Abstract
Purpose
A bile duct stone impacted at the duodenal papilla is an urgent condition that can rapidly lead to either suppurative cholangitis or acute pancreatitis due to almost complete obstruction of the bilio-pancreatic outflow. This study evaluated the clinical characteristics and results of endoscopic treatment for a bile duct stone impacted at the duodenal papilla.
Materials and Methods
Forty-six patients who had been diagnosed with an impacted papillary stone were retrospectively reviewed.
Results
The typical features of acute cholangitis (Charcot's triad) and pancreatitis were only observed only in 10 patients (21.7%) and 17 patients (37.0%), respectively. After the endoscopic retrograde cholangiopancreatography, 30 patients (65.2%) were found to have a solitary stone impacting the duodenal papilla and 16 patients had one or more stones in the bile duct. On the radiological studies, the former patients were associated more commonly with no visible stone or no bile duct dilatation (p < 0.05). All impacted papillary stones were successfully removed by endoscopic sphincterotomy: 23 by a needle knife and 23 by a pull type papillotome. The procedure-related complications (n = 7, 4 bleeding, 3 pancreatitis) were not serious and did not differ, based on endoscopic findings and the procedure used.
A common bile duct (CBD) stone, particularly when impacted at the papilla, can lead to either complete biliary obstruction and suppurative cholangitis or acute pancreatitis due to obstruction of the bilio-pancreatic outflow.1,2 Before the introduction of therapeutic endoscopy, a CBD stone was removed surgically. However, surgery for suppurative cholangitis carries a significant risk of morbidity and mortality.3 In particular, an impacted papillary stone (IPS) is often difficult to remove during surgery, despite the use of a flexible choledochoscope, and a surgical sphincteroplasty is sometimes necessary.
Endoscopic papillotomy is now an established treatment for CBD stones. The success of stone extraction, using this technique, is over 90%.4-6 However, with stone impaction at the papilla, deep cannulation with standard papillotomy is often difficult. Given this situation, an endoscopic choledochoduodenostomy with a needle knife papillotome is a very useful method that can provide an artificial choledochoduodenal fistula, thereby facilitating the removal of the impacted stone from the papilla.1,2,5-12
Here, we present our experience with endoscopic treatment of IPS and evaluate the clinical characteristics associated with early detection of IPS, which may lead to an urgent condition.
Six hundred and ninety-three patients underwent endoscopic retrograde cholangiopancreatography (ERCP) for CBD stones from April 2001 to May 2008. Among these patients, 46 (26 men, 20 women; mean age 62.5 years, range 16 to 88 years) were found to have an impacted CBD stone at the papilla of Vater, i.e. IPS. IPS was defined as an impacted stone at the duodenal papilla at risk for causing biliary or pancreatic outflow obstruction. In addition, the stones had the following characteristic duodenoscopic findings: an edematous, swollen and bulging papilla into the duodenum, a visible stone at the papillary orifice and stones at the papilla confirmed during the endoscopic sphincterotomy.
The following data were noted before ERCP: gender, age, presenting symptoms and signs, white blood cell count, biochemical tests of liver function, and pancreatic enzymes, the diameter of the bile duct, and the presence or absence of the bile duct stone on radiological studies, which included an abdominal CT (Somatom Plus 4, Seimens, Pforzheim, Germany) with/without ultrasonography. All patients underwent abdominal CT before ERCP, and a dilatation of the CBD was defined as > 7 mm at its maximum diameter.
The typical features of acute cholangitis were defined by three clinical manifestations: abdominal pain, jaundice and fever with chills. Acute pancreatitis was defined as a abdominal pain combined with increased serum amylase three times the upper limit of normal.
During the duodenoscopy, the presence or absence of peripapillary diverticulum (PPD), papillitis and a visible stone at the papillary orifice were also recorded. The number of stones was evaluated by the cholangiography obtained by optimal opacification of the biliary tree.
