Abstract
The aim of this study was to investigate the relationship of cyclooxygenase (COX)-2 and p53 expression with prognosis in patients with conventional renal cell carcinoma (RCC). Formalin-fixed, paraffin-embedded tissue sections of conventional RCC from 92 patients, who had undergone radical nephrectomy, were examined for COX-2 and p53 expression by immunohistochemistry and compared with clinicopathological variables. The COX-2 expression significantly correlated only with tumor size (p=0.049), whereas the p53 expression profoundly correlated with the TNM stage (p=0.024), M stage (p=0.001), and metastasis (synchronous or metachronous; p=0.004). The COX-2 overexpression did not significantly associate with p53 positivity (p=0.821). The survival rate of patients correlated with the p53 expression (p<0.0001) but not with the COX-2 expression (p=0.7506). Multivariate analyses indicated that tumor size, M stage, and p53 expression were independent prognostic factors for cancer-specific survival. The COX-2 expression was not an independent factor. These results show that the increased expression of p53 was associated with metastasis and a worse prognosis in conventional RCC, which suggests that p53 might have played an important role in the progression of conventional RCC. The increased expression of COX-2 was associated only with tumor size, but may not be an important prognostic factor in conventional RCC. No association was observed between COX-2 overexpression and p53 positivity in conventional RCC.
The renal cell carcinoma (RCC) is the most common malignant tumor of the adult kidney, and its incidence is increasing.1 To date, tumor stage and grade have been considered the most important prognostic parameters for patients with RCC. However, in many cases, these parameters were insufficient to predict the clinical behavior of RCC tumors.2,3 Therefore, it is important to identify additional indicators of the biological aggressiveness of RCC.
Cyclooxygenase (COX) catalyzes the synthesis of prostaglandins from arachidonic acid. There are two isoforms of COX: COX-1 and COX-2. While COX-1 is constitutively expressed, COX-2 is induced by various stimuli such as the cytokines, growth factors, and tumor promoters.4,5 The COX-2 levels have been shown to increase in several types of human cancers like the ones which develop in the gastrointestinal tract, breast, cervix, lung, prostate, and bladder.6-12 This suggests that the COX-2 may play an important role in the cancer progression by affecting tumor cell proliferation, resistance to apoptosis, angiogenesis, immunosuppression, and tumor invasion.7,13-15 However, the relationship between the COX-2 expression and RCC remains unclear. Although the COX-2 is highly expressed in canine RCC,16 it is down-regulated in RCC in the Eker (TSC2 gene mutant) rat model.17 The COX-2 is highly expressed in human RCC, but the results of its correlation with tumor stage and grade have been contradictory.18,19
Apoptosis is a critical pathway that selectively allows certain cells with damaged DNA to undergo cell death. Abnormalities in this pathway may lead to uncontrolled cellular proliferation and, ultimately, to carcinogenesis. p53 is a known inducer of apoptosis, and it is the most common genetic mutant found in cancers. There are wide variations in the reported incidence of p53 related mutations in RCC, and its prognostic significance for this type of cancer remains controversial. Some researchers have reported that p53 mutations in the case of RCC may be used as a prognostic factor,20,21 but others disagreed.22,23 Recent evidences have suggested that COX-2 may also inhibit apoptosis.13
In the present study, the expressions of COX-2 and p53 was investigated, and their relationships to clinicopathological variables in patients with conventional RCC were evaluated.
