Abstract
Objective
To evaluate the incidence, predictive factors, and clinical outcomes of angiographically negative acute arterial upper and lower gastrointestinal (GI) bleeding.
Materials and Methods
From 2001 to 2008, 143 consecutive patients who underwent an angiography for acute arterial upper or lower GI bleeding were examined.
Results
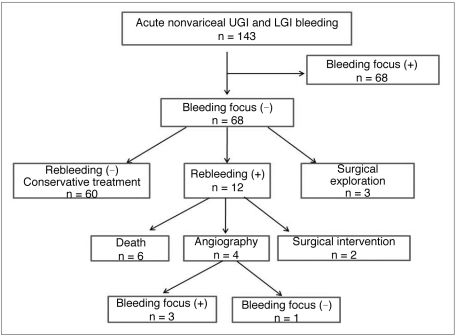
The angiographies revealed a negative bleeding focus in 75 of 143 (52%) patients. The incidence of an angiographically negative outcome was significantly higher in patients with a stable hemodynamic status (p < 0.001), or in patients with lower GI bleeding (p = 0.032). A follow-up of the 75 patients (range: 0-72 months, mean: 8 ± 14 months) revealed that 60 of the 75 (80%) patients with a negative bleeding focus underwent conservative management only, and acute bleeding was controlled without rebleeding. Three of the 75 (4%) patients underwent exploratory surgery due to prolonged bleeding; however, no bleeding focus was detected. Rebleeding occurred in 12 of 75 (16%) patients. Of these, six patients experienced massive rebleeding and died of disseminated intravascular coagulation within four to nine hours after the rebleeding episode. Four of the 16 patients underwent a repeat angiography and the two remaining patients underwent a surgical intervention to control the bleeding.
Acute gastrointestinal (GI) bleeding is a major cause of morbidity and mortality despite advances in therapeutic options (1). Mortality rates range from 8-14% in patients with acute GI bleeding (2-4), despite a medical or surgical treatment, and increases to 21-40% in cases of massive bleeding (5, 6).
Angiographic therapy plays an important role in the diagnosis and treatment of acute arterial GI bleeding. Angiographic therapy can detect and localize the bleeding focus; and, with embolization or vasopressin, the infusion can effectively stop acute bleeding (7-10).
The limitations of angiographic therapy include the inability to find and localize a bleeding focus when the rate of bleeding is slow or when active bleeding is not present at the moment the contrast material is injected. Because cases with intermittent bleeding or with a much lower bleeding rate are common in acute GI bleeding, the detection rate of bleeding sites by angiography are reported to vary widely from 24-78% (9, 11). However, little is known about the clinical outcome or natural history of patients with negative angiographic results. In the present study, we sought to evaluate the incidence, predictive factors, and clinical implications of angiographically negative acute arterial upper and lower GI bleeding.
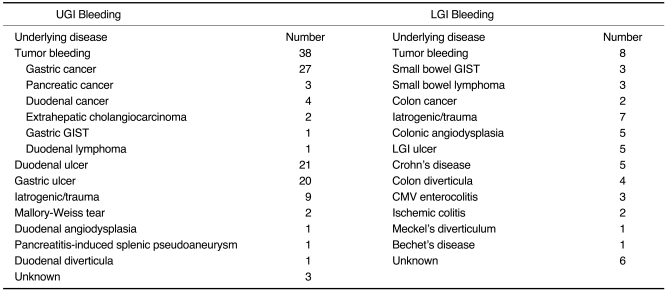
The study protocol was approved by our Institutional Review Board with a waiver of informed consent. We studied 143 consecutive patients (113 men, 30 women; mean age: 61 ± 13 years; age range: 18-88 years) with acute arterial upper or lower GI bleeding between February 2001 and October 2008. Upper or lower GI bleeding was diagnosed if its origin was located proximal or distal to the ligament of Treitz, respectively (1). All patients showed the symptoms related to an acute episode of GI bleeding (hematemesis, melena, or hematochezia) within six hours, which included changes in blood pressure, hemoglobin level, or pulse rate. In all patients, the endoscopic hemostasis had failed or was abandoned due to the inability to control bleeding. Upon admission, 50 of the 143 patients (35%) presented with hemodynamic instability (hypotension with systolic blood pressure < 90 mmHg) within six hours of an active bleeding episode. Multiple etiologies for arterial upper or lower GI bleeding are summarized in Table 1. The identification of causes and bleeding sites were achieved with an integrative evaluation, which included an endoscopy, CT, angiography, or a Technetium 99m (99m Tc)-labeled red blood cell (RBC) scintigraphy.
A 5 Fr angiographic catheter was introduced over a guide wire following the right or left common femoral artery puncture. To localize the bleeding sites, all patients underwent diagnostic angiograms of the celiac axis, superior mesenteric artery (SMA), and inferior mesenteric artery (IMA) via 5 Fr catheters. The sequence of diagnostic angiograms depended upon the location of the bleeding site. For instance, in lower GI bleeding, the SMA was studied first, followed by the IMA. If no bleeding site was found in the SMA or IMA distributions, the celiac artery was studied to determine if bleeding occurred in the upper GI origin. Twenty-five milliliters of contrast fluid was injected at a rate of 5 ml/s in the celiac artery, 30 ml at 5-6 ml/s in the SMA, and 15 ml at a rate of 3 ml/s in the IMA. In cases of a suspected bleeding area, a selective angiogram was performed using 2.0-2.4 Fr microcatheters (Progreat; Terumo, Tokyo, Japan). A direct angiographic sign of active GI bleeding was extravasation of the contrast medium, whereas indirect angiographic signs included a pseudoaneurysm and the cut-off of an artery.
Surgical treatment was selected if the patients showed continuous bleeding after a negative bleeding focus on the angiography or if the patients required surgical treatment as well as bleeding control.
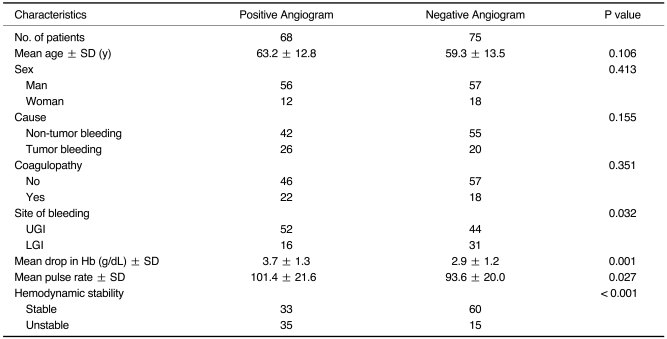
