Abstract
Purpose
A retrospective investigation of the clinical and radiologic features as well as the bronchoscopic appearance was carried out in patients with endobronchial aspergilloma.
Materials and Methods
Ten patients with endobronchial aspergilloma diagnosed by bronchoscopy and histological examination were identified at the Gyeongsang University Hospital of Korea, from May 2003 to May 2009.
Results
The patients included 9 men and 1 woman, and the age of the patients ranged from 36 to 76 (median, 58 years). The associated diseases or conditions were: previous pulmonary tuberculosis in 7 patients, lung cancer in 2 patients, pulmonary resection in 1 patient, and foreign body of the bronchus in 1 patient. The chest radiologic finding showed fibrotic changes as a consequence of previous tuberculosis infection in 6 patients and a mass-like lesion in 2 patients. Two patients had a co-existing fungus ball, and an endobronchial lesion was suspected in only 2 patients on the CT scan. The bronchoscopic appearance was a whitish to yellow necrotic mass causing bronchial obstruction in 7 patients, foreign body with adjacent granulation tissue and whitish necrotic tissue in 1 patient, whitish necrotic tissue at an anastomosis site in 1 patient, and a protruding mass with whitish necrotic tissue in 1 patient.
Aspergillus spp. is a ubiquitous fungus and responsible for a broad spectrum of lung disease, depending on the patient's immune status and underlying lung disease. Pulmonary involvement of aspergillosis is usually classified with a pulmonary aspergilloma, allergic bronchopulmonary aspergillosis, chronic necrotizing pulmonary aspergillosis, and invasive aspergillosis.1-4 In patients with a preexisting lung cavity from a variety of causes, such as pulmonary tuberculosis, sarcoidosis, or pneumoconiosis, aspergillus can colonize and grow into the cavity to form a pulmonary aspergilloma (fungus ball). Allergic bronchopulmonary aspergillosis (ABPA) is a hypersensitivity reaction related to the presence of Aspergillus antigens that mainly affect patients with asthma. While invasive aspergillosis is a severe and fatal disease that is primarily observed in severely immunocompromised patients, chronic necrotizing pulmonary aspergillosis (CPNA) is characterized by a local invasion into the lung tissue in patients with chronic lung disease and associated with diabetes mellitus, corticosteroid therapy and malnutrition. An endobronchial aspergilloma is an unusual presentation of pulmonary aspergillosis; it is characterized by growth of the Aspergillus species into the bronchial lumen.
Among patients who had undergone bronchoscopy and histological examination at Gyeongsang University Hospital from May 2003 to December 2009, the medical records of those diagnosed with endobronchal aspergilloma were reviewed. The diagnosis of endobronchial aspergilloma was made primarily based on the presence of an intraluminal mass or necrotic tissue on bronchoscopy and septated fungal hyphae with acute branching angles, characteristic of aspergillus species, on histological examination. Cases with no visible endobronchial lesions on bronchoscopy and patients diagnosed by transbronchial lung biopsy were excluded. The clinical and radiological features as well as bronchoscopic appearance were retrospectively investigated in patients with endobronchial aspergilloma.
Ten patients with endobronchial aspergilloma were identified.Table 1 summarized the clinical characteristics of the patients. There were nine men and one woman, and the age of the patients ranged from 36 to 76 (median, 58 years). Seven patients had a history of pulmonary tuberculosis. One patient had been diagnosed with pulmonary tuberculosis at a local public health center, just two months before presenting to this hospital. Six patients had been diagnosed with pulmonary tuberculosis several years ago, ranging from 6 to 30 years previously. Two patients had lung cancer and one patient underwent lobectomy for lung cancer. One patient had a suspected foreign body in the right main bronchus. Five patients had non-pulmonary comorbid illness: dilated cardiomyopathy, essential thrombocytosis, cerebrovascular accident, and hypertension. None of the patients were in an immunocompromised state or had atopy. Seven patients were current or ex-smokers. The findings of cough, sputum and dyspnea on exertion were the most common complaints, and hemoptysis was observed in five patients. Microbiologic studies of bronchial washing fluid were performed in seven patients, and revealed no M. tuberculosis in all patients, however, aspergillus species was isolated in one patient. Two patients were treated with anti-fungal agent. One patient received itraconazole via intravenous route for 2 weeks and switched to oral for 2 weeks, and one patient took oral itraconazole for 3 weeks.