Formalin-fixed, paraffin-embedded, archival surgical specimens that had been obtained from 92 patients (71 men and 21 women; mean age, 54.8 years; range, 26 - 81 years) who had received a diagnosis of primary conventional RCC were studied. All patients underwent radical nephrectomy at our institution between January 1995 and September 2002. During the lymphadenectomy, only the renal hilar lymph nodes were routinely removed. Whenever an enlarged lymph node was observed during surgery, a node dissection clearing the ipsilateral great vessel and the renal hilum was performed. Tumors were staged according to the 1997 revised TNM system,24 and were graded according to Fuhrman's nuclear grading system.25
Paraffin-embedded blocks were sectioned at 4-µm thickness, deparaffinized, and rehydrated. After microwave pretreatment in citrate buffer (pH 6.0) for antigen retrieval, slides were immersed in 3% hydrogen peroxide for 10 minutes to block the endogenous peroxidase activity. The sections were blocked for 10 minutes with blocking reagent using the Cap-Plus™ Detection Kit (ZYMED, San Francisco, CA, USA). Sections were then incubated manually with goat monoclonal antibody to COX-2 (diluted 1 : 200; Santa Cruz Biotechnology, Santa Cruz, CA, USA) for 1 hour at 37℃ or with mouse monoclonal antibody to p53 (diluted 1 : 20; Novo Castra, Newcastle, UK) overnight at 4℃ in a humidified chamber. After a second incubation with a biotinylated secondary antibody, slides were incubated with peroxidase-conjugated streptavidin (DAKO LSAB+ Kit; DAKO Corp., Carpinteria, CA, USA) for COX-2 or the Cap-Plus™ Detection Kit (ZYMED) for p53. Reaction products were visualized by immersing the slides in diaminobenzidine tetrachloride and then counterstaining them with Mayer's hematoxylin. The positive staining of smooth muscle cells from blood vessels provided an internal positive control for COX-2 immunostaining. The colon carcinoma samples with known p53 mutations and documented accumulation of p53 by immunohistochemistry were used as positive control for p53. Negative controls were obtained by omitting the primary antibody.
The immunostaining was independently evaluated by two pathologists who were unaware of the clinical data. The COX-2 expression was based on the presence of the cytoplasmic staining, which was semi-quantitatively estimated according to the methods described by Sinicrope et al.,26 with minor modifications. On the basis of the percentages of immunopositive cells, the data were subdivided into five categories as follows: (0) ≤ 10%; (1) 11 - 25%; (2) 26 - 50%; (3) 51 - 75%; and (4) > 75% positive cells. The immunointensity was also subclassified into four categories: (0) negative; (1) weak; (2) moderate (same intensity of smooth muscle cells); and (3) strong (Fig. 1). The immunoreactive scores for each case were generated by multiplying the values of the two parameters, which were then stratified into three groups: weak (scores 0 - 4), moderate (scores 5 - 8), and strong (scores 9 - 12) COX-2 expression for the survival analysis. The p53 immunostaining was considered to be positive when 10% or more of the tumor cell nuclei were stained (Fig. 2).
Either an independent-sample t-test or a chi-square test was used to analyze the correlation between COX-2 or p53 expression and various clinicopathological variables. The relationship between COX-2 and p53 expression was evaluated by the Mann-Whitney U-test. The paired t-test or McNemar test was used for the correlation of the primary and metastatic sites in the expression of the COX-2 or p53. The survival calculations were illustrated with Kaplan-Meier curves, and univariate and multivariate analyses were performed using the log-rank test or the Cox proportional-hazards regression model. The values of p<0.05 were considered to be statistically significant in all of the analyses.
The clinicopathological characteristics of the 92 patients are summarized in Table 1. Sixty-seven patients were disease-free at a median follow-up of 36 months (range, 12 - 96 months); the other 25 patients had either synchronous metastases (n=12) at the time of nephrectomy or metachronous metastases (n=13) a median of 23 months (range, 4 - 72 months) after nephrectomy. Fourteen patients died during the follow-up period, 7 with synchronous metastases and 7 with metachronous metastases. For 18 of the 25 patients with metastases, their metastases were confirmed histopathologically.
Of the 92 sections, the COX-2 expression (immunoreactive scores) was weak in 17 (18.5%), moderate in 21 (22.8%), and strong in 54 (58.7%). Positive immunostaining for p53 was observed in 11 (12.0%) of the 92 sections.
Because only 1 patient had lymph node metastasis, the analysis according to the lymph node status was not performed. The COX-2 expression significantly correlated with the tumor size (p=0.049) but not with the TNM stage (p=0.541), T stage (p=0.368), M stage (p=0.394), grade (p=0.658), or metastasis (synchronous or metachronous; p=0.564). The p53 expression profoundly correlated with the TNM stage (p=0.024), M stage (p=0.001), and metastasis (p=0.004) but not with the tumor size (p=0.777), T stage (p=0.480), or grade (p=0.829) (Table 2).
