Abstract
Objective
The purpose of this study was to compare the results of different agents for bronchial artery embolization of hemoptysis.
Materials and Methods
From March 1992 to December 2006, a bronchial artery embolization was performed on 430 patients with hemoptysis. The patients were divided into three groups. Group 1 included 74 patients treated with a gelfoam particle (1×1×1 mm), while group 2 comprised of 205 patients treated with polyvinyl alcohol (PVA) at 355-500 µm, and group 3 included 151 patients treated with PVA at 500-710 µm. We categorized the results as technical and clinical successes, and also included the mid-term results. Retrospectively, the technical success was compared immediately after the procedure. The clinical success and mid-term results (percentage of patients who were free of hemoptysis) were compared at 1 and 12 months after the procedure, respectively.
Results
Neither the technical successes (group 1; 85%, 2; 85%, 3; 90%) nor the clinical successes (group 1; 72%, 2; 74%, 3; 71%) showed a significant difference among the 3 groups (p > 0.05). However, the mid-term results (group 1; 45%, 2; 63%, 3; 62%) and mid-term results excluding the recurrence from collateral vessels in each of the groups (group 1; 1 patient, 2; 4 patients, 3; 2 patients) showed that group 1 was lower than the other two groups (p < 0.05). No significant difference was discovered for the mid-term results between groups 2 and 3. Moreover, the same results not including incidences of recurrence from collateral vessels also showed no statistical significance between the two groups (p > 0.05).
Hemoptysis is a manifestation of pulmonary or tracheobronchial disease (1, 2). It is caused by chronic lung diseases such as pulmonary tuberculosis, chronic bronchitis, bronchiectasis, lung cancer, aspergillosis, and pneumoconiosis. In most cases, the amount of hemoptysis is small, and it subsides gradually without a need for treatment.
However, massive hemoptysis, defined as 300 to 600 ml per 24 hours, is a life-threatening condition with a reported mortality rate of 50 to 60% (1).
Bronchial artery embolization (BAE) has been proven as a good treatment method for a patient for whom a surgical procedure is not an option as well as for a patient needing palliative therapy requiring hemodynamic stabilization (2). However, 36 to 44% of patients who underwent successful BAE for hemoptysis reported recurrences during long-term follow-up (1, 2). Many studies have dealt with causes for the recurrence of hemoptysis, as well as underlying diseases or angiographic findings have been identified as the reasons (2-5). Nevertheless, a number of studies focused on embolic agents that have been relatively small and have consequently generated much debate.
The purpose of this study is to compare results of various embolic agents used in our hospital to treat hemoptysis and to select an embolic agent resulting in a more favorable outcome.
Because this study was retrospective, Institutional Review Board approval was not required. Prior to the procedure, written informed consent was obtained, in accordance with the Institutional Review Board policy.
From March 1992 to December 2006, 561 patients underwent BAE to treat hemoptysis in our hospital. Of these patients, 430 patients consisting of 246 males and 184 females ranging in age from 18 to 87 years old (mean age 56.7 years) were selected for the study by exclusion criteria. The exclusion criteria were the following: (i) no angiographic finding of hemoptysis on diagnostic bronchial angiography, (ii) embolization by other than gelfoam and PVA or by a combination of more than two embolic agents, (iii) loss during follow-up or inability to confirm recurrence of hemoptysis during 12 months after BAE.
Then, according to the embolic agents used, patients were divided into three groups: group 1 - BAE was performed with the SPONGOSTAN Standard gelfoam particle (1×1×1 mm) (Johnson & Johnson MEDICAL limited, Skipton, UK), group 2 - BAE was performed with Contour Emboli PVA (355-500 µm) (Boston Scientific, Natick, MA), and group 3 - BAE was performed with Contour Emboli PVA (500-710 µm) (Boston Scientific, Natick, MA).
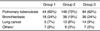
Group 1 had 74 patients, of whom 44 had hemoptysis due to pulmonary tuberculosis, 18 had bronchiectasis, five had lung cancer, and seven had other diseases (3 with pneumonia, 2 with lung abscesses, and 2 with pulmonary infarction). Group 2 consisted of 205 patients, of whom 148 had pulmonary tuberculosis, 38 had bronchiectasis, 13 had lung cancer, and six had other diseases (2 with pneumonia, 3 with lung abscesses, and 1 with coagulopathy due to coumadin medication). Among 151 patients in group 3, 94 had pulmonary tuberculosis as the cause of hemoptysis, 36 had bronchiectasis, 14 had lung cancer, and seven had other diseases (4 with pneumonia, 1 with a lung abscess, 1 with coagulopathy due to coumadin medication, and 1 with pulmonary infarction) (Table 1).
