This article has been corrected. See "Erratum to "The Urologist's View of Male Overactive Bladder: Discrepancy between Reality and Belief in Practical Setting" by Lee SH, et al. (Yonsei Med J 2010;51:432-437)" in Volume 51 on page 615.
Abstract
Purpose
In order to gain insight into the physicians' awareness of and attitude towards management of overactive bladder (OAB) in males, we performed a nationwide survey of the current strategies that urologists use to diagnose and manage OAB in male patients.
Materials and Methods
A probability sample was taken from the Korean Urological Association Registry of Physicians, and a random sample of 289 Korean urologists were mailed a structured questionnaire that explored how they manage benign prostatic hyperplasia (BPH).
Results
A total of 185 completed questionnaires were returned. The consent rate in the survey was 64.5%. Eighty-one (44%) urologists believed that of all males with lower urinary tract symptoms (LUTS), 20% or more had OAB and 72 (39%) believed that 10-20% had OAB. Half of the urologists surveyed believed that the most bothersome symptom in male OAB patients was nocturia. Seventy-three percent of respondents reported that they prescribed alpha blockers with anticholinergics for first line management, while 19% of urologists prescribed alpha blocker monotherapy but not anticholinergics for OAB patients. Though acute urinary retention (AUR) was considered the anticholinergic adverse event of most concern, the most frequently observed adverse event was dry mouth (95%).
Conclusion
The present study provides insights into urologist views of male OAB. There is a discrepancy between the awareness of urologists and actual patterns of diagnosis and treatment of male OAB. This finding indicates the need to develop further practical guidelines based on solid clinical data.
Overactive bladder (OAB) is defined as urgency, with or without urge incontinence, usually accompanied by increased daytime frequency and nocturia.1 OAB is a serious health problem because of its high prevalence and its significantly associated burden. The EPIC study2 reported that the overall prevalence of OAB is 12%, with similar rates in men and women, and that the prevalence of OAB increases with age.
The treatment of lower urinary tract symptoms (LUTS) in men is complicated by the fact that storage and voiding symptoms frequently coexist.3 It is unclear whether storage symptoms may develop secondary to bladder outlet obstruction (BOO) in men.4 However, storage symptoms often occur independently of BOO and persist in many men despite pharmacologic or surgical treatment.5 Therefore, therapies that target the prostate often fail to alleviate OAB symptoms and may not be the most appropriate therapy for men with storage LUTS.3
At present, relatively little is known about clinical prescribing patterns of OAB in Asia, although several studies in other countries have revealed underdiagnosis of OAB.6,7 To gain insight into urologist awareness and attitudes toward management of OAB in males, we performed a nationwide survey in Korea of the current strategies urologists use for diagnosis and management of patients with OAB.
We obtained a probability sample (n = 448) of Korean urologists from the Korean Urological Association (KUA) Registry of Physicians and selected 289 participants who were informed of the purpose of the survey and agreed to be enrolled before the survey began. The eligibility criteria required that participants be urologists not in residency training and in active practice at least 20 hours per week
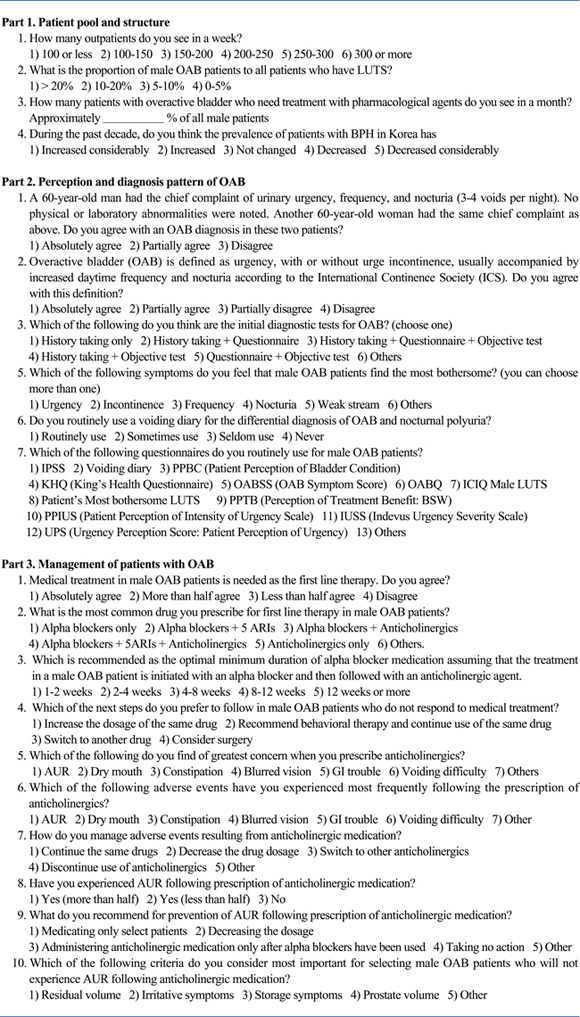
The survey was conducted from October 2008 to November 2008. It was based on a structured questionnaire delivered via e-mail. Participants received the survey instrument, which consisted of a cover letter that identified the author and described the purpose of the survey and the survey questionnaire itself. The questionnaire was developed by the authors of this paper. The survey instrument was also reviewed and revised by additional experts and pretested for clarity and convenience. The survey questionnaire was divided into three parts. Part One of the questionnaire focused on the patient pool and structure, and was comprised of four separate items. Part Two of the questionnaire comprised seven separate items related to the perception and diagnosis pattern of patients with OAB. Part Three of the questionnaire comprised 10 separate items related to the strategy used for medication and the individual physician's preference concerning medical therapy (see Appendix). The data collected from the survey are presented descriptively; therefore, no statistical analyses were performed.