The COX-2 overexpression did not significantly associate with p53 positivity (p=0.821). The expressions of COX-2 (p=0.476) and p53 (p=0.125) were not significantly different between the primary and metastatic sites. A Kaplan-Meier survival curve showed that the survival rate of patients with p53-positive tumors was significantly lower than that of patients with p53-negative tumors (p<0.0001) (Fig. 3). There was no difference in the survival rates according to the level of the COX-2 expression (p=0.7506) (Fig. 4).
The univariate analyses identified tumor size, TNM stage, T stage, M stage, and p53 expression as significant prognostic factors for cancer-specific survival, whereas the multivariate analyses indicated that tumor size (p=0.002), M stage (p<0.001), and p53 expression (p=0.016) were independent prognostic factors. The COX-2 expression was not an independent factor (Table 3).
An elevated COX-2 expression has been observed in several types of human cancers, and the overexpression of the COX-2 has been shown to correlate with carcinogenesis and poor prognostic outcome.6-12 However, past studies in RCC have been limited, and the relationship between the COX-2 expression and RCC remains unclear.
Khan et al.16 showed that COX-2 was overexpressed in 2 of 3 dogs with spontaneously developed RCC, which suggested that COX-2 might play a role in the modulation of neoplastic cell growth. Conversely, Okamoto et al.17 found that COX-2 mRNA expression was down-regulated in 8 of 10 spontaneously developed RCCs of Eker (TSC2 gene mutant) rats and that it was not down-regulated, but showed almost the same intensity as in the normal kidney in the other two rats.
With regard to the human RCC, Hara et al.27 showed that COX-2 was overexpressed in RCC but that the expression levels did not correlate with cancer grade. In RCC, the immunoreactive signals in granular cell subtypes were stronger than those in clear cell subtypes. Miyata et al.18 found that increased COX-2 expression was observed in 70 (53.4%) of 131 patients with RCC. Among the patients, 84% had conventional RCC. The COX-2 expression significantly associated with various clinicopathological variables, including the T stage, N stage, M stage, and tumor grade. It was correlated with the Ki-67 labeling index, microvessel density, and MMP-2 expression but not with the apoptotic index. The COX-2 expression was identified as an independent risk factor for large tumor size (> 7 cm) but not an independent prognostic factor for cancer-specific survival, which suggested that the COX-2 is not a significant prognostic factor in RCC.
In the present study, only the conventional RCC was studied in order to exclude the influence of the histologic type. The COX-2 expression was moderate or strong in 75 (81.5%) of the 92 RCC samples. The COX-2 expression significantly correlated with the tumor size but not with the TNM stage, T stage, M stage, grade, or metastasis (synchronous or metachronous). There was no difference in the survival rates according to the level of the COX-2 expression. The COX-2 expression was not an independent prognostic factor for cancer-specific survival according to our multivariate analysis. The results show that COX-2 is not an important prognostic factor in conventional RCC. These results are in agreement with those of Yoshimura et al.19 who reported that COX-2 overexpression was detected in RCC tissues but was not associated with tumor stage or grade. The findings of the present study are also in keeping with the results of Miyata et al.18 that the COX-2 expression was associated with tumor size but was not an independent prognostic factor for cancer-specific survival.
Recent evidences have suggested that COX-2 contributes to the inhibition of apoptosis.13 The possible mechanism of the COX-2 inhibition of apoptosis involves the generation of prostaglandin products or the removal of the substrate arachidonic acid via COX-2 catalytic activity.28,29
p53 is a known inducer of apoptosis, and its prognostic significance for RCC remains controversial. 20-23 In the current study, the p53 expression significantly correlated with the TNM stage, M stage, and metastasis (synchronous or metachronous). The survival rate of patients with p53-positive tumors was significantly lower than that of patients with p53-negative tumors. The p53 expression, together with tumor size and M stage, was an independent prognostic factor for cancer-specific survival according to the results of the multivariate analysis conducted in this study. However, p53 positivity did not significantly associate with the COX-2 overexpression, and that was in harmony with the results of Miyata et al.18 that the COX-2 expression did not correlate with the apoptotic index.