To detect bleeding sites prior to BAE, all the patients with hemoptysis underwent chest CT or bronchoscopy, and a diagnostic angiography was performed to confirm the bleeding site. Using the standard Seldinger technique, selective bronchial angiography was performed using a number of different 5-Fr catheters such as G.R.B & G.L.B (JUNG SUNG MEDICAL Co., Ltd., Seongnam, Korea) or Cobra (TERUMO®, Tokyo, Japan) to localize the site. In some cases from each group, there were bleeding sites of transpleural supplies from subclavian branches which included the internal mammary artery, lateral thoracic artery or other branches, bronchial arteries originating from the intercostobronchial trunk (31 patients in group 1, 71 patients in group 2, and 59 patients in group 3) (Fig. 1), or in some cases the anterior spinal artery was seen on angiography (2 patients in group 1, 3 patients in group 2, and 2 patients in group 3). The bleeding vessels were picked using 2 or 2.5 Fr Renegade (Boston scientific, Natick, USA) or Progreat™ (TERUMO®, Tokyo, Japan) microcatheters. We guided all vessels before the embolization, and any findings of hypervascularization, arterial enlargement, bronchial-pulmonary artery shunt, and extravasation for contrast material obtained from angiography were considered as evidence of the bleeding (Table 2). In addition, closed fluoroscopic observation was performed during the embolization to prevent other complications such as reflux into the anterior spinal artery. In each procedure, BAE was performed until the bleeding sites were no longer visible. Images from the arterial embolizations were captured by the Optimus DVI System and BV 5000 (Philips Healthcare, Best, The Netherlands).
Investigations of underlying diseases, embolic agents, and follow-ups were conducted by reviewing patient medical records or by telephone interview. If medical records indicated recurrence of hemoptysis, follow-ups were then terminated. Also, observations were concluded when no recurrence was observed within 12 months after BAE.
We defined technical success as a percentage of patients without a recurrence immediately after BAE. Clinical success was defined as a percentage of patients who hemoptysis-free for at least one month after the embolization, and the mid-term result was set as a percentage of patients who were free of hemoptysis 12 months after the procedure (6). Next, we assessed cumulative hemoptysis-free rates using the Cutler-Ederer method with SPSS version 12.0 (SPSS, Chicago, IL). P-values less than 0.05 were set as the threshold for statistical significance.
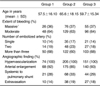
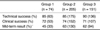
In group 1, 11 patients showed recurrence immediately after the BAE, and the technical success was 85% (63 of 74). After one month, 10 patients had recurrence in previously embolized vessels without collateral vessel origin, and the clinical success was 72% (53 of 74). Recurrence after 12 months was found in 20 patients, and the mid-term result was found to be 45% (33 of 74). Among them, 19 experienced recurrences in previously embolized vessels, while one was due to collateral bleeding.
In group 2, 30 patients showed hemoptysis immediately after the procedure, and technical success was calculated to be 85% (175 of 205). After one month, 23 patients experienced recurrence due to recanalization, and the clinical success was 74% (152 of 205). There was no bleeding focus in collaterals after one month; however, after 12 months, 22 patients had experienced a recurrence, and the mid-term result was 63% (130 of 205). Recurrence in previously embolized vessel was found in 18 patients, of whom four had collateral vessels.
In group 3, 15 patients showed recurrence of hemoptysis immediately after the procedure. As a result, the technical success rate was 90% (136 of 151). Recurrence occurred in 29 patients, in previously embolized vessels, and they had no collateral recurrence after one month. Hence, the clinical success was 71% (107 of 151) for group 3. After 12 months, a total of 13 patients had recurrence. Of these, 11 originated from the embolized vessels, whereas two originated from collateral vessels. The mid-term result was found to be 62% (94 of 151) (Table 3) (Fig. 2).
There were no significant differences among the three groups for the technical and clinical success rates (p > 0.05). However, group 1 showed a significantly lower mid-term result than the other groups. Significant differences for the mid-term results were found between groups 1 and 2 (p = 0.02) as well as groups 1 and 3 (p = 0.03).
