 261 infants were born and admitted to the Samsung Medical Center NICU. Seven died within 72 hours of birth and had incomplete blood pressure data. We evaluated a total of 261 ELBWIs: 110 (42%) in the N group, 104 (40%) in the P group, and 47 (18%) in the T group. Table 1 lists the subjects' demographic characteristics. Birth weight was significantly lower in the T group than the other two groups. The 1-minute and 5-minute Apgar scores were significantly lower in the T group than the other two groups. The incidence of pathologically confirmed chorioamnionitis was significantly higher in the N group than the P and T groups, and higher in the P group than the T group.
Invasive blood pressure monitoring was performed in 56% (62/110) infants in the N group, 54% (56/104) infants in the P group, and 77% (36/47) infants in the T group. The T group depicted significantly higher rate of invasive BP monitoring (p-value: 0.02). The trend in mean blood pressures for all ELBWIs is shown in Fig. 1, while the trends in mean blood pressures of the N/P/T groups during the initial 72 hours of life are shown in Fig. 2. A spontaneous increase in mean arterial blood pressure was observed in the N and P groups, with a statistically significant difference in MAP between the N and P groups at every time point. In the T group, hypotension developed usually and was treated within 12 hrs from birth. Although the T group received treatment, infants in this group had a consistently lower mean blood pressure than infants in the N and P groups after 12 hours from birth. Infants with hypotension received treatment because of pneumothorax, severe pulmonary hypertension, or their cardiopulmonary resuscitation status. In T group infants, 87% (41/47) received volume expansion treatment (10 mL/kg of normal saline or bivon), 60% (28/47) dopamine, 30% (14/47) dobutamine, and 25% (12/4) intermittent epinephrine injections.
The mortality rate and the incidence of moderate to severe bronchopulmonary dysplasia (BPD) were significantly higher in the T group than the other two groups even after adjusting for birth weight, Apgar score, and pathologically confirmed chorioamnionitis (Table 2 and 3). The incidence of severe IVH (≥grade 3) was the highest in the T group compared to the other two groups, and higher in the P group than the N group. In multivariate analyses, adjusted for confounding factors including birth weight, Apgar scores and pathologically confirmed chorioamnionitis, there was no significant difference in IVH rate between the N and P groups, but the rate of IVH in the T group was significantly higher than the other two groups.
Even though the severe IVH rate in the P group was not significant after multivariate analysis, severe IVH was seen in more infants in the P group than in the N group. The gestational ages of 90% (18/20) of infants with severe IVH ranged from 23 to 26 weeks. To compare trends in the blood pressures of infants with and without severe IVH, the P group was divided into two subgroups: an IVH group and a non-IVH group. The data were analyzed according to gestaional week to account for the potentially confounding effect of number of gestational weeks. The IVH subgroup of infants showed a blood pressure trend similar to that of the non-IVH subgroup for gestational weeks 23-26 within 72 hours of birth (Fig. 2).
A total of 97/110 (88%), 87/104 (84%), and 23/47 (49%) ELBWIs from the N, P, and T groups, respectively, were discharged successfully. Of these, 89 (92%), 83 (95%), and 20 (87%) were followed-up for 2 years, and Bayley testing was performed in 28 (29%), 33 (38%), and 8 (17%) patients from the N, P, and T groups, respectively. There was no significant differences between groups N and P in incidence of cerebral palsy, hearing loss, or developmental delay, defined as Bayley score MDI or PDI <75 (Table 4). None of the infants developed blindness. Due to substantial proportion of missing data and follow-up loss, the long-term neurological outcomes of group T were not analyzed.
In this retrospective study, we characterized blood pressure trends during the initial 72 hours from birth and compared the mortality and morbidities between normotensive and permissive hypotension infants. The mortality rate and incidence of severe IVH and moderate to severe BPD were higher in treated hypotension infants than in permissive hypotension or normotensive infants. There were no differences in mortality or morbidities, including neurodevelopment outcomes, between normotensive and permissive hypotension infants. The results of this study support the proposal that a permissive hypotension approach does not result in poor outcomes.
Dempsey, et al.7 reported that careful observation without intervention in ELBWIs with hypotension (defined as BP<GA) and good perfusion signs resulted in outcomes as good as those of normotensive infants. In this earlier report, the most important factor informing the decision whether or not to treat hypotension was clinical assessment of end organ perfusion. By careful observation of peripheral perfusion, Dempsey, et al. were able to reduce the number of infants who received intervention. Although they reported only short-term outcomes, we herein evaluated long-term outcomes, as assessed by the 18 month corrected age Bayley DMI and DPI scores, cerebral palsy, and hearing abnormalities. Consistent with the previous short-term study, we found that the long-term outcomes of permissive hypotension infants were as good as those of normotensive infants.