We retrospectively reviewed the records and/or images of patients who underwent an angiography and/or superselective embolization for acute arterial upper or lower GI bleeding. Patient data collection included age, sex, etiologies for acute bleeding, presence of coagulopathy, site of bleeding, and hemodynamic status (blood pressure, hemoglobin level, and pulse rate) upon admission (within 6 hours of an active bleeding episode). The differences in these factors were evaluated between patients with or without a bleeding focus. We evaluated the clinical outcomes of patients with angiographically negative results.
The student's t-test (parametric test) or Mann-Whitney U test (non-parametric test) was used to compare pairs of independent continuous variables including age, drop in hemoglobin level, and pulse rate. The Fisher's exact test was used to compare categorical variables including sex, cause (tumor bleeding versus non-tumor bleeding), presence of coagulopathy, site of bleeding (upper GI versus lower GI), and hemodynamic stability (stable; systolic blood pressure ≥ 90 mmHg versus unstable; systolic blood pressure < 90 mmHg). All statistical analyses were performed using the SPSS package (version 12.0; SPSS, Chicago, IL). A two-sided p value of less than 0.05 was considered to indicate statistical significance.
The angiographic therapy revealed a negative bleeding focus in 75 of the 143 (52%) patients. The incidence of an angiographically negative outcome was significantly higher in patients with stable hemodynamic status (60 of 93 cases; 65%) than in patients with unstable hemodynamic status (15 of 50 cases; 30%) (p < 0.001), or in patients with lower GI bleeding (31 of 47 cases; 66%) than in patients with upper GI bleeding (44 of 96 cases; 46%) (p = 0.032). In addition, a positive bleeding focus was correlated with a degree of drop in hemoglobin level (mean 2.9 g/dL in negative foci versus 3.7 g/dL in positive foci) (p = 0.001) and of elevation of pulse rate (mean of 93.6 for the negative foci versus 101.4 in the positive foci) with a statistical significance (p = 0.027). Conversely, age, sex, cause, and coagulopathy were not significantly correlated with a positive bleeding focus (Table 2).
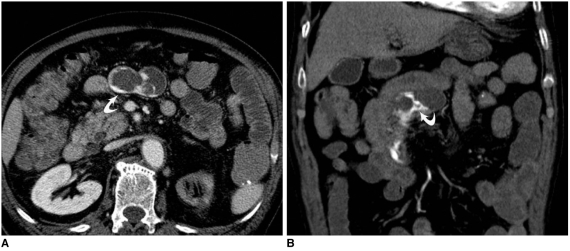
Of the 75 patients with no identified bleeding focus upon an initial angiography, 25 underwent a 99m Tc-labeled RBC scintigraphy. The majority of the patients who underwent the bleeding scan had lower GI bleeding (n = 21). Of these 25 patients, the bleeding scan found the bleeding focus in 12 patients (12 of 25; 48%) (Fig. 1). In addition, 20 of 75 patients with negative initial angiograms got through multidetector CT scans. Of the 20 patients, 11 had upper GI bleeding, whereas the remaining nine patients had lower GI bleeding. Of the 20 patients, CT scans identified the bleeding focus in four patients (20%) (Fig. 2).
The 75 patients with no identified bleeding focus upon initial angiographies were closely monitored over the course of an 8 month (± 14 months) follow-up period (range: 0-72 months) (Fig. 3). Three of the 75 (4%) patients underwent surgical exploration because of continuous bleeding; however, no bleeding focus was detected and the patients recovered without any further treatment. Sixty of the 75 (80%) patients underwent conservative management only, and the acute bleeding was controlled without rebleeding. Rebleeding occurred in 12 of 75 (16%) patients within 0-10 days (mean: 3 days) after the initial negative angiography. Six of the 16 patients experienced massive rebleeding and died within four to nine hours due to a disseminated intravascular coagulation. In addition, four of the 16 patients underwent an additional angiography. In three of the 16 patients, the bleeding focus was found and embolized. Lastly, one patient once again showed no bleeding focus and the condition was controlled with conservative management only. The two remaining patients with rebleeding underwent a surgical intervention. The rebleeding in one patient with advanced gastric cancer bleeding was controlled by a palliative antral resection with a gastrojejunostomy. The other patient with peptic duodenal ulcer bleeding was controlled by surgical ligation of the bleeding artery with closure of the perforated duodenum.
Acute arterial upper and lower GI bleeding remains a significant clinical challenge, often having poor outcomes irrespective of the multi-disciplinary treatments (11). Angiographic therapy and subsequent embolization is a successful first-line treatment of acute GI bleeding, which is refractory to endoscopic therapy (10). This approach is generally preferred over surgery, especially in high-risk patients (12-15).
To the best of our knowledge, no study has focused on the clinical outcome or natural history of patients with angiographically negative results. In the present study, we found that negative bleeding focus on angiography was relatively common (52%), which is within previously published ranges of negative bleeding focus (22-76%) (9, 11). Among the factors, which include age, sex, etiologies for acute bleeding, presence of coagulopathy, site of bleeding, and hemodynamic status, stable hemodynamic status (systolic blood pressure ≥ 90 mmHg) upon admission (p < 0.001) and lower GI bleeding (p = 0.032) were significant predictive factors for angiographically negative results. The majority of patients (60 of 75 cases; 80%) with a negative bleeding focus experienced spontaneous resolution of bleeding and therefore did not undergo surgical, endovascular, or endoscopic interventions during the follow-up.
