Abstract
Objective
To evaluate the usefulness of newly designed sheaths for gastroduodenal intervention in a gastric phantom and dogs.
Materials and Methods
A regular sheath was made using a polytetrafluoroethylene tube (4 mm in diameter, 90 cm long) with a bent tip (4 cm long, 100 degree angle). For the supported type of sheath, a 5 Fr catheter was attached to a regular sheath to act as a side lumen. To evaluate their supportability, we measured the distance of movement of the sheath's tip within a silicone gastric phantom for three types of sheath, the regular type, supported type, and supported type with a supporting guide wire. The experiments were repeated 30 times, and the results were analyzed using ANOVA with the postHoc test.
In addition, an animal experiment was performed in six mongrel dogs (total: 12 sessions) to evaluate the torque and supportability of the sheaths in the stomach, while pushing a guide wire or coil catheter under fluoroscopic guidance.
Results
In the guide wire application, the distances of movement of the sheath tip in the three types of sheath, the regular type, supported type, and supported type with supporting guide wire, were 8.40±0.51 cm, 6.23±0.41 cm, and 4.47±0.32 cm, respectively (p < 0.001). In the coil catheter application, the corresponding values were 7.22±0.70 cm, 5.61±0.31 cm and 3.91±0.59 cm, respectively (p < 0.001).
All three types of sheath rotated smoothly and enabled both the wires and catheters to be guided toward the pylorus of the dog in all cases.
Gastric outlet strictures are the second most commonly treated enteric strictures (1). Strictures are caused by malignancy or benign diseases such as pyloro-antral scarring resulting from a long-standing peptic disease or stenosis at the anastomotic site after surgery. Recently, self-expandable metallic stents have been used for the palliative treatment of inoperable malignant gastric and duodenal obstructions (2-5). Direct balloon dilatation of the stenotic pylorus has been relatively successful for the relief of outlet obstruction symptoms (6-11). However, some technical problems occur during the placement of a stent or balloon dilatation for the treatment of gastric outlet obstructions. The combination of a massively dilated, flaccid stomach and a narrow, tortuous or scarred pylorus may make the passage through the stricture extremely difficult (6). For intubation, angiographic catheters are generally used, but torque control is poor in this case, because catheters buckle in a capacious stomach. De Baere et al. reported technical failure in one out of 10 patients, and Pinto also reported that there was a need for gastrostomy access in one out of 6 patients undergoing gastroduodenal stent placement (5, 12). In such cases, endoscopic assistance is initially used to pass a guide wire through the stricture (7, 8).
To overcome these problems, we designed and created new types of sheath. These sheaths enabled a guide wire or catheter to be introduced into the pylorus, in order to provide support within the capacious stomach. The purpose of this study was to evaluate the usefulness of the newly designed sheaths for gastroduodenal intervention by experimenting in a phantom and dogs.
Two types of sheaths were designed, namely the regular and supported types (Fig. 1). The regular type of sheath was made of polytetrafluoroethylene (PTFE, Sang-A Flontec Co. Ltd., Incheon, Korea) tube, 90 cm in length with a 4 mm outer diameter and a 3 mm inner diameter. The length of the sheath was decided after consideration of the optimum working length and the distance between the incisor and the esophagogastric junction. The diameter and thickness of the sheath were decided after consideration of the physical properties of the PTFE tube. The distal end of the regular sheath was bent using a heat-gun, creating a bend that was 4 cm long with an angle of curvature of 100 degrees. A radiopaque ring was attached to the outer surface of the distal end of the sheath for the purpose of providing easy detection during fluoroscopic guidance. In order to fabricate the supported sheath, a 5 Fr catheter catheter was attached to a regular sheath to act as the side lumen for the passage of a 0.035-inch wire designed to support the sheath on the other side of the bent tip, parallel to the long axis. The supporting wire in the side lumen can be pushed against the greater curvature of the gastric wall, while supporting the sheath and keeping it oriented toward the pylorus.