A total of 185 completed questionnaires were returned by urologists. The consent rate in the survey was 64.5% (73.2% in private clinics, 62.7% in general hospitals), and the compliance rate for the 289 urologists who initially agreed to participate was 64.0%. In the total sample, 26% of urologists described their practice as 'private clinics', while 74% described their practice as 'hospital practice'.
In the questionnaire, the case studies of two 60 year-old patients, one male and one female, with urinary urgency, frequency, and nocturia were presented. Neither of these patients had physical or laboratory abnormalities. One hundred thirteen urologists (61%) agreed with an OAB diagnosis; however, 66 urologists (36%) partially agreed and 6 (3%) disagreed.
In response to a question asking what information the urologist felt that he/she need to diagnose OAB in males, 97 (52%) urologists replied that they required information obtained from interviews, questionnaires, and objective tests (Table 1). The International Prostate Symptom Score (IPSS) questionnaire was the most commonly-used questionnaire, while a voiding diary was the second most common diagnostic method. OAB questionnaires (OABQ) were used by about 15% of respondents.
Urologists thought that the most bothersome symptom of OAB was nocturia (n = 100, 54%), and the second most bothersome symptom was urgency (n = 54, 29%) (Fig. 1). However, only 83 (45%) urologists believed that the initiating factors of OAB in males could be determined in patients with symptoms of OAB.
Ninety-nine percent of respondents (n = 182) replied that they chose medical treatment as the initial management option for patients with OAB. Table 2 shows the initial treatment patterns for patients with OAB. Seventy-three percent of the respondents reported that they prescribed alpha blockers with anticholinergics as first line management, while anticholinergic monotherapy or alpha blocker monotherapy was used less frequently (6% vs. 16%, respectively). Fifty-six percent of the respondents prescribed alpha blockers for a minimum of two to four weeks before anticholinergics. In response to the question concerning which management option to use for patients unresponsive to initial management, 68 respondents (36%) replied that they would switch to another medication while 61 respondents (33%) replied that they would continue prescribing the current medication with behavioral therapy. Another 55 respondents (30%) replied that they would increase the dosage (Fig. 2). When urologists prescribed anticholinergics, their primary concern was acute urinary retention (AUR), and the second was dry mouth (59% vs. 11%, respectively). However, the most frequently experienced adverse event was dry mouth (95%), while AUR was uncommon (3%). With regard to which management option the urologists would choose if adverse events occurred, 37% replied that they would change to another anticholinergic, 29% replied that they would reduce the dosage, 21% replied that they would continue administering the same drug, and 11% reported that they would discontinue prescribing the drug.
We surveyed the views of a broad range of urologists based in both hospitals and private clinics. The response rate of 64.0% in this study is much higher than the 5-10% response rates achieved through postal surveys.8
International differences in OAB prevalence have been observed. A multinational study in six European countries demonstrated significant variation in prevalence, with Spain reporting the highest (22%) prevalence and France reporting the lowest (12%) prevalence.7 However, in Asian samprles, the prevalence of OAB has been reported to be even higher. The prevalence of OAB in Asian men was recently evaluated in 11 Asian countries. A questionnaire was sent to over 2,000 men aged from 18 to 70 years.9 An OAB prevalence of about 30% was observed in the Asian male population (range, 14-84%). Frequency and urgency were the most commonly reported symptoms, while 13% of individuals examined reported urge incontinence. However, it is still unclear whether the higher prevalence rate in Asia is truly reflective of international differences. Moreover, there are fewer reports about the incidence of male OAB than all male LUTS. It has been observed that 45% to 75% of men with BOO have OAB symptoms.10,11 However, in our survey, 56% of urologists believed that the incidence of OAB patients among all male LUTS was less than 20%. This finding may result from a discrepancy between the awareness of the physician and his/her patients. Most urologists focus on LUTS/benign prostatic hyperplasia (BPH), especially in elderly men, and do not regard OAB symptoms to be a serious problem until they become severe. Further studies that focus on the real incidence of OAB patients among all male LUTS patients are required to compare the findings for Asian populations with those for Western populations.