In the present study, of the 75 patients with no identified bleeding focus upon an initial angiography, 25 patients underwent a 99m Tc-labeled RBC scintigraphy. The bleeding scan found the bleeding focus in 12 patients (12 of 25; 48%). Based on these results, the use of a 99m Tc-RBC scan in cases of negative angiographies for patients with intermittent or slow flow bleeding appears to be a reasonable way to help confirm and localize the bleeding (11).
The application of a contrast-enhanced CT for finding and localizing acute GI bleeding has received little attention. Recently, however, the multidetector CT has been an increasingly used modality in the diagnosis of vascular disease because of the much improved image resolution and decreased scanning time (16). The acquisition of accurate arterial phase images by a multidetector CT makes it possible for the identification of extravasation in contrast material into the intestinal lumen, a finding diagnostic of acute GI bleeding before the contrast material is diluted (1). A recent study (1) showed the high accuracy (98%) of the arterial phase multidetector CT for detection and localization of bleeding sites in patients with acute massive GI bleeding. In the present study, 20 of 75 patients with negative angiograms underwent a multidetector CT scan. Of the 20 patients, a bleeding focus was found in four patients (20%). Both the 99m Tc-RBC scan and multidetector CT scan may be helpful in detecting a bleeding focus in patients with a negative angiography. A more detailed study comparing the ability of the scanning modalities in finding the bleeding focus in patients with negative angiographies may be required.
In the present study, a positive bleeding focus was significantly more prevalent in patients with hemodynamic instability (systolic blood pressure < 90 mmHg) upon admission. Furthermore, a positive bleeding focus was correlated with a degree of drop in the hemoglobin level (mean 2.9 g/dL in negative focus versus 3.7 g/dL in positive focus) and the elevation of pulse rate (mean of 93.6 for the negative focus versus 101.4 for the positive focus). Reductions in blood counts, tachycardia, hypotension, and transfusion requirements have been postulated by many authors, with the goal of identifying ongoing blood loss (6, 17, 18). The careful evaluation of hemodynamic status in patients with acute GI bleeding is crucial because it is one of the most important predictive factors for the presence of a bleeding focus on angiography.
Another important predictive factor in identifying the presence of a bleeding focus in the present study was the location of the bleeding: lower GI bleeding was significantly related to a negative bleeding focus upon angiographic therapy. Because of the rich vascular anatomy of the upper GI tract, upper GI bleeding seems to be more massive than lower GI bleeding (11, 19). Furthermore, etiologies including the angiodysplasia, and ischemic or inflammatory lesions leading to low grade bleeding is more prevalent for lower GI bleeding (20, 21).
The rate of rebleeding in patients with angiographically negative bleeding focus occurred in 12 of 75 (16%) cases in the present study, which lies within the range of rebleeding rates (7-34%) after embolization for acute GI bleeding (10, 22-25). In addition, six patients from the current study that experienced massive rebleeding, died of disseminated intravascular coagulation soon after a rebleeding event. Despite the low rate of rebleeding after the initially negative angiographic results, the clinical outcome of rebleeding can be fatal, especially in patients with massive rebleeding. Therefore, a close follow-up of patients with an initial negative angiogram is crucial, especially within one or two weeks after initial angiography, as shown in the present study.
Moreover, three of the four patients who underwent a repeat angiography showed a positive bleeding focus and was treated by embolization. This observation suggests that a repeated angiography is necessary even after an initial finding of a negative bleeding focus, and should be performed as soon as possible for every episode of rebleeding.
The principal limitation of this study is its retrospective study design, which may decrease the study's statistical strength. For instance, the difference in time between the GI bleeding and angiography was not evaluated. Furthermore, the hemodynamic parameters just prior to the angiography were not evaluated. Although these limitations are significant, our study remains important in looking at the clinical outcome or natural history of patients with acute GI bleeding patients with negative angiographic results.
In conclusion, angiographically negative results are relatively common in patients with acute GI bleeding, especially in patients with a stable hemodynamic status or lower GI bleeding. The majority of patients with negative bleeding focus experienced a spontaneous resolution of the bleeding.
References
1. Yoon W, Jeong YY, Shin SS, Lim HS, Song SG, Jang NG, et al. Acute massive gastrointestinal bleeding: detection and localization with arterial phase multi-detector row helical CT. Radiology. 2006; 239:160–167. PMID: 16484350.