PPD was defined as the presence of a diverticulum within a 2 cm radius from the papilla, and was divided into two types according to the relationship between the papilla and diverticulum: Type A PPD (PPD-A) were papilla located on the inner rim of the diverticulum (juxtapapillary diverticulum) or papilla located deep within the diverticulum (intradiverticular papilla); Type B (PPD-B) were papilla located outside of the diverticulum.13 The definition of papillitis was adopted from the Sydney system for classifying duodenitis.14 A positive finding of papillitis was considered when there was one or more endoscopic findings with the following four characteristic features: erythema, erosion, hemorrhage, and nodularity.
All patients underwent endoscopic treatment first, which was performed using a lateral-viewing duodenoscopy (JF-240 or TJF-240, Olympus, Tokyo, Japan) under conscious sedation with intravenously administered midazolam (2-5 mg) and meperidine (25-50 mg). The duodenal motility was suppressed with an intravenous injection of scopolamine butylbromide (20-40 mg). An endoscopic sphincterotomy was performed using a pull-type or a needle knife papillotome (MTW, Wesel, Germany). The needle knife papillotomy was performed when it was difficult to insert conventional pull-type papillotome into the bile duct because of the impacted stone at the papilla or when the papilla was inaccessible due to massive posterior displacement of the papillary orifice. For a papillotomy with a needle knife papillotome, the papillotomy was started a few millimeters below the proximal edge of the bulging intraduodenal segment of the bile duct after contact of the papillotomy with the bulging papilla. The papillotomy was then extended stepwise toward the duodenal wall and down onto the papilla until the stone spontaneously passed out into the duodenum. Retrieval baskets or balloons were applied when the IPS did not spontaneously pass into the duodenum even after an adequate papillotomy was extended; this might be needed in cases with a large stone or a stone that migrated into the bile duct during a deep cannulation.
The data were analyzed statistically using the Mann Whitney U test to compare the differences between the parameters studied. A p value < 0.05 was considered significant.
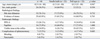
The presenting signs and symptoms were as follows: abdominal pain (n = 44), jaundice (n = 31) and fever with chills (n = 14). Among 46 patients, 15 did not have jaundice (total bilirubin of less than 2.5 mg/dL) even if the stone was impacted at the duodenal papilla. The typical clinical features of acute cholangitis (Charcot's triad) were observed only in 10 patients (21.7%), and they were significantly associated with the findings of the stone on radiological studies (p < 0.05). Acute pancreatitis was observed in 17 patients (37.0%), which was associated with young age (less than 60 years), the presence of PPD-A, a solitary stone impacting the duodenal papilla, and a visible stone at the papillary orifice on the duodenoscopy (Table 1) (p < 0.05).
Radiological studies including abdominal CT and transabdominal ultrasonography revealed 35 patients (76.1%) with CBD dilatation and 29 patients (63.0%) with stones in the CBD or at the papilla. Seventeen patients (37.0%) showed no radiological evidence of stones or no dilation of the CBD, which was significantly associated with a solitary stone impacted at the papilla without additional bile duct stones and inversely associated with male gender and the presence of Charcot' triad (Table 1) (p < 0.05).
On ERCP, 30 patients (65.2%) were found to have a solitary stone impacting the duodenal papilla and 16 patients had one or more stones in the CBD. The former patients were associated more commonly with the presence of acute pancreatitis and no visible stone or no bile duct dilatation on the radiological studies (p < 0.05).
The duodenoscopy revealed the papillae to be edematous, swollen and bulging into the duodenum in all patients (Fig. 1). Thirty-four patients (73.9%) had a papillitis including hyperemic changes and erosions or hemorrhagic changes on the surface of the papilla. The presence of papillitis was associated with young age and a visible stone at the papillary orifice on the duodenoscopy (p < 0.05). A visible stone at the papillary orifice was found in 16 patients (34.8%); in these cases, it was associated significantly with the presences of pancreatitis and papillitis. PPD was found in 12 patients (26.1%), each type having 6 cases. The presence of PPD-A was associated significantly with the presence of pancreatitis (Table 1) (p < 0.05).
