Abstract
Materials and Methods
The MRI findings of 17 confirmed cases of non-infectious ischiogluteal bursitis were analyzed: four out of the 17 cases were confirmed with surgery, and the remaining 13 cases were confirmed with MRI plus the clinical data.
Results
The enlarged bursae were located deep to the gluteus muscles and postero-inferior to the ischial tuberosity. The superior ends of the bursal sacs abutted to the infero-medial aspect of the ischial tuberosity. The signal intensity within the enlarged bursa on T1-weighted image (WI) was hypo-intense in three cases (3/17, 17.6%), iso-intense in 10 cases (10/17, 58.9%), and hyper-intense in four cases (4/17, 23.5%) in comparison to that of surrounding muscles. The bursal sac appeared homogeneous in 13 patients (13/17, 76.5%) and heterogeneous in the remaining four patients (4/17, 23.5%) on T1-WI. On T2-WI, the bursa was hyper-intense in all cases (17/17, 100%); it was heterogeneous in 10 cases and homogeneous in seven cases. The heterogeneity was variable depending on the degree of the blood-fluid levels and the septae within the bursae. With contrast enhancement, the inner wall of the bursae was smooth (5/17 cases), and irregular (12/17 cases) because of the synovial proliferation and septation.
Ischiogluteal bursitis, so called "weaver's bottom", is an uncommon disorder nowadays, and it is often overlooked as a cause of buttock pain (1). This malady may cause a radiating pain running down the posterior thigh, and then the diagnosis of ischiogluteal bursitis can be overlooked since these symptoms are often mistaken as a referred pain due to some pathology of the spine (2-4). The pain and impaired ambulation that are due to ischiogluteal bursitis, and especially in the elderly, can drastically effect the sufferers' sense of well-being and general health (4). In addition, ischiogluteal bursitis may result in a misplaced clinical diagnosis as arthritis, or as a peri-rectal mass or neoplasm, especially when the buttock pain occurs in those patients with known malignancies (5-8). In these challenging clinical situations, MRI is the imaging modality of choice. To the best of our knowledge, a clinical study on the MRI findings of ischiogluteal bursitis has not been reported in the literature, although there are reports on the ultrasound findings (9), and there are brief mentioning of the CT (5, 8-10) and MRI findings (6, 9, 11).
It could be helpful for radiologists, and certainly for the younger doctors, to know the MRI findings of ischiogluteal bursitis as a cause of the buttock pain or mass. They can then confidently provide information to the referring physicians who are not aware of ischiogluteal bursitis and are often frustrated about isolating the cause of the buttock pain, thereby delaying the proper treatment for their patients.
We collected 41 MRI studies on patients with abnormal findings in vicinity of the ischial tuberosity from a total of 768 MRI studies of the hip region that were done during the proceeding eight years. The medical records of these 41 patients were thoroughly scrutinized to ascertain that no pathologies other than ischiogluteal bursitis had been identified. Among them, we first excluded 14 patients because the cause of their buttock pain was originating from primary or secondary neoplasms of soft tissue or bone, hematomas, abscesses and cellulitis on both the MRI findings and clinical data, which included the surgical findings. Second, ten more patients were excluded when their medical records could not clarify that the buttock pain was caused by either ischiogluteal bursitis or spinal diseases because they had not been completely evaluated clinically and radiologically.
Our study group was finally composed of 17 cases of ischiogluteal bursitis (six cases on the right side and 11 on the left side) in 17 patients (12 women and five men; range: 50-82 years; average: 63.8 years). None of our cases had bilateral involvement. Four out of the 17 confirmed cases were proven at surgery and on histopathologic studies. The reasons for surgery in these four patients were the clinical uncertainties in differentiating bursitis from a buttock neoplasm in one patient, and there was no improvement with conservative treatment in the remaining three patients. The remaining 13 out of the 17 cases were confirmed by clinical data and when oral N-SAIDs (non-steroidal anti-inflammatory drugs) for 2-4 weeks alleviated the symptoms on the clinical follow-up that was at least one month or longer. Among these 13 patients, four of the patients underwent percutaneous needle aspiration of the bursa before or during treatment, and serosanguinous or bloody fluid was obtained.