Furthermore, for the mid-term results, when subtracting incidences of recurrence from collateral vessels in each group (group 1: 32 of 74, group 2: 126 of 205, group 3: 92 of 151), we found that group 1 also showed a significantly lower result than the other two groups (between groups 1 and 2: p = 0.03 and between groups 1 and 3: p = 0.04).
There were similar rates of technical failures among the three groups (group 1: 15%, group 2: 15%, group 3: 10%), and there had been no major procedure-related complications including spinal cord ischemia, non-target organ embolization, dysphagia, and so on.
From the moment Remy et al. (7) first performed BAE to treat hemoptysis, BAE has been used to treat both massive and chronic intermittent hemoptysis (8). BAE has also been used as a preoperative method to improve the lung function of patients prior to a surgery, and it is an effective hemostatic treatment modality in patients for whom surgery is not an option (7-10).
Therapeutic benefits of BAE in hemoptysis are diverse depending on the amount of bleeding, risk of recurrent hemoptysis, and overall lung function of patients (8). Among them, the risk of recurrent hemoptysis is a more important factor, especially in long-term recurrence. Moreover, the status of underlying diseases and characteristics of embolic agents may affect the risk of recurrent hemoptysis (6, 11).
Many embolic agents are used to perform BAE to treat hemoptysis, which include gelfoam and PVA. Each material has its own advantages and disadvantages. Gelfoam is cost-effective, and the size can be controlled. However, recanalization can occur faster than PVA, because gelfoam is absorbed spontaneously. PVA is a permanent material and can occlude a vessel at the small arteriolar level, but it results in collateral flow (12, 13).
In this study, we compared the relationship between clinical outcomes and embolic agents, especially PVA and gelfoam. We found that there was no significant difference in the results found among gelfoam and two PVA groups immediately after the procedure and after one month. However, PVA had better results than gelfoam after 12 months, regardless of particle size. No difference was found among these groups immediately after the embolization, which means that there was no difference in the rate of technical failure. Causes of technical failure include overlooking other bleeding sites, incomplete embolization, and so on (14). No significant difference was noted after one month also means that there was no difference in the temporary effect of BAE among the three embolic agent groups. However, a significant difference was found after 12 months; PVA had a better outcome than gelfoam in a setting of minimal progression of underlying diseases.
Many studies have dealt with the relationship between recurrent hemoptysis and embolic materials. However, they presented a controversy about which of gelfoam or PVA was the more effective embolic agent (15, 16). According to the report by Chung et al. (17), if an initially successful embolization was performed, the recurrence risk by gelfoam itself in previously embolized vessels was low, and hence there was no definite difference with other results, despite gelfoam being more absorbable in theory. Some authors also reported that there was no difference in the success rates among the various embolic agents (14, 18), and no difference in the results was noted among gelfoam and other non-absorbable agents (18). However in this study, under similar underlying disease conditions, technical failure, and the same follow-up period, we presented that PVA is superior for long-term outcomes in BAE, especially with the comparison among the mid-term results (except for the recurrence from collateral vessels), and provided a buttress for PVA in previous arguments about embolic efficacy.
The reason to establish a follow-up period to 12 months is to minimize the recurrence from collateral vessels. According to the report by Tanaka et al. (13), causes of recurrent hemoptysis include recanalization and reperfusion. Reperfusion is achieved by newly developed collateral vessels as underlying diseases progress with time (17). Thus, in our study, we set a follow-up period of 12 months to have a minimal impact on the recurrence risk from collateral vessels due to underlying diseases.
Many factors affected these results; because of the gelfoam particle's good absorbability, previously embolized vessels can recanalize earlier than in the case of PVA embolization. Therefore, rebleeding risk can increase with time. Also, the larger size of the gelfoam particles compared to PVA cannot occlude bleeding at the small arteriole level (16).
This study has several limitations. First, the maximum follow-up period was 12 months. Second, it was a retrospective analysis of patients from a single center. Finally, we did not compare the results to newer embolic materials such as embosphere, bead block, hepasphere, and others.
In conclusion, PVA is a better choice than gelfoam particle for BAE to improve the result, and it is considered that the material size of PVA needs to be selected to match the vascular diameter.