Endoscopic therapy was successful in all patients. At the first ERCP session, the impacted stone was completely removed in 44 patients (95.7%). Two patients initially had endoscopic nasobiliary drainage and then stone removal several days later because they were using antiplatelet agents.
In 23 out of the 44 treated patients, the bile duct cannulation using a standard catheter or a pull-type papillotome was unsuccessful at the first session of the ERCP, because of the tight obstruction at the papillary orifice by the impacted stone, or a marked displacement of the papillary orifice posteriorly. In these cases, an endoscopic choledochoduodenostomy using a needle knife was performed.
ERCP-induced complications developed in 7 patients, however, none was serious. Bleeding in 4 patients was controlled successfully by an epinephrine injection at the edge of the sphincterotomy site. Three patients with initially normal pancreatic enzymes developed mild acute pancreatitis which did not require specific treatment. There was no significant difference in radiologic and endoscopic findings as well as the complication rate between patients treated with the needle knife and conventional pull type papillotome (Table 2).
Traditionally, a CBD stone impacted at the duodenal papilla has been considered as an urgent condition that can rapidly lead to either suppurative cholangitis or acute pancreatitis due to almost complete obstruction of the biliopancreatic outflow.1,2 Therefore, the removal of the IPS should expeditiously be performed in order to prevent these complications.
Endoscopic papillotomy is currently an established treatment for CBD stones. The performance of a sphincterotomy is dependent upon the ability of the endoscopist to introduce a papillotome sufficiently deep into the common bile duct. However, either an impacted stone or anatomic variant, natural or acquired, can prohibit complete introduction of the papillotome.1,2,5-12,15-19 For example, an impacted stone at the papilla may hinder a standard papillotomy because of the displacement and obstruction of the papillary orifice. Osnes and Kahrs20 first described the papillotomy technique using a needle knife papillotome in 1977. Since its introduction, the use of a needle knife papillotome has gained popularity as a "pre-cut papillotome"; this procedure facilitates biliary cannulation in patients who fail with the standard techniques, and is an effective method for removing an impacted stone at the papilla. However, this device has been associated with duodenal perforations and pancreatitis, and is generally believed to be rather risky.21-23 However, Compared with cutting a normal papilla, the use of the needle knife is relatively safe in patients with IPS; this is because the pancreatic duct lies posterior to the impacted stone and the intraluminal surface is greater due to the stretching caused by the stone.1,2,9,12 Therefore, the risk of perforation and/or pancreatitis may be reduced. Hemorrhaging has been a significant complication, which may be related to the edematous and congested papilla.24
In this study, 23 patients underwent an endoscopic sphincterotomy using a needle knife papillotome. Among these patients, only three patients suffered procedure-related complications: two had bleeding and one developed pancreatitis. Compared to the cases with the pull-type papillotome (two bleeding and two pancreatitis), there was no significant difference in the complication rates. In addition, endoscopic papillitis and PPD were not influenced by the sphincterotomy-induced complications. Although a successful sphincterotomy without complications depends on the endoscopist's skill, a needle knife papillotome might be used safely in patients with IPS regardless of the presence of endoscopic papillitis.
Suspicion of an IPS is dependent usually on the clinical manifestations and findings on the radiological studies. However, as shown in this study, radiological studies do not always locate a stone in the bile duct and the papilla (n = 17, 37.0%), and the diameter of the bile duct might be within normal range (n = 11, 23.9%) even with a stone impacted in the distal bile duct. Furthermore, the typical manifestations of acute cholangitis (n = 10, 21.7%) and acute pancreatitis (n = 17, 37.0%) due to an impacted stone at the papilla were less common than expected. The absence of some of these manifestations might partially be explained by the patients who present early to the hospital because of severe abdominal pain, therefore, there was not enough time for the bile duct to become dilated and for full-blown signs and symptoms of cholangitis to develop.