The duration of symptoms in the 17 patients ranged from three weeks to six months (average duration: 1.9 months). The patients could not recall any traumatic episodes that preceded their discomfort, although they might have had an unnoticed minor injury during some recent activities. One of the 17 patients had a history of uterine cervical cancer that had been surgically treated three years previously.
Radiographs in all the 17 confirmed cases showed there were no abnormalities at the ischial tuberosity and adjacent soft tissue.
The MRI examinations were ordered by physicians to exclude the possibility of neoplasm with buttock pain (9/17, 53%), for defining the cause of the buttock pain only (5/17, 30%), and for investigating the cause of buttock pain as referred pain to the posterior thigh (3/17, 17%). For these last three patients with posterior thigh pain, the etiology was proven to be related to ischiogluteal bursitis and not to the spine when MRI was performed on both the spine and buttock.
MRI studies were carried out using four MRI units: the MRI studies were performed for five cases with either a 1.5 T Signa or Horizon system, (GE Medical Systems, Milwaukee, Wis); MRI studies were performed for two cases with a 0.5 T Gyroscan system (Philips Medical Systems, Einthoven, Netherlands), and MRI studies were performed for ten cases with a 1.5 T Magnetom Vision system (Siemens, Erlangen, Germany). With the GE and Siemens units, we obtained images with the fast spin-echo technique, and the spin-echo technique was used with the Philips unit. The MRI protocol included T1-weighted images (TR/TE, 400-700/11-15) and T2-weighted images (TR/TE, 2000-4600/90-110) in the axial, coronal and sagittal planes. A body coil was used for the Signa unit, and a pelvic phased array coil was used for the Horizon unit; a dedicated BWA (body wrap around) coil was used for the Gyroscan unit and a dedicated C-P (circular polarized) body array coil was used for the Magnetom Vision unit. The studies were performed with a 20-40 cm field-of-view, 6-10 mm slice thickness, 0.5-1 mm intersection gap and a 256×256 or 256×512 matrix depending on the MRI unit that was used. Contrastenhanced T1-weighted studies (TR/TE, 400-1025/11-12) were subsequently performed using a standard dose (0.1 mmole per kilogram of body weight) of gadopentetate dimeglumine (Magnevist®; Schering, Berlin, Germany).
The MR images were retrospectively reviewed by four experienced musculoskelectal radiologists (K.H.C., S.M.L., Y.H.L., K.J.S.) working together, and these physicians were not aware of the clinical history for each patient. A consensus was obtained in all the cases, except for the one case that was confirmed as ruptured bursitis upon surgery. We analyzed the location of the bursa and its anatomical relationship to the ischial tuberosity and hamstring tendon, the size of the enlarged bursa, the characteristics of the signal intensity of the bursal contents, the bursal wall and the peri-bursal soft tissues.
All the enlarged bursae, except the one case that ruptured, were located deep to the inferior portion of the gluteus maximus muscle and posterioinferiorly to the ischial tuberosity on the sagittal sections. On the transverse and coronal sections, the superior end of the bursa abutted to the inferomedial surface of the ischial tuberosity, and it was medial to the common tendon of the hamstring muscles that originates from the inferolateral surface of the ischial tuberosisty (Fig. 1).
The size of the enlarged bursa in 16 cases (the one bursa that ruptured was excluded from the size measurements) variably ranged from the smallest, 1.5×2.5×2.5 cm to the largest, 8×6×2 cm (average size: 4.7×3.8×1.6 cm) for the anterior-posterior, transverse and cephalo-caudal diameters.
On the T1-weighted images, the signal intensity within the bursa was hypo-intense in three patients (3/17, 17.6%), iso-intense in 10 patients (10/17, 58.9%), and hyper-intense in four patients (4/17, 23.5%) compared to that of the adjacent muscle. On the T1-weighted images, the signal intensity within the bursa was homogeneous in 13 patients (13/17, 76.5%) and heterogeneous in four patients (4/17, 23.5%).
On the T2-weighted images, the bursa was hyper-intense in all patients (17/17, 100%; heterogeneously hyper-intense in 10 cases and homogenously hyper-intense in 7 cases). This heterogeneity was variable depending on the degree of the blood-fluid levels and septations within the bursae (Fig. 2).