2. van Leerdam ME, Vreeburg EM, Rauws EA, Geraedts AA, Tijssen JG, Reitsma JB, et al. Acute upper GI bleeding: did anything change? Time trend analysis of incidence and outcome of acute upper GI bleeding between 1993/1994 and 2000. Am J Gastroenterol. 2003; 98:1494–1499. PMID: 12873568.
3. Prakash C, Zuckerman GR. Acute small bowel bleeding: a distinct entity with significantly different economic implications compared with GI bleeding from other locations. Gastrointest Endosc. 2003; 58:330–335. PMID: 14528203.
4. Sanders DS, Perry MJ, Jones SG, McFarlane E, Johnson AG, Gleeson DC, et al. Effectiveness of an upper-gastrointestinal hemorrhage unit: a prospective analysis of 900 consecutive cases using the Rockall score as a method of risk standardization. Eur J Gastroenterol Hepatol. 2004; 16:487–494. PMID: 15097042.
5. Leitman IM, Paull DE, Shires GT 3rd. Evaluation and management of massive lower gastrointestinal hemorrhage. Ann Surg. 1989; 209:175–180. PMID: 2783842.

6. Walsh RM, Anain P, Geisinger M, Vogt D, Mayes J, Grundfest-Broniatowski S, et al. Role of angiography and embolization for massive gastroduodenal hemorrhage. J Gastrointest Surg. 1999; 3:61–65. PMID: 10457326.

