Abstract
Dermatomyositis (DM) is an autoimmune disorder with idiopathic myopathy and characteristic skin manifestations that one often accompanied by an internal malignancy. The association between dermatomyositis and malignancy has been reported several times, although tonsillar carcinoma is extremely rare not only in far eastern populations but also in caucasian populations. We report two cases of Korean patients with dermatomyositis associated with tonsillar carcinoma.
Dermatomyositis (DM) is an idiopathic inflammatory myopathy with characteristic cutaneous manifestations, such as erythematous papules on the dorsal surface of the phalangeal joints (Gottron's sign), edematous erythema of the eyelids (heliotrope erythema), and a violaceous, erythematous rash on the trunk.1 Malignancy may occur before the onset of myositis, concurrently or afterwards. The most commonly observed cancers in female patients with DM are breast and gynecologic cancers, whereas the most commonly observed cancer in male patients with DM is lung cancer. The most commonly observed cancer shared by both genders is gastrointestinal cancer.1 The risk of malignancy in DM patients increases for 3-5 years after the onset of DM and then decreases to near baseline, and a true link with cancer does exist.2 Worldwide, only one case of tonsillar cancer associated with DM has been reported in Italy.3 We report two cases of Korean patients with DM and tonsillar squamous cell carcinoma.
A 61-year-old woman born in South Korea was referred to the Department of Otorhinolaryngology-Head and Neck Surgery on December 2005 because of a sore throat and left cervical lymphadenopathy that was first noticed by the patient in September 2005.
The patient was diagnosed with DM in September 2004 and was subsequently followed by a rheumatologist. She was noted to have a heliotrope rash on the eyelids and a red, violaceous, non-pruritic skin rash on her trunk, and symmetrical proximal muscle weakness. The clinical features of DM were supported by several laboratory tests. The patient had elevated muscle enzymes as demonstrated by increased CK (1609 U/L), serum myoglobin (548 ng/mL), LDH (485 U/L), ESR (45 mm/h), and C-reactive protein (1.6 mg/dL). Antinuclear antibodies (ANA) were positive at a lower titer (1 : 160) in Hep-2 cells with a "speckled" morphology on indirect immunofluorescence. Based on the above data, this patient was diagnosed with probable DM. Initially, oral treatment with prednisolone and azathioprine was carried out. The oral prednisolone was tapered off when remission occurred.
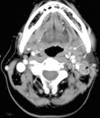
On the initial visit to our department in December 2005, pharyngeal endoscopy demonstrated a vegetation on the left palatine tonsil. A surgical biopsy revealed that the lesion was squamous cell carcinoma. A non-tender, hard, and non-movable mass was palpated in the left neck. A neck CT with enhancement revealed multiple pathologic lymph nodes in the left upper internal jugular chain (level II) and a primary lesion on the left palatine tonsil (Fig. 1). The preoperative cancer evaluation included a neck MRI, a bone scan, gastroscopy, an abdominal sonogram, and a chest X-ray. The tumor status was reported as stage IVa, cT1N2bM0.
The patient underwent three courses of neoadjuvant chemotherapy with cisplatin and 5-fluorouracil with a good response. One month after the end of this treatment, surgical treatment with wide excision of the left tonsil cancer via a midline mandibulotomy approach with an ipsilateral modified radical neck dissection was performed. Histology of the surgical specimens from the neck dissection and primary lesion showed squamous cell carcinoma. The patient received concurrent chemoradiotherapy (CCRT); the oral prednisolone and azathioprine had been discontinued. Her muscle enzyme levels were normalized 6 months after the surgical treatment. However, multiple pulmonary metastatic lesions were found on PET CT in March 2007 and she died of pulmonary edema and an embolism in August 2007.
A 64-year-old man born in South Korea was referred to the Department of Otorhinolaryngology-Head and Neck Surgery in March 2007 because of a right neck mass. The mass was diagnosed as a carcinoma by fine needle aspiration cytology (FNAC). He was diagnosed with DM in August 2005 at the Department of Rheumatology. The characteristics of DM were supported by physical findings, such as heliotrope erythema, a Gottron's papule, symmetrical proximal muscle weakness, and several laboratory studies. The laboratory findings included elevated muscle enzymes, as demonstrated by increased CK (2606 U/L), serum myoglobin (608 ng/mL), LDH (612 U/L), and ESR (50 mm/h). ANA were positive at a lower titer (1 : 80) on Hep-2 cells with a "speckled" morphology on indirect immunofluorescence. Based on the above findings, this patient was diagnosed with probable DM. At follow-up, the DM was treated with steroids and an immunosuppressant agent at the Department of Rheumatology.