The radiographic and bronchoscopic findings are shown in Table 2. The chest radiographic findings were abnormal in nine patients. The abnormal radiographic findings were fibrotic changes with some degree of volume loss as a consequence of previous tuberculosis infection in six patients, and a mass-like lesion in two patients. One patient showed volume loss of the right upper lobe due to lobectomy, and one patient had no abnormal findings of the lung parenchyma. The CT findings showed a mass with a multi-lobulated contour in two patients (patient 1, 3) (Fig. 1) and the two patients had a co-existing fungus ball (patient 6, 8) and an endobronchial lesion, such as a foreign body or broncholithiasis, was suspected in two patients (patient 2, 9) (Fig. 2). Multiple calcified nodules and fibrotic changes as a sequelae of previous pulmonary tuberculosis was noted in six patients (patient 4-9) (Fig. 3)
The bronchoscopic findings showed a whitish to yellow necrotic mass in the bronchus causing obstruction of the lobar or segmental bronchus in seven patients (Fig. 1), a foreign body with adjacent granulation tissue covered with whitish necrotic tissue in one patient (patient 2) (Fig. 2), granulation tissue with whitish necrotic tissue at an anastomosis site in one patient (patient 3) (Fig. 2), and a protruding mass with whitish necrotic tissue in one patient (patient 10). The abnormalities on bronchoscopy were confined to the left upper lung zone in seven patients, left lower lung zone in one patient, and right lung in two patients. The median number of specimens by bronchoscopic biopsy was three pieces, ranging from one to six.
Endobronchial aspergilloma is a rare disease entity with pulmonary involvement of aspergillosis. Its definition is not well described in the literature and is not usually classified with other pulmonary aspergillosis.1,3 However, endobronchial aspergilloma can usually be defined as a non-invasive form of aspergillosis characterized by massive intrabronchial overgrowth of the aspergillus species, mainly aspergillus fumigates, and it may be considered an unusual form of a fungus ball, found inside of the bronchus with or without a parenchymal lesion and/or cavity. One of rare presentation of pulmonary apsergillosis, pseudomembranous necrotizing tracheobronchial aspergillosis, which is usually limited to the trachea and main bronchus, is an uncommon form of invasive aspergillosis that mainly affects immunocompromised patients.1,21
In our study, endobronchial aspergilloma was incidentally detected during bronchoscopy. Only two patients (patient 2, 9) had suspicious endobronchial lesions on their CT scans. The other patients underwent bronchoscopy to evaluate the cause of hemoptysis and to diagnose parenchymal lung lesions. Most patients were incidentally diagnosed during bronchoscopy, and the aspergillus was confirmed by histological examination. Endobronchial aspergilloma can present either as the sole manifestation of pulmonary aspergillosis or can be found with other forms of pulmonary aspergillosis. CNPA or ABPA may be associated with endobronchial aspergilloma14 and pulmonary aspergilloma inside of the lung cavity can be visualized by bronchoscopy.16 In our study, two patients had a fungus ball inside of a cavity on the CT scan, and we considered that these patients had endobronchial aspergilloma with co-exististing fungus ball.
In immunocompetent patients, aspergillosis requires a nidus or structural changes that induce airflow stasis to colonize the bronchial lumen. In the present study, most patients had a history of pulmonary tuberculosis, and their chest X-ray showed destructive and fibrotic changes of the parenchyma that resulted in airway narrowing and obstruction. Such changes may induce airflow stasis and can be the focus of colonization by aspergillosis. Review of the medical literature showed that the majority of patients had a wide range of parenchymal changes caused by previous pulmonary infections.5,10,12,16,18,20 Four patients without underlying lung disease in our study had an endobronchial lesion similar to a foreign body, lung cancer or granulation tissue of the anastomosis site after pulmonary resection. These endobronchial lesions may act as a nidus for colonization of aspergillus.