To draw the outline of the stomach, the distance from the greater curvature of the stomach to the lesser curvature was measured on each section of an abdominal CT (Somatom Plus IV, Siemens, Erlangen, Germany) scan taken after the ingestion of one liter of contrast media (slice thickness = 1 cm) in a patient in whom the gastric outlet was not obstructed. The distances from the location of the greater curvature on one section of the CT scan to the same location on the lower and upper sections were also measured. Both the distances from the greater to the lesser curvature and the location of the greater curvature on one section relative to that on the next section were plotted on a 2-dimensional plane, and the contour of the greater and lesser curvature of the stomach was drawn by connecting these points on a 2-dimensional plane (Fig. 2A). The esophageal outline was drawn from the distal portion of the esophagus to the cardia, with a diameter of 2 cm and a length of 5 cm. Clay was shaped so as to have a thickness of 2 cm, in order to produce the gastric contour with a tubular shape at the esophageal portion, and it was then put into a molding flask made of acryl plate (Atoglas, Elf Atochem Korea Ltd., Seoul, Korea) (Fig. 2B). The molding flask was then filled with silicone, and the hardening process was performed. The clay in the gastric and esophageal portion was removed from the hardened silicone, and the exposed side of the silicone was covered with a lucent acryl plate. The cavity between the acryl plate and the hardened silicone having the shape of a stomach was used as the gastric phantom. PTFE tube, with an outer diameter of 3 mm and a length of 10 cm, having a blind distal end, was attached to the gastric phantom, so as to act as the duodenal and pyloric portions of the stomach.
The ability of the newly designed sheaths to change the direction of the guide wire or coil catheter from parallel to transverse to the esophageal portion, and to guide it toward the pyloric portion was evaluated, while the wire or coil catheter was advanced to the duodenal portion beyond the pyloric portion of the phantom. The ability of the sheath to prevent the guide wire and coil catheter from being pushed toward the greater curvature was also evaluated. Once the sheath was inserted into the gastric portion via the esophageal portion, the location of the sheath's tip, without any force being applied to the sheath or guide wire, was chosen as the central point. The inner circle, which was surrounded by concentric circles drawn at intervals of 0.5 cm in order to act as a scale, corresponded to the tip of the sheath. A 0.038-inch guide wire (Radiofocus, Terumo Corporation, Tokyo, Japan) was advanced to the pyloric and duodenal portions through the sheath. When the guide wire was continuously pushed toward the blind end of the duodenal portion, it reached a point where it did not advance any further, whereupon it sloped down toward the greater curvature. Subsequently, the tip of the sheath was displaced away from the central point and toward the curved guide wire. Pushing was stopped when the curved guide wire contacted the greater curvature of the phantom, in order to prevent bias due to differences in the pushing force. The distance between the central point and tip of the sheath was measured. This experiment was repeated 30 times using both the regular and supported types of sheath.
With the supported sheath, an additional experiment was performed, and this involved advancing a supporting wire through the side lumen. A supporting wire with a diameter of 0.035-inches was inserted into the stomach portion through the side lumen and the tip was located at the blind end of the duodenal portion. When the wire was pushed, it advanced against the greater curvature side of the gastric phantom, and the distal portion of the sheath was propelled toward the pyloric portion. The distance of movement of the tip of the supported sheath, from the central point to its final location, was measured, while pushing both the guide and supporting wires (Figs. 3A, B).
The statistical significance of the differences between the distance of movement of the tip of the sheath in the regular and supported sheaths, with and without the supporting wire, was evaluated by means of the ANOVA postHoc test. The same experiment was repeatedly performed, while pushing both the guide wire and coil catheter, which was custom-made at this institution for the purpose of gastroduodenal intervention. The coil catheter was made of a stainless steel coil and a heat-compressive tube (1.3 mm in internal diamenter, 2.5 mm in external diameter and 90 cm in length) (13) (Figs. 4A, B).
All experimental procedures were performed in accordance with the National Institutes of Health guidelines for the humane handing of animals and approved by the committee for animal research at our institution.