The characteristic endoscopic findings of an IPS are a prominent and bulging papilla with a posterior displacement of the papillary orifice.1,2 These findings were confirmed in this study. The papillitis was significantly associated with abdominal pain and a visible stone at the papillary orifice during the duodenoscopy. At first, we thought that the PPD-A might affect some of the endoscopic findings including papillitis and a visible stone at the papillary orifice, depending on the degree of incarceration of the stone at the papilla, and that it might also affect the outcome of endoscopic therapy; this is because PPD can cause a difficult cannulation of the papilla for the ERCP. However, the PPD-A did not influence the findings.
The limitations of this study include the following. First, the time interval between the onset of symptoms and endoscopic procedure was not considered because some patients knew precisely when the symptoms began, while others did not. However, almost all patients had severe abdominal pain on the day of their hospital visit, and this was believed to be the key factor for visiting the hospital. Therefore, we evaluated clinical manifestations including acute cholangitis, pancreatitis and jaundice at the time of hospital visit. Second, the size of the IPS could not be measured. From the beginning of this study, it was believed that this factor might play an important role in determining the degree of stone impaction within the papilla. However, to obtain a complete cholangiography was difficult in practice because of the impacted stone within the papilla. In addition, an endoscopic papillotomy had been performed prior to bile duct cannulation in more than half of the cases, therefore, the measurement of the size of the IPS was impossible. Furthermore, during the endoscopic papillotomy, the stone within the papilla was suddenly expelled into the duodenum. At that moment, it was hard to locate the stone in the duodenum and measure its size. Therefore, the size of the impacted stone could not be analyzed in our study. Thirdly, endoscopic papillitis was defined based on the Sydney classification of duodenitis. Although the duodenal papilla and duodenum are covered by the same mucosa, it does not appear to be appropriate to adopt the Sydney system of duodenitis for the definition of papillitis, considering the relationship between papillitis and pancreaticobiliary disease.25 Therefore, it appears to be necessary to establish a new system for defining papillitis. Fourthly, we did not randomize the patients into pull type papillotome or needle knife papilltome for sphincterotomy. As mentioned in the methodology section, an endoscopic sphincterotomy was performed first using a pull-type papillotome. The needle knife papillotomy was performed only when there was a tight obstruction at the papillary orifice by the impacted stone or when the papilla was inaccessible due to massive posterior displacement of the papillary orifice. Therefore, it was not possible to randomize the use of papillotome in that situation.
In conclusion, suspicion of an IPS should be based on both the clinical manifestations and radiological findings; one or both of these evaluations may not be successful to detect an early IPS. Endoscopic stone removal in patients with an impacted bile duct stone at the papilla of Vater can be performed by conventional methods using a pull-type papillotome or choledochoduodenostomy with a needle knife papillotome. The needle knife papillotomy is especially useful in patients in whom biliary access is not possible by the conventional approach; this technique appears to be as safe as conventional methods with the full-type papillotome.
Figures and Tables
Fig. 1
Endoscopic findings of impacted bile duct stone at the duodenal papilla. (A) The duodenal papilla is edematous and massively bulging into the duodenum. (B) The stone is easily exposed after needle knife choledo-choduodenostomy. (C) The stone is spontaneously passes into the duodenum immediately after full sphincterotomy.