In our survey, 54% of respondents regarded nocturia as the most bothersome symptom of male OAB. This result, however, has not been consistently observed across epidemiologic studies. Johansson, et al.12 suggested that nocturia is one of the most bothersome symptoms of LUTS in men and women. Another study noted that nocturia was the second most bothersome symptom after urinary urgency.13 Although nocturia is highly prevalent in elderly people, it only has a minor impact on daily life and few individuals seek medical care.14 This is largely because Koreans believe that nocturia is a normal consequence of aging and not a disease. This, however, may indicate that patients who complain of nocturia in Korea may have more serious nocturia than patients surveyed in other studies.
There is a rationale for prescribing anticholinergics not only to men with LUTS, but also to men with OAB. However, guidelines from the European Association of Urologists make no mention of the possible therapeutic role of anticholinergics for treating storage symptoms in such patients. Moreover, many physicians are still reluctant to prescribe anticholinergics due to the concern of urinary retention, especially in men with BOO. Several studies have reported that prescribing anticholinergics to men with LUTS or even BOO does not seem to elevate the risk of AUR.15,16 In our study, almost all urologists agreed that anticholinergics are needed to treat male OAB. However, 19% of urologists did not prescribe anticholinergics and instead opted for alpha blocker monotherapy in OAB patients. The most frequently experienced adverse event was dry mouth, but urologists were most concerned about AUR.
These findings are interesting for several reasons. Urologists in Korea appear to give more weight to BOO in elderly men than OAB, and are concerned with prescribing anticholinergics to males with OAB. It is obvious that there is significant overlap between the male OAB population and men with LUTS. Both may result from pathophysiologic mechanisms such as benign prostatic enlargement, benign prostatic obstruction, detrusor overactivity, or from a combination of prostate and bladder dysfunctions.17 It is debatable whether a distinction between male LUTS and OAB is clinically relevant and whether or not it influences treatment decisions. Further epidemiologic studies are needed to confirm the effect of actual practice patterns in males with OAB.
The results of the current survey should be viewed within the context of its limitations. This survey is not an epidemiologic study. The data used in this survey are based only on the awareness of urologists, which could introduce a degree of subjectivity. Second, all data were collected by an e-mail survey and self-administered questionnaires. Different survey modes may have different sampling errors, response rates, data completeness, and measurement errors.18 In particular, fewer urologists in private clinics than urologists working in hospitals participated in this study. This could introduce a sampling error given that the general distribution of Korean urologists in private clinics is about half that of all the urologists. However, despite these limitations, this descriptive survey indicates the need for more practical diagnosis guidelines and a treatment consensus.
In conclusion, in this study, we have provided insights into urologist views of male OAB. There is a discrepancy between urologist awareness and the actual diagnosis and treatment of male OAB. This finding indicates the need to further develop practical guidelines based on solid clinical data, and to ensure that these guidelines are widely promoted and accepted by the urological community.
Figures and Tables
Fig. 2
Treatment alternatives for male OAB patients who do not respond to medication. OAB, overactive bladder.