Twelve experimental sessions were performed in six mongrel dogs, in order to evaluate the torque and support-ability of the sheath in the stomach, while pushing a guide wire or a coil catheter under fluoroscopic guidance (Fig. 5). For general anesthesia, the dogs were premedicated intramuscularly with ketamine hydrochloride (20 mg/kg, Yuhan Pharmacy, Seoul, Korea) and atropine sulfate (0.5 mg, Daewon Pharmacy, Seoul, Korea). General anesthesia was maintained by an intravenous infusion of ketamine hydrochloride (1-2 mg/kg/min). The dogs were restrained on the fluoroscopic unit (MCA-901 High-End Surgical C-arm, Medison, Seoul, Korea), and a gag was put in their mouth. After the advancement of the 0.038-inch-diameter guide wire into the stomach, a regular sheath coated with lubricating jelly was pushed into the stomach over the guide wire. The sheath was then rotated, so that the tip moved in a direction which was away from the greater curvature of the body and toward the pylorus in the stomach, in order to evaluate the torque and, finally, a wire or coil catheter was pushed toward the pylorus to evaluate the supportability of the sheath. The same experiment was performed again for the supported sheath, with and without a supporting wire in the side lumen.
The dogs were sacrificed after the second session of experiments for the purpose of evaluating possible injuries caused by the sheaths, including hemorrhage or rupture of the esophagus or stomach.
The newly designed sheaths easily changed the direction of the guide wire or coil catheter from the longitudinal direction of the esophageal portion to the transverse direction. The sheaths successfully guided the tip toward the pyloric portion, with the simultaneous advancement of the wire or coil catheter toward the duodenal portion past the pyloric portion of the phantom, for both the regular and supported types. In the experiments designed to evaluate the supportability of the sheaths when the guide wire was advanced toward the greater curvature, the distance of movement of the tip from the central point was the shortest in the case of the supported sheath combined with a supporting wire situated in the side lumen (4.47±0.32 cm). The distance of movement of the supported sheaths without a supporting wire (6.23±0.41 cm) was shorter than that of the regular sheaths (8.40±0.51 cm). The differences among the different types of sheath were statistically significant (p < 0.001). According to the data obtained by pushing a coil catheter showed that the distance of movement was the shortest in the supported sheath combined with a supporting wire in the side lumen (3.91±0.59 cm), followed by the supported sheath without a supporting wire (5.61±0.31 cm) and the regular sheath (7.22±0.70 cm). The differences among the different types of sheath were statistically significant (p < 0.001) (Table 1).
In the experiment designed to evaluate the torque, the sheaths were smoothly rotated within the stomach, regardless of the type of sheath or the insertion or not of a supporting wire, in all 12 sessions for the six dogs. When the guide wire and coil catheter were pushed through the sheath, their direction was changed from the long axis of the esophagus to the transverse axis oriented toward the pylorus in the stomach, and the shape of the sheath was well maintained without straightening. The guide wire and coil catheter were easily advanced to the duodenum beyond the pylorus, for all types of sheath with and without a supporting wire. No kinking or buckling of the guide wire or coil catheter occurred in the stomach of any of the dogs.
The experiments were well tolerated by the dogs, and no procedure related complications occurred, such as massive bleeding or perforation of the esophagus or stomach. There was no definitive evidence of rupture or gross hemorrhage in the esophagus or stomach on the pathologic specimens.
Balloon dilatation and placement of a metallic stent have been used for the palliative treatment of strictures involving the gastric outlet. Controlled balloon dilatation relieves the symptoms of gastric stasis due to scarring resulting from long-standing peptic ulcers, and may also permit normal or near-normal oral intake in patients for whom surgery is impossible. In the majority of patients with strictures which developed after gastric surgery, their symptoms are relieved with a single balloon dilatation (6, 9). The placement of a metallic stent is feasible and effective for the palliative treatment of inoperable malignant gastroduodenal obstructions (2, 4, 5, 12). Depending on the anatomy, either a variable straight or curved angiographic catheter can be used, in combination with a torque-control guide wire, in order to traverse the strictures during gastroduodenal intervention. However, an angiographic catheter is often too soft to pass directly through the stricture effectively, and torque control is often poor when the catheter buckles within a capacious stomach. In patients having a massively dilated stomach with a narrow and tortuous stricture, intubation is extremely difficult (7, 12). Moreover, the denudation of the hydrophilic coating of the guide wire caused by gastric acid makes it extremely difficult to advance a catheter with a 5 F-diameter over the guide wire across the stricture.
