Abstract
Purpose
We reviewed the results of cross finger flaps after surgical release and vigorous postoperative exercises for long-standing, severe flexion contractures of the Proximal Interphalangeal (PIP) joints of fingers.
Materials and Methods
In 9 patients, all contracted tissue was sequentially released and the resultant skin defect was covered with a cross-finger flap. The cause of the contracture was contact burn in 4, skin graft in 3, and a previous operation in 2. The mean follow-up period was 41.2 months.
Results
The mean flexion contracture/further flexion in the joints were improved from 73.4/87.8° to 8.4/95.4° at the last follow-up. A mean of 19.5° of extension was achieved with vigorous extension exercise after the operation. The mean gain in range of motion (ROM) was 79.4°. Near full ROM was achieved in 3 cases. There were no major complications.
Longstanding and severe flexion contractures of the proximal interphalangeal (PIP) joint of fingers significantly impair hand function. Several anatomical structures, including the skin, subcutaneous tissues, tendon sheath, flexor tendons, palmar plate, check rein ligament, and collateral ligaments, are shortened.1-3 If non-operative measures fail to stretch these contracted structures, surgical intervention is probably needed to restore hand function. However, it is quite challenging and the results are often discouraging, especially if the contracture is combined with scarring on the palmar side of the joint.
Various surgical techniques have been described with differing results for the treatment of flexion contractures of the PIP joints.2-15 These techniques can be assigned to 2 categories: open release or distraction histogenesis. With the open technique, the majority of studies have reported disappointing outcomes. Recently, some researchers have achieved satisfactory results with the use of gradual distraction using an external fixator to correct traumatic flexion contracture.10,11 However, they excluded patients with flexion contractures combined with scar tissue around the joints. To restore function in these patients, surgical release of all contracted tissue seems to be inevitable and the resultant skin defect should be covered with stable skin to prevent recurrence.
The purpose of this study was to evaluate the effect of cross finger flaps after extensive surgical release of contracted tissue and vigorous postoperative extension exercise in gain of extension for long standing, severe flexion contractures with palmar scarring of the fingers.
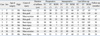
Between June 2002 and November 2007, 9 patients were operatively released and the resultant skin defects were covered with cross-finger flaps due to long standing (when duration of the contracture was more than 10 years), severe flexion contractures of the PIP joints. There were 5 men and 4 women, and the median age was 37.7 years (range, 23-59 years). The average interval between the initial injury and operation was 20.8 years (range, 11-50 years). The mean follow-up period was 41.2 months (range, 24-77 months). The middle finger was involved in 1 patient, the ring finger in 5, and the little finger in 3. The cause of contracture was contact burn in 4 patients, split-thickness skin grafts for palmar skin defects in 3, and excision of a tumor in 2. In 2 patients (cases 3 and 5), mild hypoplasia of the proximal phalangeal head was shown in plain radiographs of the fingers (Table 1).
After the excision of the scar tissue on the palmar side of the finger, the contracted soft tissues were released sequentially from the check rein ligaments and palmar plates to collateral ligaments in all of our patients (Fig. 1A and B). The shortening of the palmar plate and bilateral collateral ligaments were identified in all our patients. The proper collateral ligament was partially released. All of our patients also showed mild tightening of the flexor tendons. After the release, the PIP joints were forcefully stretched as much as possible to achieve joint extension, while circulation to the distal finger was not disturbed with this maneuver and the passive range of motion of the joint was recorded. Then, the PIP joint was fixed in maximal extension using transarticular fixation with a Kirschner wire. The resultant palmar skin defect was covered with a cross finger flap from a neighbor finger at the same time. The size of the flap was determined by adding 2 mm or more to the defect size. The donor site was covered with a splitthickness skin graft. The flap was divided 2 weeks postoperatively at the time of the removal of the Kirschner wire. Then, aggressive active and passive joint extension exercises were continued for 3 months after surgery (Fig. 2). Continuous active and passive range of motion (ROM) exercises were also emphasized for maintaining the angle of finger extension.
At the final follow-up, the residual flexion contractures and further flexion of the PIP joints in all patients were measured. Complications related to the surgery were also evaluated.
A Wilcoxon signed-rank test was performed to determine the significance in improvement of flexion contractures, further flexion, and ROM at the final follow-up, comparing with preoperative and intraoperative values. A p-value of ≤ 0.05 was considered significant.
The mean preoperative angle of flexion contractures and further flexion of the PIP joints was 73.4° (range, 55-95°) and 87.8° (range, 80-95°). After the excision of the scar tissue, shortening of the palmar plate and biliateral collateral ligament was identified in all our patients. After completion of the surgical release for the contracted joint, the mean angle of flexion contractures and further flexion of the PIP joints was 27.9° (range, 20-38°) and 93.0° (range, 87-98°). At the final follow-up, the mean angle of flexion contractures and further flexion in the joints was 8.4° (range, 0-23°) and 95.4° (range, 87-110°). The mean gain in the flexion extension arc was 79.4° (range, 58-105°) in comparison with preoperative range of motion and 22.7° (range, 3-47°) in comparison with intraperative range of motion. The mean improvement in flexion contractures showed a statistically significant difference when compared with preoperative and intraoperative values (p = 0.008) from a mean of 73.4° and 27.9° to 8.4°. Near full ROM was obtained in 3 cases (Fig. 1C and D). All patients were satisfied with the final results, although 2 patients had an extension lag of more than 10° (cases 1 and 3) (Table 1).