In conclusion, the increased expression of p53 was associated with metastasis and a worse prognosis in the conventional RCC, which suggested that p53 might have played an important role in the progression of the conventional RCC. However, the increased expression of the COX-2 was only associated with tumor size, but may not be an important prognostic factor in the conventional RCC. There was no association between the COX-2 overexpression and p53 positivity in the conventional RCC.
Figures and Tables
Fig. 1
Immunohistochemical staining for COX-2. (A) COX-2 immunostaining was not seen (COX-2 intensity, 0). (B) Almost all cancer cell cytoplasms strongly stained for COX-2 (COX-2 intensity, 3). Original magnification, ×400.

Fig. 2
Immunohistochemical staining for p53. (A) Tumor cells showed no nuclear staining for p53 (p53 negative). (B) A strong nuclear expression of p53 was seen (p53 positive). Original magnification, ×400.

Fig. 3
Kaplan-Meier cancer-specific survival curves according to the p53 expression. The survival rate of patients with p53-positive tumors was significantly lower than that of patients with p53-negative tumors (p<0.0001).
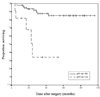
Fig. 4
Kaplan-Meier cancer-specific survival curves according to the COX-2 expression. There was no difference in survival rates according to the level of the COX-2 expression (p=0.7506). Weak, scores 0 - 4; moderate, scores 5-8; strong, scores 9-12.

References
1. Chow WH, Devesa SS, Warren JL, Fraumeni JF Jr. Rising incidence of renal cell cancer in the United States. JAMA. 1999. 281:1628–1631.
2. Delahunt B. Histopathologic prognostic indicators for renal cell carcinoma. Semin Diagn Pathol. 1998. 15:68–76.
3. Yasunaga Y, Shin M, Miki T, Okuyama A, Aozasa K. Prognostic factors of renal cell carcinoma: a multivariate analysis. J Surg Oncol. 1998. 68:11–18.
4. Vane JR, Bakhle YS, Botting RM. Cyclooxygenases 1 and 2. Annu Rev Pharmacol Toxicol. 1998. 38:97–120.
5. Herschman HR. Prostaglandin synthase 2. Biochim Biophys Acta. 1996. 1299:125–140.
6. Masunaga R, Kohno H, Dhar DK, Ohno S, Shibakita M, Kinugasa S, et al. Cyclooxygenase-2 expression correlates with tumor neovascularization and prognosis in human colorectal carcinoma patients. Clin Cancer Res. 2000. 6:4064–4068.
7. Joo YE, Rew JS, Seo YH, Choi SK, Kim YJ, Park CS, et al. Cyclooxygenase-2 overexpression correlates with vascular endothelial growth factor expression and tumor angiogenesis in gastric cancer. J Clin Gastroenterol. 2003. 37:28–33.
8. Denkert C, Winzer KJ, Müller BM, Weichert W, Pest S, Köbel M, et al. Elevated expression of cyclooxgenase-2 is a negative prognostic factor for disease free survival and overall survival in patients with breast carcinoma. Cancer. 2003. 97:2978–2987.
9. Chen YJ, Wang LS, Wang PH, Lai CR, Yen MS, Ng HT, et al. High cyclooxygenase-2 expression in cervical adenocarcinomas. Gynecol Oncol. 2003. 88:379–385.
10. Khuri FR, Wu H, Lee JJ, Kemp BL, Lotan R, Lippman SM, et al. Cyclooxygenase-2 overexpression is a marker of poor prognosis in stage I non-small cell lung cancer. Clin Cancer Res. 2001. 7:861–867.
11. Yoshimura R, Sano H, Masuda C, Kawamura M, Tsubouchi Y, Chargui J, et al. Expression of cyclooxygenase-2 in prostate carcinoma. Cancer. 2000. 89:589–596.