When lung cancer is associated with aspergillosis colonization, it may often be confused with a simple endobronchial aspergilloma. There was a case of lung cancer masked by endobronchial aspergilloma in our study.9 The patient underwent bronchoscopy to evaluate a lung mass, and fungal hyphae were observed on histological examination. The patient was treated with itraconazole for a month with the diagnosis of endobronchial aspergilloma. However, the lung mass gradually increased despite treatment, and the diagnosis of lung cancer was finally confirmed by transthoracic needle biopsy. A few cases of endobronchial aspergillosis associated with tumors have been reported in the literature.17,22,23
Although aspergillosis of the bronchial stump site is very rare, it can occur after pulmonary resection; the suture material can act as a nidus for the aspergillus infection.15 In the literature, bronchial stump aspergillosis occurs usually 6 to 12 months after a resection and is more common with silk than with nylon sutures.11 However, in a case of this study (patient 3), it occurred unusually with nylon sutures one month after surgery.
In the present study, five patients reported hemoptysis at the time of admission, and two of these patients had a ground glass appearance on their CT scan, which indicated recent bleeding from the respiratory tract. Although hemoptysis may result from underlying lung disease or a co-existing fungus ball, endobronchial aspergilloma might have been the cause of hemoptysis in these patients.
Optimal treatment of endobronchial aspergilloma has not yet been established, because endobronchial apsergilloma may be a simple colonization of airway lumen of aspergillus species in immunocompetent host, and specific treatment was not done in most of the patients. In pulmonary aspergilloma, anti-fungal agent has usually no benefit, and surgical resection may be considered as an alternative treatment strategy in patients with a favorable pulmonary reserve.24,25 In the present study, only two patients were treated for endobronchial aspergilloma with itaconazole for about a month, and one patient was the first case of pathologically confirmed endobronchial aspergilloma. At first, we considered as an invasive form of pulmonary aspergillosis-like chronic necrotizing pulmonary aspergillosis. However, the lesion was not improved after one month of itraconazole treatment. Therefore, we thought that the lesion was a simple colonization of asperillus species. The other patient was observed for a certain period without any treatment. One patient underwent bronchoscopy one and half years after an endobronchial aspergilloma, and was diagnosed without any treatment. There was no significant change of the bronchoscopic appearance reported.
In conclusion, endobronchial aspergilloma is usually incidentally detected in patients with underlying lung disease and also in immunocompetent patients. It appears as a necrotic mass causing bronchial obstruction on bronchoscopy, and can be confirmed by biopsy.
Figures and Tables
Fig. 1
Patient 1 (A) Chest radiograph of a 75-year-old man shows a large mass like shadow in the left upper lobe. (B) The CT scan shows a non-enhanced mass with a multi-lobulated contour in the left upper lobe. (C) The bronchoscopy shows a protruding whitish mass in the upper bronchus of the left upper lobe. (D) The histologic examination shows numerous hyphae with background necrotic debris (H&E, ×100). H&E, hematoxylin and eosin.
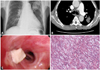
Fig. 2
Patient 2 (A) The CT scan shows a small high density lesion in the right bronchus intermedius (arrow). (B) The bronchoscopy shows a foreign body-like lesion covered with whitish necrotic material. Patient 3 (C) The bronchoscopy shows granulation tissue with whitish material at the stump site. (D) Histopathologic examination revealed abundant necrotic material with multiple mycelia consisting of septate hyphae branching at an angle of approximately 45°, characteristic of aspergillus species (H&E, ×100). H&E, hematoxylin and eosin.
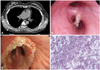
Fig. 3
Patient 6 (A) Chest radiograph of a 46-year-old man shows multiple calcified nodule and fibrotic changes with volume loss in the both lung zones. (B) The CT scan shows a suspicious fungus ball in the left upper lobe. (C) The bronchoscopy shows a whitish mass lesion causing obstruction of the apical segment of the left upper lobe.