There were no major complications such as neurovascular injury, infection, or recurrence of contractures. Two patients had mild tingling sensations in their fingers, but they spontaneously disappeared. Partial skin necrosis was observed in 1 patient, which healed with no intervention at postoperative 5 weeks.
Several authors have described the results after surgical correction of disabling flexion contractures of the PIP joints of the fingers with variable rates of success. In 1976, Sprague13 reported 13° ROM gains of flexion contractures of the PIP joints after palmar capsular release. However, the ROM deteriorated and became less than that of the preoperative status at the last follow-up. In 1977, Harrison16 reported a 24° gain of ROM of flexion contractures with sequential capsular release while preserving the proper collateral ligaments of the PIP joints using a palmar incision. In 1979, Gould and Nicholson8 reported 12° to 13° improvements of motion of the joints after palmar capsulectomy, and suggested that more severe problems the patients had in the diagnosis, the less motion they gained at the last follow-up. In 2002, Ghidella, et al.6 reported only 5.8° of improvement with palmar release of the contracted tissue at a 2-year follow-up. Contrary to these unsatisfactory results, Brüser, et al.17 reported 30° and 50° of improvement of motion after surgical release with 2 different approaches, a palmar and a midlateral incision. They recommended the midlateral incision because of less soft tissue trauma than that of the palmar incision, which made early mobilization possible.
As the majority of studies have reported disappointing outcomes with the open technique, other authors have been concerned about distraction histogenesis in the treatment of chronic flexion contractures of the PIP joints.10,11,18 In 2002, Haushian, et al.11 reported a mean of 38° of improvement of motion with a mean ROM of 42° by dynamic extension correction technique using compass hinge external fixator. In 2004, Houshian and Schrøeder18 also reported good short-term results using a monolateral frame for distraction correction in 10 patients with chronic flexion contractures of the PIP joints. Houshian and Chikkamuniyappa10 reported an increase of the mean active ROM by 63° and the mean active extension by 47° after gradual distraction correction using an external fixator without serious complications. However, they excluded patients with contractures from burn or crushing in their study. Although the technique has satisfactory clinical outcomes, it has limitations in patients with severe flexion contractures of the PIP joints combined with scarring.
In our study, we selected patients with long standing (10 years or more), severe flexion contractures of the PIP joints combined with palmar scarring. In these patients, tethering by the scar tissue and contractures of the palmar plates and collageral ligaments were the main cause of contracture. In all of our patients, surgical release of contracted tissue was inevitable to get maximal extension of the joint during the operation. The resultant skin defect was covered by a cross-finger flap, which was slightly larger in size than that of the defect, from a neighboring finger to prevent contracture with time. By covering with stable and redundant skin, vigorous ROM exercises were possible just after healing of the operative wound. In the operation field, our patients showed a mean of 27.9° of flexion contracture after completion of the release. However, vigorous exercise improved the angle of flexion contracture to a mean of 8.4° at the last follow-up. With our technique and postoperative management, a mean of 79.4° of increase of motion was achieved in comparison with preoperative values. We believe that early vigorous exercises after covering the defect with stable skin is how we achieved our excellent clinical results. In 2005, Ulkür, et al.14 also reported a mean of 81.2° of improvement of motion in patients with severely contracted fingers with combined use of a cross-finger and side finger transposition flap after the resection of the scar tissue.
There are several limitations of this study. First, only ROM at the final follow-up was used to estimate the clinical results. Second, a small number of patients with mixed etiologies was included in this study, which means this procedure has been infrequently indicated. Third, it is a retrospective study. However, it could give some important information in the treatment of patients with chronic flexion contractures of the PIP joints of the finger. Contractures without severe scar tissue could be approached by palmar or midlateral incisions or gradually corrected by using distraction histogenesis with external fixator. However, open release of all contracted tissue followed by covering the resultant skin defect with cross-finger flap could be a reasonable option in patients with combined severe scar tissue of the finger.
Figures and Tables
Fig. 1
(A) A 51-year-old woman presented with a chronic, 90° fixed flexion contracture of the proximal interphalangeal joint of right fourth finger caused by a burn injury 50 years ago. (B) All contracted tissue was released sequentially and the resultant skin defect was covered with stable and redundant skin by a using cross-finger flap from the neighboring third finger. (C and D) A at 30-month follow-up, near full range of motion (extension 0° and flexion 105°) was achieved without extension lag.