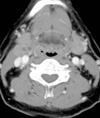
Physical examination demonstrated no primary origin for the malignancy. A non-tender, hard, and non-movable mass was palpated in the right neck (cervical lymph node level II). A neck CT with enhancement revealed a predominantly solid mass in the right parapharyngeal space at the level of the oropharynx (Fig. 2). An FNAC reported the presence of atypical cells. A PET CT was performed to identify the primary cancer site. 18F-fluorodeoxyglucose (18F-FDG) uptake was increased in the right palatine tonsil and right parapharyngeal space (max SUV of 4.4 and 1.4, respectively) (Fig. 3).
Panendoscopic biopsies were obtained at four suspicious primary sites (the hypopharynx, base of the tongue, tonsils, and nasopharynx). The primary site was shown to be the right palatine tonsil. The tumor status was reported as cT1N1M0. Surgical treatment with wide excision of the right tonsil cancer and right modified radical neck dissection was performed. The surgical biopsy revealed squamous cell carcinoma. His muscle enzyme levels were normalized 6 months after the surgical treatment. During subsequent 14 months of follow-up, no signs of malignancy recurred and the muscle enzyme levels were persistently normal.
DM should be considered an autoimmune disorder in which genetic and environmental factors, such as neoplastic antigens, seem to play a determinant pathogenic role in inducing dysregulation of the immune system.3,4
Although the temporal relationship between DM and malignancy remains unclear, coincidental observations have been found in all body areas. Ovarian, lung, and colorectal cancers have been diagnosed frequently both before and after the diagnosis of DM, suggesting that these are candidate cancers for association with the disease.4 The clinical manifestations of DM have been reported to improve after treatment of underlying cancer, however, the tumor prognosis is not affected by DM since the survival rate is similar to cases without DM.5 In addition, muscle weakness has been shown with relapses of the malignancy.6 Therefore, surveillance needs to be maintained because the risk of malignant disease remains high for many years after diagnosis. An evaluation for malignancy in patients with DM could potentially reduce mortality.
In the two cases presented in this paper, one patient died of metastatic disease of the lungs 17 months after surgery and CCRT while the other patient has survived for 14 months after surgery. The prognoses of the patients reported herein are similar to other reports,6 suggesting that survival rates are comparable to cases without DM. Thus, the progression of cancer does not appear to change with treatment of the DM.
In conclusion, from the viewpoint of otolaryngologists, careful examination of the upper airway and digestive tract is important for screening and detection of a malignancy in patients with DM, because survival can be prolonged and disability from myositis can be alleviated if cancers are treated early.
Figures and Tables
Fig. 1
Axial view of the neck CT with enhancement revealed multiple pathologic lymph nodes of the left upper internal jugular chain and cervical lymph node group II (black arrow) and a primary lesion of the left palatine tonsil (white arrow).
References
1. Hill CL, Zhang Y, Sigurgeirsson B, Pukkala E, Mellemkjaer L, Airio A, et al. Frequency of specific cancer types in dermatomyositis and polymyositis: a population-based study. Lancet. 2001. 357:96–100.

2. Airio A, Pukkala E, Isomäki H. Elevated cancer incidence in patients with dermatomyositis: a population based study. J Rheumatol. 1995. 22:1300–1303.
3. Botsios C, Ostuni P, Boscolo-Rizzo P, Da Mosto MC, Punzi L, Marchiori C. Dermatomyositis and malignancy of the pharynx in Caucasian patients: report of two observations. Rheumatol Int. 2003. 23:309–311.
5. Sugiyama T, Nakagawa T, Inui M, Tagawa T. Tongue carcinoma in a young patient with dermatomyositis: a case report and review of the literature. J Oral Maxillofac Surg. 2001. 59:925–928.

6. Kovacs SO, Kovacs SC. Dermatomyositis. J Am Acad Dermatol. 1998. 39:899–920.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download