The bursal wall was not discernable on both the T1- and T2-weighted images. On the contrast enhancement studies, the bursal wall, intra-bursal septation(s) and synovial proliferaltion were positively enhanced with variable thickness. The inner wall was smooth in five cases, and the walls were irregular in 12 cases because of synovial proliferation.
In four patients, the enlarged bursa extended into the subcutaneous fat at the ischiorectal fossa, beyond the imaginary line that can be drawn between the medial ends of the gluteus maximus and adductor magnus muscles on the transverse sections. In two patients, inflammation in the peri-bursal soft tissues was more observed as the signal aberration increased.
The three patients having referred pain to their posterior thigh had variable findings. For the one patient that had the ruptured bursitis, the fluid had diffusely flowed into the soft tissues of the posterior buttock around the ischial tuberosity. This case was positively confirmed as ruptured bursitis upon surgery (Fig. 3). The second patient who had referred pain to the posterior thigh improved after the surgical removal of the ischiogluteal bursa. In the remaining third patient, the radiating pain was relieved after needle aspiration was performed under ultrasound-guidance.
Buttock pain in the elderly may be related to a variety of pathologies that are found around the hip, including osteoarthritis, avascular necrosis of the femoral head, stress or occult fracture, vascular insufficiency, metastasis and various soft tissue diseases that involve the nerve, muscle, bursa and supporting connective tissues (4, 12). In addition, this pain can be caused by diseases that may spread to and from the hip area, the thigh, pelvis, retroperitoneum and the spine, as the hip region serves as the bridge and conduit between the trunk and lower limb (1).
Inflammation of the ischiogluteal bursa has been known to be common in people whose occupations are related with frequent irritation to the bursa, and this irritation can occur during long periods of time spent in the sitting position. When vibration is involved in working, such as with heavy powered sewing machine (weavers), tractor-driving or road equipment machines, the ischiogluteal bursa can become inflamed (2, 3). It can also be affected by an acute or chronic shearing force on the ischial tuberosity caused by falling on his or her backsides (buttocks) in athletes, resulting in chronic and sometimes disabling discomfort that can prevent athletes from participating in their sporting activities (13). There are many sports that involve sitting such as canoeing, horseback riding, wheel-chair racing for paraplegic patients and so on. Besides that, as the ischial tuberosity bears the weight of the body in the supine position, these pressure points may lead to ischiogluteal burisitis in debilitated persons, and particularly for those patients with malignancies or paraplegia (7, 14).
Although there are no specific radiographic findings that are diagnostic of ischiogluteal bursitis, the most common findings in a long-standing case would be irregularity of the cortex of the ipsilateral ischial tuberosity, or any calcification projecting over or near the tuberosity (10).
Radiological evaluation is helpful to the physician when the clinical diagnosis is obscured for patients having buttock pain and/or a mass. When imaging is indicated for the diagnosis, MRI and/or ultrasound is the first choice of modality. There are at least two advantages for using MRI in this situation. The first is that MRI provides a global view for finding causative lesions of buttock pain or a mass in the pelvis, hip, and soft tissue, or for excluding the possibility of spinal diseases. The second is that the T2-weighted images clearly identify and localize the inflamed bursa according to the characteristic MRI findings of bursitis at the expected location (13).
The MRI findings of ischiogluteal bursitis may be similar to other inflamed bursae that arise in other regions of the body. However, the internal signal intensity of ischiogluteal bursitis is usually brighter than that of other bursitis observed elsewhere. The reason for this high signal intensity on the T1-weighted image of this affected bursal sac is due probably to the internal hemorrhage caused by the shearing force applied to the ischial tuberosisty area when sitting, and this hemorrhage is aggravated by frequent irritation. The heterogeneity on the T2-weighted and contrast studies is probably related to bleeding, synovial proliferation and the internal septation within the bursa.
It is imperative to differentiate ischiogluteal bursitis from peri-rectal or buttock abscess, hematoma, epidermoid cyst, dermoid cyst or hydatid cyst when the lesion shows a cystic appearance. The typical location of ischiogluteal bursitis might be a very important diagnostic criterion for separating bursitis from the other cystic masses. The common hamstring tendon is typically located lateral to the inflamed ischiogluteal bursa, and it possibly acts as a barrier to prevent the extension of the bursitis. Instead, the enlarged bursa usually spreads inferomedially to the ischiorectal fossa, according to our experience.