References
1. Soubani AO, Chandrasekar PH. The clinical spectrum of pulmonary aspergillosis. Chest. 2002. 121:1988–1999.

3. Franquet T, Müller NL, Giménez A, Guembe P, de La Torre J, Bagué S. Spectrum of pulmonary aspergillosis: histologic, clinical, and radiologic findings. Radiographics. 2001. 21:825–837.

4. Klein DL, Gamsu G. Thoracic manifestations of aspergillosis. AJR Am J Roentgenol. 1980. 134:543–552.

5. Kim JS, Rhee Y, Kang SM, Ko WK, Kim YS, Lee JG, et al. A case of endobronchial aspergilloma. Yonsei Med J. 2000. 41:422–425.

6. Park BJ, Kim YK, Kim H, Kim YH, Lee HI, Kang HM, et al. A case of endobronchial aspergillosis completely obstructing lobar bronchus. Tuberc Respir Dis. 2005. 59:311–314.

7. Kim TH, Yong BJ, Kim YK, Lee YM, Kim KU, Uh ST, et al. A case of endobronchial aspergilloma with massive hemoptysis. Tuberc Respir Dis. 2004. 57:589–593.

8. Kim SJ, Lee EJ, Lee TH, Yoo KH, Lee KY. A case of endobronchial aspergilloma. Tuberc Respir Dis. 2006. 61:60–64.

9. Ham HS, Lee SJ, Cho YJ, Jeon KN, Jeong YY, Kim HC, et al. A case of lung cancer obscured by endobronchial aspergilloma. Tuberc Respir Dis. 2006. 61:157–161.

10. Eom WY, Kim NI, Kim SW, Lee BH, Kim SH, Ahn YS, et al. A case of endobronchial aspergilloma in patient with collapse of right middle lobe. Korean J Med. 2006. 70:221–225.
11. Sawasaki H, Horie K, Yamada M, Tajima G, Katsura S, Naito Y, et al. Bronchial stump aspergillosis. Experimental and clinical study. J Thorac Cardiovasc Surg. 1969. 58:198–208.
12. Dar KA, Shah NN, Bhargava R, Ahmed Z, Pandey DK, Dar NH, et al. Endobronchial aspergilloma in a 30-year-old man. J Bronchol. 2007. 14:207–209.

13. Noppen M, Claes I, Maillet B, Meysman M, Monsieur I, Vincken W. Three cases of bronchial stump aspergillosis: unusual clinical presentations and beneficial effect of oral itraconazole. Eur Respir J. 1995. 8:477–480.

14. Dobbertin I, Friedel G, Jaki R, Michl M, Kimmich M, Hofmann A, et al. [Bronchial aspergillosis]. Pneumologie. 2010. 64:171–183.
15. Le Rochais JP, Icard P, Simon T, Poirier P, Evrard C. Bronchial stump aspergillosis. Ann Thorac Surg. 2000. 70:302–304.

16. Smith RL, Morelli MJ, Aranda CP. Pulmonary aspergilloma diagnosed by fiberoptic bronchoscopy. Chest. 1987. 92:948–949.

17. Yoshitomi A, Kuwata H, Suzuki T, Narushima M, Nakajima T, Yogo Y, et al. [Lung cancer obscured by aspergillus hyphae]. Nihon Kokyuki Gakkai Zasshi. 2000. 38:321–324.
18. Shameem M, Bhargava R, Ahmad Z, Fatima N, Malik A. Endobronchial aspergilloma - Presenting as solitary pulmonary nodule. Respir Med CME. 2010. 3:111–112.

20. Qureshi MA, Nair VS. Pulmonary aspergilloma: Bronchoscopic appearance. J Bronchol. 2003. 10:204–206.
21. Pervez NK, Kleinerman J, Kattan M, Freed JA, Harris MB, Rosen MJ, et al. Pseudomembranous necrotizing bronchial aspergillosis. A variant of invasive aspergillosis in a patient with hemophilia and acquired immune deficiency syndrome. Am Rev Respir Dis. 1985. 131:961–963.
22. Quoix E, Gasser B, Apprill M, Gourdon C, Pauli G, Roegel E. [Endobronchial aspergillosis associated with a carcinoid tumor]. Rev Mal Respir. 1990. 7:609–612.
23. Yoshitomi A, Terada S, Fujita H, Miura T, Imokawa S, Chida K. [Aspergillosis with non-cavitary lung cancer]. Kansenshogaku Zasshi. 2000. 74:536–540.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download