References
1. Leung JW, Banez VP, Chung SC. Precut (needle knife) papillotomy for impacted common bile duct stone at the ampulla. Am J Gastroenterol. 1990. 85:991–993.
2. Binmoeller KF, Katon RM. Needle knife papillotomy for an impacted common bile duct stone during pregnancy. Gastrointest Endosc. 1990. 36:607–609.

3. Heinerman PM, Boeckl O, Pimpl W. Selective ERCP and preoperative stone removal in bile duct surgery. Ann Surg. 1989. 209:267–272.

4. Freitas ML, Bell RL, Duffy AJ. Choledocholithiasis: evolving standards for diagnosis and management. World J Gastroenterol. 2006. 12:3162–3167.
5. Cotton PB, Vallon AG. British experience with duodenoscopic sphincterotomy for removal of bile duct stones. Br J Surg. 1981. 68:373–375.
6. Siegel JH. Precut papillotomy: a method to improve success of ERCP and papillotomy. Endoscopy. 1980. 12:130–133.
7. Akcakaya A, Ozkan OV, Okan I, Kocaman O, Sahin M. Endoscopic retrograde cholangiopancreatography during pregnancy without radiation. World J Gastroenterol. 2009. 15:3649–3652.

8. McAlister VC, Roy A, Passi RB. Harpoon extraction of a common bile duct stone impacted at the ampulla of Vater with needle-knife sphincterotome. Gastrointest Endosc. 1993. 39:111–112.

9. Conio M, Saccomanno S, Aste H, Pugliese V. Precut papillotomy: primum non nocere. Gastrointest Endosc. 1990. 36:544.

10. Siegel JH, Ben-Zvi JS, Pullano W. The needle knife: a valuable tool in diagnostic and therapeutic ERCP. Gastrointest Endosc. 1989. 35:499–503.
11. Kozarek RA, Sanowski RA. Endoscopic choledochoduodenostomy. Gastrointest Endosc. 1983. 29:119–121.
12. Schapira L, Khawaja FI. Endoscopic fistulo-sphincterotomy: an alternative method of sphincterotomy using a new sphincterotome. Endoscopy. 1982. 14:58–60.
13. Kim DI, Kim MH, Lee SK, Seo DW, Choi WB, Lee SS, et al. Risk factors for recurrence of primary bile duct stones after endoscopic biliary sphincterotomy. Gastrointest Endosc. 2001. 54:42–48.

14. Tytgat GN. The Sydney System: endoscopic division. Endoscopic appearances in gastritis/duodenitis. J Gastroenterol Hepatol. 1991. 6:223–234.

15. Rajnakova A, Goh PM, Ngoi SS, Lim SG. ERCP in patients with periampullary diverticulum. Hepatogastroenterology. 2003. 50:625–628.
16. Lobo DN, Balfour TW, Iftikhar SY. Periampullary diverticula: consequences of failed ERCP. Ann R Coll Surg Engl. 1998. 80:326–331.
17. Vaira D, Dowsett JF, Hatfield AR, Cairns SR, Polydorou AA, Cotton PB, et al. Is duodenal diverticulum a risk factor for sphincterotomy? Gut. 1989. 30:939–942.

18. Cotton PB. Endoscopic management of bile duct stones; (apples and oranges). Gut. 1984. 25:587–597.
19. Kirk AP, Summerfield JA. Incidence and significance of juxtapapillary diverticula at endoscopic retrograde cholangiopancreatography. Digestion. 1980. 20:31–35.
20. Osnes M, Kahrs T. Endoscopic choledochoduodenostomy for choledocholithiasis through choledochoduodenal fistula. Endoscopy. 1977. 9:162–165.
21. Wang P, Li ZS, Liu F, Ren X, Lu NH, Fan ZN, et al. Risk factors for ERCP-related complications: a prospective multicenter study. Am J Gastroenterol. 2009. 104:31–40.
22. Williams EJ, Taylor S, Fairclough P, Hamlyn A, Logan RF, Martin D, et al. Risk factors for complication following ERCP; results of a large-scale, prospective multicenter study. Endoscopy. 2007. 39:793–801.

23. Cotton PB. Precut papillotomy--a risky technique for experts only. Gastrointest Endosc. 1989. 35:578–579.

24. Kim HJ, Kim MH, Kim DI, Lee HJ, Myung SJ, Yoo KS, et al. Endoscopic hemostasis in sphincterotomy-induced hemorrhage: its efficacy and safety. Endoscopy. 1999. 31:431–436.

25. Park JS, Kim MH, Lee SK, Seo DW, Lee SS, Chang HS, et al. The clinical significance of papillitis of the major duodenal papilla. Gastrointest Endosc. 2002. 55:877–882.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download