Figures and Tables
Fig. 1
39-year-old male with hemoptysis in right lower lobe.
A. Bronchial angiography showed bleeding from right bronchial artery which originated from intercostobronchial trunk.
B. After embolization with 2-Fr microcatheter, follow-up bronchial angiography showed no evidence of bleeding in right bronchial artery.

References
1. Mauro MA, Jaques PF. Baum S, Pentecost MJ, editors. Transcatheter bronchial artery embolization for inflammation (hemoptysis). Abrams' angiography. 1997. Boston: Little, Brown and Company;819–828.
2. Lee JM, Kwak HS, Han YM, Lee YK, Han HY, Kim CS. Bronchial arterial embolization for hemoptysis: analysis of outcome in various underlying causes. J Korean Radiol Soc. 1999. 41:45–53.
3. Kato A, Kudo S, Matsumoto K, Fukahori T, Shimizu T, Uchino A, et al. Bronchial artery embolization for hemoptysis due to benign diseases: immediate and long-term results. Cardiovasc Intervent Radiol. 2000. 23:351–357.
4. Hayakawa K, Tanaka F, Torizuka T, Mitsumori M, Okuno Y, Matsui A, et al. Bronchial artery embolization for hemoptysis: immediate and long-term results. Cardiovasc Intervent Radiol. 1992. 15:154–158.
5. Mal H, Rullon I, Mellot F, Brugière O, Sleiman C, Menu Y, et al. Immediate and long-term results of bronchial artery embolization for life-threatening hemoptysis. Chest. 1999. 115:996–1001.
6. Drooz AT, Lewis CA, Allen TE, Citron SJ, Cole PE, Freeman NJ, et al. Quality improvement guidelines for percutaneous transcatheter embolization. J Vasc Interv Radiol. 2003. 14:S237–S242.
7. Rémy J, Viosin C, Dupuis C, Beguery P, Tonnel AB, Denies JL, et al. Treatment of hemoptysis by embolization of the systemic circulation. Ann Radiol(Paris). 1974. 17:5–16. [French].
8. Kwon W, Kim YJ, Lee YH, Lee WY, Kim MS. The effectiveness of embolotherapy for treatment of hemoptysis in patients with varying severity of tuberculosis by assessment of chest radiography. Yonsei Med J. 2006. 47:377–383.
9. Ong TH, Eng P. Massive hemoptysis requiring intensive care. Intensive Care Med. 2003. 29:317–320.
10. Remy J, Jardin M. Dondelinger F, Rossi P, Kurdziel JC, editors. Angiographic management of bleeding. Interventional radiology. 1990. New York: Thieme;325–341.
11. Uflacker R, Kaemmerer A, Picon PD, Rizzon CF, Neves CM, Oliveira ES, et al. Bronchial artery embolization in the management of hemoptysis: technical aspects and long-term results. Radiology. 1985. 157:637–644.
12. Coldwell DM, Stokes KR, Yakes WF. Embolotherapy: agents, clinical applications, and techniques. Radiographics. 1994. 14:623–643.
13. Tanaka N, Yamakado K, Murashima S, Takeda K, Matsumura K, Nakagawa T, et al. Superselective bronchial artery embolization for hemoptysis with a coaxial microcatheter system. J Vasc Interv Radiol. 1997. 8:65–70.
14. Remy-Jardin M, Wattinne L, Remy J. Transcatheter occlusion of pulmonary arterial circulation and collateral supply: failures, incidents, and complications. Radiology. 1991. 180:699–705.
15. Mauro MA, Japques PF, Morris S. Bronchial artery embolization for control of hemoptysis. Semin Intervent Radiol. 1992. 9:45–51.
16. Fairfax AJ, Ball J, Batten JC, Heard BE. A pathological study following bronchial arterial embolization for haemoptysis in cystic fibrosis. Br J Dis Chest. 1980. 74:345–352.
17. Chung SK, Kim JK, Yoon W, Kim YH, Park JG, Kang HK. Bronchial artery and non-bronchial systemic artery embolization for the treatment in patients with hemoptysis: analysis of efficacy of Gelfoam single use. J Korean Radiol Soc. 2003. 49:15–22.
18. Kim EJ, Lim JW, Oh JH, Yoon Y, Sung DW. Prognostic factors in bronchial arterial embolization for hemoptysis. J Korean Radiol Soc. 1994. 31:43–48.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download