7. Abbas SM, Bissett IP, Holden A, Woodfield JC, Parry BR, Duncan D. Clinical variables associated with positive angiographic localization of lower gastrointestinal bleeding. ANZ J Surg. 2005; 75:953–957. PMID: 16336385.

8. Cynamon J, Atar E, Steiner A, Hoppenfeld BM, Jagust MB, Rosado M, et al. Catheter-induced vasospasm in the treatment of acute lower gastrointestinal bleeding. J Vasc Interv Radiol. 2003; 14:211–216. PMID: 12582189.

9. Hastings GS. Angiographic localization and transcatheter treatment of gastrointestinal bleeding. Radiographics. 2000; 20:1160–1168. PMID: 10903705.

10. Jae HJ, Chung JW, Jung AY, Lee W, Park JH. Transcatheter arterial embolization of nonvariceal upper gastrointestinal bleeding with N-butyl cyanoacrylate. Korean J Radiol. 2007; 8:48–56. PMID: 17277563.

11. Burke SJ, Golzarian J, Weldon D, Sun S. Nonvariceal upper gastrointestinal bleeding. Eur Radiol. 2007; 17:1714–1726. PMID: 17058080.

12. Dempsey DT, Burke DR, Reilly RS, McLean GK, Rosato EF. Angiography in poor-risk patients with massive nonvariceal upper gastrointestinal bleeding. Am J Surg. 1990; 159:282–286. PMID: 2305934.

13. Encarnacion CE, Kadir S, Beam CA, Payne CS. Gastrointestinal bleeding: treatment with gastrointestinal arterial embolization. Radiology. 1992; 183:505–508. PMID: 1561358.

14. Lang EV, Picus D, Marx MV, Hicks ME. Massive arterial hemorrhage from the stomach and lower esophagus: impact of embolotherapy on survival. Radiology. 1990; 177:249–252. PMID: 2399325.

15. Lang EK. Transcatheter embolization in management of hemorrhage from duodenal ulcer: long-term results and complications. Radiology. 1992; 182:703–707. PMID: 1535883.

16. Napoli A, Fleischmann D, Chan FP, Catalano C, Hellinger JC, Passariello R, et al. Computed tomography angiography: state-of-the-art imaging using multidetector-row technology. J Comput Assist Tomogr. 2004; 28:S32–S45. PMID: 15258492.
17. Koval G, Benner KG, Rosch J, Kozak BE. Aggressive angiographic diagnosis in acute lower gastrointestinal hemorrhage. Dig Dis Sci. 1987; 32:248–253. PMID: 3493124.