The brain of preterm infants is known to be quite vulnerable to hypoperfusion of cerebral blood flow.3 Several studies reported that hypotension infants who received dopamine showed increased cerebral blood flow with increased blood pressure.18,19 Dopamine is regarded as the first choice and the most commonly used inotropic agent in hypotension of premature infants. The hypotension in ELBWIs might be related with myocardial dysfunction induced by umbilical cord clamping, therefore, the removal of placenta increases systemic vascular resistance. In such cases, dobutamine may be more helpful by decreasing afterload and improving cardiac contractility. However, vasopressor administration may induce sudden increase of blood pressure which is uncontrollable and possibly related with IVH or periventricular white matter injury.20 Fanaroff, et al.6 suggested that hearing and delayed motor development are related to treatment of symptomatic hypotension,21 and another study suggested that anti-hypotensive treatment is related to IVH, periventricular leukomalacia and major developmental impairments. Dopamine possibly induces worse outcomes than hypotension itself by rapidly changing cerebral hemodynamics.1,22
In these earlier studies, however, no clear therapeutic criteria or treatment protocols for hypotension treatment were used, thus making it hard to determine whether the treated hypotension was symptomatic or not and whether these adverse outcomes resulted from symptomatic hypotension itself or the side-effects of treatments such as fluid replacement and vasopressor agents.
Pellicer, et al.20 therefore performed a cohort case-control study to determine the impacts of hypotension treatment on morbidity and neurodevelopmental outcomes in low birth weight infants, however, found no differences in the rates of neurodevelopmental outcomes. These authors suggested that cautious use of cardiotonics in early systemic hypotension appears to be safe. However, Pellicer, et al. defined hypotension based on numerical blood pressure value alone without considering organ perfusion or overall clinical condition, therefore, they might have included healthy infants with transient hypotension in their analyses who were treated for hypotension.
At the Samsung Medical Center NICU, hypotension in infants is managed only when infants exhibit hemodynamically unstable status including unstable vital signs, and impaired perfusion signs such as delayed capillary refill, lack of a pinkish skin color, or decreased urine output. Non-symptomatic hypotension infants are treated by using a permissive hypotension approach. We found in the present study that treatment of hypotension in ELBWIs was related to IVH, BPD and mortality. However, the treated hypotension infants were relatively more immature, and thus more likely to require intervention for hypotension. Although birth weight, Apgar score and pathologically confirmed chorioamnionitis were adjusted in comparison of morbidities and mortality, it was difficult to ascertain that worse outcomes in the T group were not related with their higher vulnerability.
Nonetheless, infants in the P group in the present study could avoid unnecessary treatment for hypotension, and the P group showed as good outcomes as the N group.
Limitations of this study include the fact that it was a retrospective study, and 18 (38%) of 47 treated hypotension patients did not survive more than 7 days because of severe illness. Furthermore, only 69 (26%) of 261 infants were evaluated using Bayley tests, therefore, larger data would be needed for more reliable and constant conclusion.
In the present study, invasive BP monitoring rate was significantly higher in the T group, and this result could be related to the fact that the T group consisted of smaller babies who need central lines including umbilical arterial line more than others. However, between the N and P groups, no significant difference was observed in the ratio of invasive to non-invasive BP measuring method, indicating that this factor hardly affects the BP level and outcomes, at least between N group and P group.
In summary, a numerical blood pressure value lower than gestational age should not be used as the only indicator for treating early period hypotension in ELBWIs. Unnecessary treatment can be avoided by careful monitoring of ELBWIs with hypotension but good perfusion signs, and these infants have outcomes as good as those of normotensive infants. In contrast, hypotensive infants who showed unstable vital signs and received supportive treatment had higher mortality rate, and greater incidence of severe IVH (≥stage 3) and BPD (≥moderate) than normotensive and permissive hypotension infants.
Figures and Tables
Fig. 1
Mean blood pressures of all infants (A) and infants in each of the three groups (B) during the first 72 hours of life. Data are expressed as mean±SD (A), mean±SEM (B). *p<0.05 versus N, †p<0.05 versus P. SD, standard deviation; SEM, standard error of the mean.
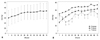
Fig. 2
Blood pressure trends of ELBWIs in the P group with and without severe intraventricular hemorrhage (≥grade 3) at gestational weeks 23-26. IVH, intraventricular hemorrhage; ELBWIs, extremely low birth weight infants.
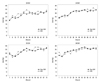
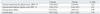
Table 3
Odds Ratios for Mortality and Major Morbidities after Adjusting Birth Weight, Apgar Scores and Pathologically Confirmed Chorioamnionitis
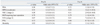
N, normotensive group; P, permissive hypotension group; T, treated hypotension group; PDA, patent ductus arteriosus; BPD, bronchopulmonary dysplasia; NEC, necrotizing enterocolitis; ROP, retinopathy of prematurity; IVH, intraventricular hemorrhage; PVL, periventricular leukomalacia.
*p<0.05 versus N.
†p<0.05 versus P.
References
1. Barrington KJ, Dempsey EM. Cardiovascular support in the preterm: treatments in search of indications. J Pediatr. 2006. 148:289–291.