References
1. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002. 21:167–178.

2. Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006. 50:1306–1314.

3. Chapple CR, Roehrborn CG. A shifted paradigm for the further understanding, evaluation, and treatment of lower urinary tract symptoms in men: focus on the bladder. Eur Urol. 2006. 49:651–658.

4. Abdel-Aziz KF, Lemack GE. Overactive bladder in the male patient: bladder, outlet, or both? Curr Urol Rep. 2002. 3:445–451.

5. de Nunzio C, Franco G, Rocchegiani A, Iori F, Leonardo C, Laurenti C. The evolution of detrusor overactivity after watchful waiting, medical therapy and surgery in patients with bladder outlet obstruction. J Urol. 2003. 169:535–539.

6. Goepel M, Hoffmann JA, Piro M, Rübben H, Michel MC. Prevalence and physician awareness of symptoms of urinary bladder dysfunction. Eur Urol. 2002. 41:234–239.

7. Milsom I, Abrams P, Cardozo L, Roberts RG, Thüroff J, Wein AJ. How widespread are the symptoms of an overactive bladder and how are they managed? A population-based prevalence study. BJU Int. 2001. 87:760–766.
8. Djavan B, Nickel JC, de la Rosette J, Abrams P. The urologist view of BPH progression: results of an international survey. Eur Urol. 2002. 41:490–496.

9. Moorthy P, Lapitan MC, Quek PL, Lim PH. Prevalence of overactive bladder in Asian men: an epidemiological survey. BJU Int. 2004. 93:528–531.
10. Knutson T, Edlund C, Fall M, Dahlstrand C. BPH with coexisting overactive bladder dysfunction--an everyday urological dilemma. Neurourol Urodyn. 2001. 20:237–247.
11. Ameda K, Sullivan MP, Bae RJ, Yalla SV. Urodynamic characterization of nonobstructive voiding dysfunction in symptomatic elderly men. J Urol. 1999. 162:142–146.

12. Johansson C, Hellström L, Ekelund P, Milsom I. Urinary incontinence: a minor risk factor for hip fractures in elderly women. Maturitas. 1996. 25:21–28.

13. Eckhardt MD, van Venrooij GE, van Melick HH, Boon TA. Prevalence and bothersomeness of lower urinary tract symptoms in benign prostatic hyperplasia and their impact on well-being. J Urol. 2001. 166:563–568.

14. Choo MS, Ku JH, Park CH, Lee YS, Lee KS, Lee JG, et al. Prevalence of nocturia in a Korean population aged 40 to 89 years. Neurourol Urodyn. 2008. 27:60–64.

15. Abrams P, Kaplan S, De Koning Gans HJ, Millard R. Safety and tolerability of tolterodine for the treatment of overactive bladder in men with bladder outlet obstruction. J Urol. 2006. 175:999–1004.

16. Kaplan SA, Walmsley K, Te AE. Tolterodine extended release attenuates lower urinary tract symptoms in men with benign prostatic hyperplasia. J Urol. 2005. 174:2273–2275.

17. Barry MJ, Cockett AT, Holtgrewe HL, McConnell JD, Sihelnik SA, Winfield HN. Relationship of symptoms of prostatism to commonly used physiological and anatomical measures of the severity of benign prostatic hyperplasia. J Urol. 1993. 150:351–358.

18. Bowling A. Mode of questionnaire administration can have serious effects on data quality. J Public Health (Oxf). 2005. 27:281–291.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download