18. Nicholson AA, Ettles DF, Hartley JE, Curzon I, Lee PW, Duthie GS, et al. Transcatheter coil embolotherapy: a safe and effective option for major colonic hemorrhage. Gut. 1998; 43:79–84. PMID: 9771409.
19. Tan KK, Wong D, Sim R. Superselective embolization for lower gastrointestinal hemorrhage: an institutional review over 7 years. World J Surg. 2008; 32:2707–2715. PMID: 18843444.

20. Concha R, Amaro R, Barkin JS. Obscure gastrointestinal bleeding: diagnostic and therapeutic approach. J Clin Gastroenterol. 2007; 41:242–251. PMID: 17426461.
21. Barnacle AM, Aylwin AC, Jackson JE. Angiographic diagnosis of inflammatory bowel disease in patients presenting with gastrointestinal bleeding. AJR Am J Roentgenol. 2006; 187:976–985. PMID: 16985146.

22. Bandi R, Shetty PC, Sharma RP, Burke TH, Burke MW, Kastan D. Superselective arterial embolization for the treatment of lower gastrointestinal hemorrhage. J Vasc Interv Radiol. 2001; 12:1399–1405. PMID: 11742013.

23. Lee CW, Liu KL, Wang HP, Chen SJ, Tsang YM, Liu HM. Transcatheter arterial embolization of acute upper gastrointestinal tract bleeding with N-butyl-2-cyanoacrylate. J Vasc Interv Radiol. 2007; 18:209–216. PMID: 17327553.

24. Ripoll C, Bañares R, Beceiro I, Menchén P, Catalina MV, Echenagusia A, et al. Comparison of transcatheter arterial embolization and surgery for treatment of bleeding peptic ulcer after endoscopic treatment failure. J Vasc Interv Radiol. 2004; 15:447–450. PMID: 15126653.

25. Aina R, Oliva VL, Therasse E, Perreault P, Bui BT, Dufresne MP, et al. Arterial embolotherapy for upper gastrointestinal hemorrhage: outcome assessment. J Vasc Interv Radiol. 2001; 12:195–200. PMID: 11265883.

Fig. 1
77-year-old man with lower gastrointestinal bleeding due to unknown cause. Initial angiography showed no bleeding focus.
A. Following initial negative angiogram, rebleeding occurred. Degree of drop in hemoglobin level was 2.3 g/dL, however patient was hemodynamically stable. 99m Tc-red blood cell scintigraphy reveals active small bowel (jejunum) bleeding (arrows).
B. Patient underwent second angiography. Arteriogram shows contrast extravasation from proximal jejunal branch of superior mesenteric artery.
C. Final angiogram was performed after successful coil embolization.
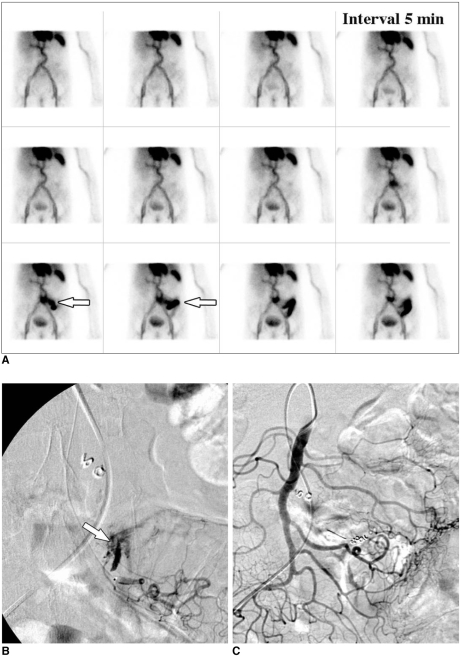
Fig. 2
80-year-old man with lower gastrointestinal bleeding due to unknown cause. Initial angiography showed no bleeding focus. Arterial phase axial (A) and coronal (B) multidetector CT scans help identify extravasation (curved arrows) of contrast material into proximal jejunal lumen, indicating active bleeding.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download