ACKNOWLEDGEMENTS
The authors thank Mr. Dane K. Grace for his efforts in preparing this manuscript for publication.
References
1. Curtis RM. Surgical restoration of motion in the stiff interphalangeal joints of the hand. Bull Hosp Joint Dis. 1970. 31:1–6.
2. Diao E, Eaton RG. Total collateral ligament excision for contractures of the proximal interphalangeal joint. J Hand Surg Am. 1993. 18:395–402.
3. Lorea P, Medina Henriquez J, Navarro R, Legaillard P, Foucher G. Anterior tenoarthrolysis for severe flexion contracture of the fingers (the "TATA" operation): a review of 50 cases. J Hand Surg Eur Vol. 2007. 32:224–229.

4. Curtis RM. Capsulectomy of the interphalangeal joints of the fingers. J Bone Joint Surg Am. 1954. 36-A:1219–1232.

5. Curtis RM. Treatment of injuries of proximal interphalangeal joints of fingers. Curr Pract Orthop Surg. 1964. 23:125–139.
6. Ghidella SD, Segalman KA, Murphey MS. Long-term results of surgical management of proximal interphalangeal joint contracture. J Hand Surg Am. 2002. 27:799–805.

7. Gibraiel EA. A local finger flap to treat post-traumatic flexion contractures of the fingers. Br J Plast Surg. 1977. 30:134–137.

8. Gould JS, Nicholson BG. Capsulectomy of the metacarpophalangeal and proximal interphalangeal joints. J Hand Surg Am. 1979. 4:482–486.

9. Harrison DH, Newton J. Two flaps to resurface the basal flexioncrease of the finger area. J Hand Surg Br. 1991. 16:78–83.

10. Houshian S, Chikkamuniyappa C. Distraction correction of chronic flexion contractures of PIP joint: comparison between two distraction rates. J Hand Surg Am. 2007. 32:651–656.

11. Houshian S, Gynning B, Schrøder HA. Chronic flexion contracture of proximal interphalangeal joint treated with the compass hinge external fixator. A consecutive series of 27 cases. J Hand Surg Br. 2002. 27:356–358.

12. Jackson IT, Brown GE. A method of treating chronic flexion contractures of the fingers. Br J Plast Surg. 1970. 23:373–379.

13. Sprague BL. Proximal interphalangeal joint contractures and their treatment. J Trauma. 1976. 16:259–265.

14. Ulkür E, Acikel C, Karagoz H, Celikoz B. Treatment of severely contracted fingers with combined use of cross-finger and side finger transposition flaps. Plast Reconstr Surg. 2005. 116:1709–1714.
15. Watson HK, Light TR, Johnson TR. Checkrein resection for flexion contracture of the middle joint. J Hand Surg Am. 1979. 4:67–71.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download