To overcome these technical problems, various methods have been introduced and used. McLean et al. (6, 7) used large-bore small bowel intubation tubes directed by a thick heavy-duty torque cable and direct manual palpation of the dilated stomach. However, in cases of chronic obstruction, there was often no "back wall" to work against and attempts to use heavy guide wires, external pressure with a leaded glove or other methods, were frequently unsuccessful and sometimes proved to be extremely frustrating. Alternatively, access to the stomach can be achieved with percutaneous gastrostomy by using standard techniques (3, 5, 12). A combination of endoscopic and fluoroscopic guidance has also been used to facilitate both the catheterization of the stenosis and accurate device deployment (5,
7, 14).
The new sheaths were designed for the purpose of performing gastroduodenal intervention, under fluoroscopic guidance only, without gastrostomy, especially in situations where endoscopic assistance is unavailable. The sheaths were designed and made from PTFE tube following consideration of its physical characteristics, given that a PTFE tube with an outer diameter of 4 mm and a thickness of 0.5 mm has a suitable stiffness. The sheaths were strong enough to protect the guide wire or coil catheter against the parallel force of the long axis of the esophagus and to direct the wire or coil catheter toward the greater curvature of the antrum. The distal end, which was bent at an angle of 100 degrees over a length of 4 cm, was effective in changing the direction of the guide wire or coil catheter from the parallel longitudinal direction of the esophageal portion to the transverse direction and guiding it toward the pyloric portion. In the case of the supporting sheath, the side lumen reinforced the ability of the sheath to support in the absence of the supporting wire, as revealed in the experiments using a gastric phantom. When a supporting wire was inserted into the side lumen of the supported type of sheath, it provided additional supporting force to the sheath. This ability to support the guide wire and coil catheter were helpful for the easy selection of the pyloric canal and for the advancement of the guide wire and coil catheter toward the duodenum beyond the pylorus in all dogs. The new sheaths were also found to have sufficient torque, and were helpful for the introduction of the guide wire and coil catheter into the pylorus of the stomach.
Although the gastric phantom was useful for the quantitative analysis of the support provided by the sheath as the guide wire or coil catheter was pushed through it, there were two limitations to this method. The first was that the gastric phantom was manufactured by measuring the size of the stomach in one patient on a CT scan, since the size and configuration of the stomach on the CT scans performed for several patients were too variable for them to be averaged. Since the ability of the sheath to support and guide the coil catheter depends on the size and configuration of the stomach, further evaluation is needed in gastric phantoms with various configurations. The second limitation was that the three-dimensional vector of the force in the human stomach was not reflected in our results, because the phantom was manufactured with a two-dimensional construction. In addition, the limitation in the animal experiment was that we could not evaluate the discomfort caused by the insertion of the sheath through the esophagus and its manipulation in the stomach. Although no injury to the esophagus or stomach was seen in the autopsy of the animals, further evaluation is needed in a clinical study.
In conclusion, these newly designed sheaths seem to be useful for increasing the success rate, by preventing failure of intubation into the pyloric canal and by augmenting the performance of interventional procedures, without the necessity for endoscopic assistance or invasive percutaneous gastrostomy, in patients with obstruction of the gastric outlet.
Figures and Tables
Fig. 1
A regular sheath (left) and supported sheath with a supporting wire in the side lumen (right).
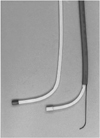
Fig. 2
A. An outline of the stomach was drawn, in order to make the gastric phantom, as follows. The distances from the greater to lesser curvature were measured in each section on the abdominal CT scan. The locations of the greater curvature on one section relative to that on the next section on the abdominal CT scan were also evaluated. Both the distances and relative locations were plotted on a 2-dimensional plane; subsequently, the contour of the greater and lesser curvature of the stomach was drawn by connecting these points on a 2-dimensional plane. The esophageal outline was drawn from the esophagus to the cardia, with a diameter of 2 cm and a length of 5 cm.