12. Shirahama T. Cyclooxygenase-2 expression is up-regulated in transitional cell carcinoma and its preneoplastic lesions in the human urinary bladder. Clin Cancer Res. 2000. 6:2424–2430.
13. Cao Y, Prescott SM. Many actions of cyclooxygenase-2 in cellular dynamics and in cancer. J Cell Physiol. 2002. 190:279–286.
14. Williams CS, Mann M, DuBois RN. The role of cyclooxygenases in inflammation, cancer, and development. Oncogene. 1999. 18:7908–7916.
15. Pruthi RS, Derksen E, Gaston K. Cyclooxygenase-2 as a potential target in the prevention and treatment of genitourinary tumors: a review. J Urol. 2003. 169:2352–2359.
16. Khan KN, Stanfield KM, Trajkovic D, Knapp DW. Expression of cyclooxygenase-2 in canine renal cell carcinoma. Vet Pathol. 2001. 38:116–119.
17. Okamoto T, Hara A, Hino O. Down-regulation of cyclooxygenase-2 expression but up-regulation of cyclooxygenase-1 in renal carcinomas of the Eker (TSC2 gene mutant) rat model. Cancer Sci. 2003. 94:22–25.
18. Miyata Y, Koga S, Kanda S, Nishikido M, Hayashi T, Kanetake H. Expression of cyclooxygenase-2 in renal cell carcinoma: correlation with tumor cell proliferation, apoptosis, angiogenesis, expression of matrix metalloproteinase-2, and survival. Clin Cancer Res. 2003. 9:1741–1749.
19. Yoshimura R, Matsuyama M, Kawahito Y, Tsuchida K, Kuratsukuri K, Takemoto Y, et al. Study of cyclooxygenase-2 in renal cell carcinoma. Int J Mol Med. 2004. 13:229–233.
20. Girgin C, Tarhan H, Hekimgil M, Sezer A, Gürel G. p53 mutations and other prognostic factors of renal cell carcinoma. Urol Int. 2001. 66:78–83.
21. Uchida T, Gao JP, Wang C, Jiang SX, Muramoto M, Satoh T, et al. Clinical significance of p53, mdm2, and bcl-2 proteins in renal cell carcinoma. Urology. 2002. 59:615–620.
22. Papadopoulos I, Rudolph P, Weichert-Jacobsen K. Value of p53 expression, cellular proliferation, and DNA content as prognostic indicators in renal cell carcinoma. Eur Urol. 1997. 32:110–117.
23. Hofmockel G, Wittmann A, Dammrich J, Bassukas ID. Expression of p53 and bcl-2 in primary locally confined renal cell carcinomas: no evidence for prognostic significance. Anticancer Res. 1996. 16:3807–3811.
24. Guinan P, Sobin LH, Algaba F, Badellino F, Kameyama S, MacLennan G, et al. TNM staging of renal cell carcinoma: Workgroup No. 3. Union Internationale Contre le Cancer (UICC) and the American Joint Committee on Cancer (AJCC). Cancer. 1997. 80:992–993.
25. Fuhrman SA, Lasky LC, Limas C. Prognostic significance of morphologic parameters in renal cell carcinoma. Am J Surg Pathol. 1982. 6:655–663.
26. Sinicrope FA, Ruan SB, Cleary KR, Stephens LC, Lee JJ, Levin B. bcl-2 and p53 oncoprotein expression during colorectal tumorigenesis. Cancer Res. 1995. 55:237–241.
27. Hara S, Kondo Y, Matsuzawa I, Hashimoto Y, Kimura G, Akimoto M, et al. Expression of cyclooxygenase-2 in human bladder and renal cell carcinoma. Adv Exp Med Biol. 2002. 507:123–126.
28. Sheng H, Shao J, Morrow JD, Beauchamp RD, DuBois RN. Modulation of apoptosis and Bcl-2 expression by prostaglandin E2 in human colon cancer cells. Cancer Res. 1998. 58:362–366.
29. Chan TA, Morin PJ, Vogelstein B, Kinzler KW. Mechanisms underlying nonsteroidal antiinflammatory drug-mediated apoptosis. Proc Natl Acad Sci USA. 1998. 95:681–686.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download