Ischiogluteal bursitis, when it occurs in cancer patients, it may clinically mimic a soft-tissue or bone metastasis from the primary malignancy (7, 8). Whenever the possibility of tumor is in the differential diagnosis, biopsy or surgical intervention should be performed for confirmation. In addition, an enlarged bursa should be aspirated to exclude an infectious process whenever this is suspected.
Tuberculosis, gout, rheumatoid arthritis, systemic lupus erythematosus, ankylosing spondylitis and Reiter's syndrome have also been reported to involve the ischiogluteal bursa (2-8, 10, 15, 16).
Although there are reports mentioning that the ischiogluteal bursa is one of the typical sites involved in tuberculosis (10, 17), we did not experience any cases of tuberculous ischiogluteal bursitis in our study.
Intra-bursal proliferation of the synovia can present as a solid mass, and it's necessary to radiologically differentiate this condition from other solid forms of synovitis such as pigmented villo-nodular synovitis, and on rare occasions from the synovial neoplastic lesions such as non-calcified synovial chondromatosis, synovial hemangioma, lipoma and synovial sarcoma.
The pain from ischiogluteal bursitis can be excruciating; patients have characterized it as "sharp and shooting", and it may radiate down the back of the leg. Because the enlarged bursa may extend to compress the sciatic nerve and/or the nearby posterior cutaneous nerve of the thigh, then referred pain can arise (1-3, 5, 7). In addition, the peri-bursal inflammation may extend and irritate the nerves with a resulting neural sign. The pain from ischiogluteal bursitis should also be differentiated from that in pyriformis syndrome as the nerves emerge out from under the pyriformis muscle in the upper gluteal area (18).
The interpretation of the MRI findings is made more difficult when the bursa ruptures. Because the ruptured bursa deflates, it can insinuate along the tissue planes of the buttock and its relatively toxic content spreads to the posterior thigh or across the hamstring tendon laterally to the sciatic nerve: the resulting inflammatory changes make the correct diagnosis difficult. As long as the bursa is not ruptured, or if it is not markedly enlarged to the point of compressing the nerves, posterior thigh pain will probably not arise.
We recognize that there are several limitations in our study: (1) not all the cases were surgically confirmed because bursitis can usually be treated conservatively; (2) the cause of the radiating pain could not be precisely proven; (3) we did not correlate the high signal intensity of the bursal content to the internal hemorrhage by pathology or needle aspiration in all the cases; and (4) we had a limited number of subjects.
In conclusion, ischiogluteal bursitis can be diagnosed with MRI by the characteristic anatomical location abutting to the medial aspect of the inferoposterior surface of the ischial tuberosity, and by its cystic appearance with a tendency for an intra-bursal blood-fluid level(s). However, care must be taken for differentiating this lesion from perianal abscesses, hematomata, and solid buttock masses. Needle aspiration, biopsy or surgery is essential whenever infection or neoplasm is to be excluded from the diagnosis. For the patients with referred pain, MRI of the spine is also a mandatory procedure.
Figures and Tables
Fig. 1
Ischiogluteal bursitis in 68-year-old woman.
A. T1-weighted image: a hypo-intense mass (arrow) in comparison with that of the adjacent muscle is seen at the soft tissue just posterior to the ischial tuberosity.
B. T2-weighted image: a hyper-intense mass (arrow) at the ischial tuberosity.
C. Contrast-enhanced T1-weighted image: the bursal wall is enhanced hyper-intensely at the ischial tuberosity (arrow). The bursa extends medially to the ischial tuberosity.
D. T2-weighted image on the coronal section shows a homogeneously hyper-intense mass (arrow) at the ischial tuberosity. The enlarged bursa extends inferiorly and medially to the inferior surface of the ischial tuberosity.

Fig. 2
Ischiogluteal bursitis in 71-year-old man.
A. The T1-weighted axial image shows a heterogeneously hyper-intense mass with multiple fluid-blood levels within it (arrows).