B. Clay was shaped, so as to be 2 cm in height, and to follow the gastric contour with a tubular shape at the esophageal portion.

Fig. 3
A. A guide wire is inserted in a supported sheath, and a supporting wire is inserted into the gastric portion through the side lumen. When the supporting wire is pushed, the tip of the wire is pressed against the greater curvature side of the gastric phantom.
B. The distance of movement of the tip of the supported sheath from the central point was measured while pushing the guide and supporting wire, and was found to be approximately 4 cm.

Fig. 4
A. A regular sheath is inserted into the gastric portion via the esophageal portion, and a coil catheter is advanced beyond the pyloric portion.
B. The distance between the central point and point of the tip of the sheath is approximately 6 cm.

Fig. 5
Experimental study in dogs. While pushing a coil catheter through the sheath, the direction is changed from the long axis of the esophagus to the transverse axis oriented toward the pylorus in the stomach. The coil catheter is then advanced to the pylorus with support from the sheath, without any kinking occurring in the stomach.

References
1. Lindor KD, Ott BJ, Hughes RW Jr. Balloon dilatation of upper digestive tract strictures. Gastroenterology. 1985. 89:545–548.
2. Jung GS, Song HY, Kang SG, et al. Malignant gastroduodenal obstructions: treatment by means of a covered expandable metallic stent-initial experience. Radiology. 2000. 216:758–763.
3. Song HY, Yang DH, Kuh JH, Choi KC. Obstructing cancer of the gastric antrum: palliative treatment with covered metallic stents. Radiology. 1993. 187:357–358.
4. Mauro MA, Koehler RE, Baron TH. Advances in gastrointestinal intervention: the treatment of gastroduodenal and colorectal obstructions with metallic stents. Radiology. 2000. 215:659–669.
5. Pinto IT. Malignant gastric and duodenal stenosis: palliation by peroral implantation of a self-expanding metallic stent. Cardiovasc Intervent Radiol. 1997. 20:431–434.
6. McLean GK, Meranze SG. Interventional radiologic management of enteric strictures. Radiology. 1989. 170:1049–1053.
7. McLean GK, Cooper GS, Hartz WH, Burke DR, Meranze SG. Radiologically guided balloon dilation of gastrointestinal strictures. Part I. Technique and factors influencing procedural success. Radiology. 1987. 165:35–40.
8. McLean GK, Cooper GS, Hartz WH, Burke DR, Meranze SG. Radiologically guided balloon dilation of gastrointestinal strictures. Part II. Results of long-term follow-up. Radiology. 1987. 165:41–43.
9. Holt PD, de Lange EE, Shaffer HA Jr. Strictures after gastric surgery: treatment with fluoroscopically guided balloon dilatation. AJR Am J Roentgenol. 1995. 164:895–899.
10. Hegedus V, Raaschou HO. Radiologically guided dilatation of stenotic gastroduodenal anastomosis. Gastrointest Radiol. 1986. 11:27–29.
11. Kozarek RA. Hydrostatic balloon dilation of gastrointestinal stenoses: a national survey. Gastrointest Endosc. 1986. 32:15–19.
12. de Baere T, Harry G, Ducreux M, et al. Self-expanding metallic stents as palliative treatment of malignant gastroduodenal stenosis. AJR Am J Roentgenol. 1997. 169:1079–1083.
13. Shin JH, He X, Lee JH, et al. Newly designed multifunctional coil catheter for gastrointestinal intervention: feasibility determined by experimental study in dogs. Invest Radiol. 2003. 38:796–801.
14. Binkert CA, Jost R, Steiner A, Zollikofer CL. Benign and malignant stenoses of the stomach and duodenum: treatment with self-expanding metallic endoprostheses. Radiology. 1996. 199:335–338.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download