2. Gill AB, Weindling AM. Randomised controlled trial of plasma protein fraction versus dopamine in hypotensive very low birthweight infants. Arch Dis Child. 1993. 69:284–287.

3. Seri I, Evans J. Controversies in the diagnosis and management of hypotension in the newborn infant. Curr Opin Pediatr. 2001. 13:116–123.

4. De Zegher F, Van Den Berghe G, Devlieger H, Eggermont E, Veldhuis JD. Dopamine inhibits growth hormone and prolactin secretion in the human newborn. Pediatr Res. 1993. 34:642–645.

5. Dempsey EM, Barrington KJ. Treating hypotension in the preterm infant: when and with what: a critical and systematic review. J Perinatol. 2007. 27:469–478.

6. Fanaroff JM, Wilson-Costello DE, Newman NS, Montpetite MM, Fanaroff AA. Treated hypotension is associated with neonatal morbidity and hearing loss in extremely low birth weight infants. Pediatrics. 2006. 117:1131–1135.

7. Dempsey EM, Al Hazzani F, Barrington KJ. Permissive hypotension in the extremely low birthweight infant with signs of good perfusion. Arch Dis Child Fetal Neonatal Ed. 2009. 94:F241–F244.

8. Bada HS, Korones SB, Perry EH, Arheart KL, Ray JD, Pourcyrous M, et al. Mean arterial blood pressure changes in premature infants and those at risk for intraventricular hemorrhage. J Pediatr. 1990. 117:607–614.

9. Laughon M, Bose C, Allred E, O'Shea TM, Van Marter LJ, Bednarek F, et al. Factors associated with treatment for hypotension in extremely low gestational age newborns during the first postnatal week. Pediatrics. 2007. 119:273–280.

10. Al-Aweel I, Pursley DM, Rubin LP, Shah B, Weisberger S, Richardson DK. Variations in prevalence of hypotension, hypertension, and vasopressor use in NICUs. J Perinatol. 2001. 21:272–278.

11. Lubchenco LO, Hansman C, Boyd E. Intrauterine growth in length and head circumference as estimated from live births at gestational ages from 26 to 42 weeks. Pediatrics. 1966. 37:403–408.

12. Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA, et al. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics. 2005. 116:1353–1360.

13. Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978. 92:529–534.

14. Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978. 187:1–7.
15. The Committee for the Classification of Retinopathy of Prematurity. An international classification of retinopathy of prematurity. Arch Ophthalmol. 1984. 102:1130–1134.
16. Stoll BJ, Hansen NI, Adams-Chapman I, Fanaroff AA, Hintz SR, Vohr B, et al. Neurodevelopmental and growth impairment among extremely low-birth-weight infants with neonatal infection. JAMA. 2004. 292:2357–2365.

17. Leonard CH, Piecuch RE, Cooper BA. Use of the Bayley Infant Neurodevelopmental Screener with low birth weight infants. J Pediatr Psychol. 2001. 26:33–40.

18. Pellicer A, Valverde E, Elorza MD, Madero R, Gayá F, Quero J, et al. Cardiovascular support for low birth weight infants and cerebral hemodynamics: a randomized, blinded, clinical trial. Pediatrics. 2005. 115:1501–1512.

19. Munro MJ, Walker AM, Barfield CP. Hypotensive extremely low birth weight infants have reduced cerebral blood flow. Pediatrics. 2004. 114:1591–1596.

20. Pellicer A, Bravo MC, Madero R, Salas S, Quero J, Cabañas F. Early systemic hypotension and vasopressor support in low birth weight infants: impact on neurodevelopment. Pediatrics. 2009. 123:1369–1376.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download