B. The T2-weighted axial image shows the multiple fluid-blood levels (arrows).
C. The Contrast-enhanced fat-suppressed T1-weighted image shows the discernable wall of the enlarged bursa; multiple fluid-blood levels are seen within it, like that observed on Fig.1A and B (arrows).
D. The T1-weighted image on sagittal section shows fluid-blood levels within the enlarged bursa that is located between the inferoposterior surface of the ischial tuberosity and the gluteus muscle (arrows).
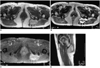
Fig. 3
Ischiogluteal bursitis that is ruptured and caused adjacent soft tissue inflammation in a 72-year-old-woman.
A. The T1-weighted axial section shows that the soft tissue posterior to the ischial tuberosity (arrows) is diffusely iso-intense or slightly hyper-intense in comparison with that of the muscle.
B. The T2-weighted axial section shows no enlarged bursa, but there is diffusely increased signal intensity of the soft tissue in the vicinity of the ischial tuberosity (arrows). The high signal intensity is extending across the hamstring tendon onto the sciatic nerve. This patient had a referred pain to the posterior thigh.
C. The fat-suppressed contrast-enhanced T1-weighted image shows diffuse soft tissue enhancement at and along the ischial tuberosity in the left buttock area (arrows).

References
1. Cho KH, Park BH, Yeon KM. Ultrasound of the adult hip. Semin Ultrasound CT MR. 2000. 21:214–230.
2. Swartout R, Compere EL. Ischiogluteal bursitis. The pain in the arse. JAMA. 1974. 227:551–552.
3. Larsson LG, Baum J. The syndromes of bursitis. Bull Rheum Dis. 1986. 36:1–8.
4. Schon L, Zuckerman JD. Hip pain in the elderly: evaluation and diagnosis. Geriatrics. 1988. 43:48–62.
5. Garcia-Porrua C, Gonzales-Gay MA, Corredoira J, Vazquez-Caruncho M. Hip pain. Ann Rheum Dis. 1999. 58:148–149.
6. Lambie P, Kaufman R, Beardmore T. Septic ischial bursitis in systemic lupus erythematous presenting as a perirectal mass. J Rheumatol. 1989. 16:1497–1499.
7. Mills GM, Baethge BA. Ischiogluteal bursitis in cancer patients: an infrequently recognized cause of pain. Am J Clin Oncol. 1993. 16:229–231.
8. Volk M, Gmeinwieser J, Hanika H, Manke C, Strotzer M. Ischiogluteal bursitis mimiking soft-tissue metastasis from a renal cell carcinoma. Eur Radiol. 1997. 8:1140–1141.
9. Kim SM, Shin MJ, Kim KS, et al. Imaging features of ischial bursitis with an emphasis on ultrasonography. Skeletal Radiol. 2002. 31:631–636.
10. Chafetz N, Genant HK, Hoaglund FT. Ischiogluteal tuberculous bursitis with progressive bony destruction. J Can Assoc Radiol. 1982. 33:119–120.
11. De Paulis F, Cancchio A, Michelini O, Damiani A, Saggini R. Sports injuries in the pelvis and hip: diagnostic imaging. Eur J Radiol. 1998. 27:Suppl 1. S49–S59.
12. Murtagh J. Hip and buttock pain in adults. Aust Fam Physician. 1992. 21:848–853.
13. Berquist TH. Berquist TH, editor. Imaging of sports injuries. 1992. Gaithersburg, Maryland: Aspen Publishers;93–94.
14. Rubayi S, Montgomerie JZ. Septic ischial bursitis in patients with spinal cord injury. Paraplegia. 1992. 30:200–203.
15. Anderson CR. Weaver's bottom[letter to the editor]. JAMA. 1974. 228:565.
16. Crenshaw AH Jr. Canale ST, editor. Non-traumatic disorders. Campbell's operative orthopedics. 1998. 9th ed. St. Louis: Mosby;782–783.
17. Resnick D, Niwayama G. Resnick D, editor. Osteomyelitis, septic arthritis, and soft tissue infection: organisms. Diagnosis of bone and joint disorders. 2002. 4th ed. Philadelphia: Saunders;2510–2624.
18. Trommer PR. Weaver's bottom [letter to the editor]. JAMA. 1974. 228:566.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download