Abstract
Objective
Materials and Methods
Results
Conclusion
Figures and Tables
Fig. 1

Fig. 2
Fig. 3
Fig. 4
Fig. 5
Table 1

Note.- *Others (n = 4): La Radiologia Medica (1), Pediatric Radiology (1), Ultraschall in der Medizin (1), Ultrasound in Medicine & Biology (1), †Others (n = 40): Annals of Academy of Medicine, Singapore (1), Alimentary Pharmacology & Therapeutics (1), American Journal of Clinical Oncology (1), American Journal of Obstetrics and Gynecology (1), Anticancer Research (1), Asian Journal of Surgery (1), Breast Cancer (1), Chinese Medical Journal (1), Collegium Antropologicum (1), Colorectal Disease (1), European Journal of Cardio-thoracic Surgery (1), European Journal of Gastroenterology & Hepatology (1), European Spine Journal (1), European Urology (1), Gastroentérologie Clinique et Biologique (1), Gynecologic Oncology (1), Hepatobiliary & Pancreatic Diseases International (1), Hong Kong Medical Journal (1), International Journal of Colorectal Disease (1), International Journal of Medical Sciences (1), International Orthopaedics (1), Japanese Journal of Clinical Oncology (1), Japanese Journal of Medicine (1), Journal of Clinical Oncology (1), Journal of Endourology (1), Journal of Gastrointestinal and Liver Diseases (1), Journal of Hepatology (1), Journal of Laparoendoscopic & Advanced Surgical Techniques (1), Journal of American Medical Association (1), Langenbeck's Archives of Surgery (1), Oncology Reports (1), Spine (1), Surgery (1), Surgical Laparoscopy, Endoscopy & Percutaneous Techniques (1), American Journal of Surgery (1), Breast (1), Cancer Journal (1), European Respiratory Journal (1), Kaohsiung Journal of Medical Sciences (1), Lancet Oncology (1)
Table 2
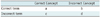
Note.- Correct concept means that definition of terminology meets reference standard for standardized terminology and reporting criteria. Correct term means term meets standardized terminology and reporting criteria. Accuracy of each term is based on formula: [a / (a + c)] × 100. We define column 'a' as accurate use of term accroding to proposed criteria. We define column 'c' as alternative term. As for column 'b', correct terms and incorrect concepts according to proposed criteria were identified in only 19 cases among all identified studies: incorrect concept of procedure or session (n = 1), treatment (n = 5), index tumor (n = 1), technical success (n = 3), primary technique effectiveness rate (n = 1), secondary technique effectiveness rate (n = 1), local tumor progression (n = 1), major complication (n = 3), and minor complication (n = 3). Column 'd' was not used in this study because of exclusion during selection of articles.
Table 5
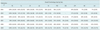
Note.- Data in parentheses represent number of articles in which terms were used without consideration of accuracy over total number of articles. There were no articles published in 2004 and 2005 that used secondary technique effectiveness rate. PS = procedure or session, Tx = treatment, IT = index tumor, AZ = ablation zone, TS = technical success, PTE = primary technique effectiveness rate, STE = secondary technique effectiveness rate, LTP = local tumor progression, MC = major complication, mC = minor complication
Table 6
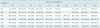
Note.- Data in parentheses represent number of articles in which terms were used accurately over number of articles in which concepts were applied accurately according to proposed criteria (refer to Table 2). There were no articles published in 2004 and 2005 that accurately used secondary technique effectiveness rate. PS = procedure or session, Tx = treatment, IT = index tumor, AZ = ablation zone, TS = technical success, PTE = primary technique effectiveness rate, STE = secondary technique effectiveness rate, LTP = local tumor progression, MC = major complication, mC = minor complication




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download