Abstract
Objective
To evaluate the clinical efficacy and safety of a transcatheter arterial embolization (TAE) with N-butyl cyanoacrylate (NBCA) for the treatment of arterial esophageal bleeding.
Materials and Methods
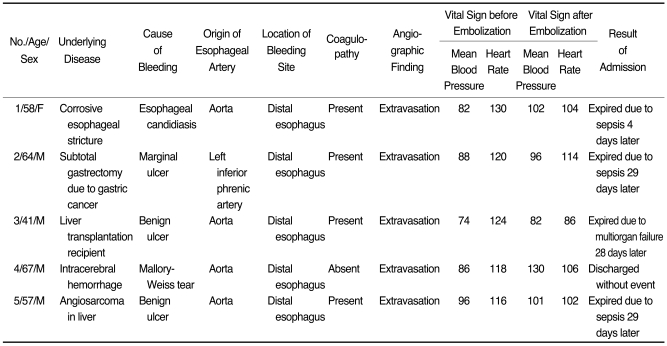
Between August 2000 and April 2008, five patients diagnosed with arterial esophageal bleeding by conventional angiography, CT-angiography or endoscopy, underwent a TAE with NBCA. We mixed NBCA with iodized oil at ratios of 1:1 to 1:4 to supply radiopacity and achieve a proper polymerization time. After embolization, we evaluated the angiographic and clinical success, recurrent bleeding, and procedure-related complications.
Results
The bleeding esophageal artery directly originated from the aorta in four patients and from the left inferior phrenic artery in one patient. Although four patients had an underlying coagulopathy at the time of the TAE, angiographic and clinical success was achieved in all five patients. In addition, no procedure-related complications such as esophageal infarction were observed during this study.
Arterial esophageal bleeding is a relatively uncommon cause of acute upper gastrointestinal hemorrhaging compared to bleeding caused by varices related to portal hypertension (1). The traditional first line of therapy for esophageal hemorrhaging is an endoscopy (1). However, with the advancement of technology, the transcatheter arterial embolization (TAE) has been an important and powerful treatment option for acute gastrointestinal hemorrhaging (2-4). Few case reports have described the treatment modalities for arterial bleeding of the esophagus and the use of various embolic materials such as gelatin sponges, microcoils and polyvinyl alcohol particles to embolize arterial esophageal bleeding (5-8). This is attributed to the reluctance of many practitioners to use such a tissue-adhesive, liquid embolic agent such as N-butyl cyanoacrylate (NBCA) to treat acute gastrointestinal hemorrhaging due to the concern of ischemic injury and the difficulty in handling the material. In this current study, we report the clinical efficacy and safety of TAE using NBCA for treatment of arterial esophageal bleeding.
Between July 2000 and June 2008, five patients underwent a TAE for treatment of arterial esophageal bleeding at our institution. The patients included four men and one woman, with an age range of 41-72 years (mean age, 59 years). Prior endoscopic treatment had failed in two patients and was not attempted in three patients because a skillful endoscopist was not available at that time or patients could not cooperate performing endoscopic treatment. We have described two of these cases in a previous report (9). Our Institutional Review Board approved this study, and patient informed consent was waived due to the retrospective nature of the study.
We used NBCA (Histoacryl; B. Braun, Melsungen, Germany) as an embolic agent in all five patients. The choice of NBCA as an embolic material in gastrointestinal bleeding patients has been common at our institution if we succeeded in the superselection of the small bleeding artery. We performed a diagnostic angiography to localize the bleeding site after a common femoral artery puncture. Our routine angiography protocol included a thoracic aortography and left gastric angiography. If we failed to show evidence of bleeding on aortography and left gastric angiography, we performed a selective angiography of the intercostal artery, bronchial artery, left inferior phrenic artery and tried to search for the esophageal artery directly from the aorta. After confirming the active bleeding, we advanced a 2.4-Fr tip microcatheter (Microferret; Cook, Bloomington, IN) or 2.0-Fr tip microcatheter (Progreat; Terumo, Tokyo, Japan) as close as possible into the bleeding esophageal artery. Next, we mixed NBCA with iodized oil (Lipiodol; Andre Guerbet, Aulnay-Sous-Bois, France) at ratios varying from 1:1 to 1:4. Prior to injection of the NBCA mixture, we flushed the microcatheter with a 5% dextrose solution to prevent premature polymerization of the mixture within the microcatheter. We injected the NBCA mixture using a 1 mL syringe under fluoroscopic monitoring. Next, we performed a post-embolization angiography to evaluate the effectiveness of the treatment.
We retrospectively evaluated the technical and clinical success, recurrent bleeding, procedure-related complications and clinical outcomes of each patient. We defined technical success as a successful superselection of the bleeding vessel and delivery of the NBCA mixture, as well as an angiography after embolization that showed no evidence of active bleeding (i.e., the presence of a pseudoaneurysm or extravasation of contrast agent). We defined clinical success as clinical improvement without evidence of bleeding for the next three days (i.e., clearing of the nasogastric aspirate and stabilization of the hemoglobin level). Patients who met one of the following criteria were considered to have coagulopathy: a prothrombin ratio greater than 1.5, a partial thromboplastin time greater than 45 seconds or a platelet count less than 80,000/µL (2, 10, 11).
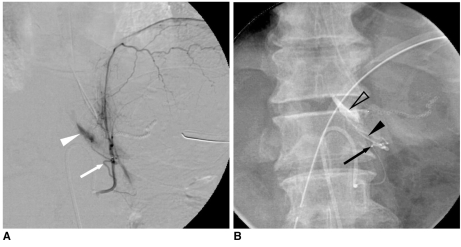
The clinical and angiographic data of the five patients are summarized in Table 1. We diagnosed four of the five patients with coagulopathy at the time of embolization. As well, four of five patients had bleeding esophageal arteries, which originated directly from the aorta (Fig. 1). The fifth patient (patient 2) had a bleeding esophageal artery that originated from the left inferior phrenic artery (Fig. 2). For all the five patients, the bleeding site was located at the distal esophagus. Further, the angiographic findings in all five patients indicated extravasation of contrast agent. Each patient showed clearing of the nasogastric aspirate and stabilization of the hemoglobin level without additional transfusion after embolization, and in turn achieved technical and clinical success. Further, there was no evidence of symptomatic esophageal infarction or other major complications directly related to NBCA embolization in any of the patients. One patient (patient 4) underwent a follow-up endoscopic evaluation five days after the embolization, and we found no esophageal ischemia. In spite of the successful embolizations, four patients expired during hospitalization due to other underlying conditions such as sepsis or multi-organ failure. The fifth patient recovered without further complications.
N-butyl cyanoacrylate starts to polymerize with the bonding of the ethylene units when exposed to anions such as the hydroxyl moieties in water or numerous anions present in blood. Because of its low viscosity, NBCA is easy to deliver through microcatheters even if the catheters have tortuous running pathways. Moreover, the lack of radiopacity and polymerization time when in contact with blood can be modified by the addition of an oily contrast medium such as Lipiodol (12, 13). This allows the operator to control the degree of distal vessel penetration as well as facilitate the occlusion at or significantly beyond the catheter tip. In effect, when blood velocity is low and the catheter tip cannot be placed near the locus of hemorrhaging, lowering the concentration NBCA and releasing it in a far proximity to the target may allow the intended goal to take effect. In turn, when blood velocity is high and the catheter tip can be placed near the locus of hemorrhaging, increasing the concentration of NBCA and releasing it in close proximity to the target, may also allow the intended goal to take effect. Furthermore, as the embolization time was significantly shorter in patients who received NBCA, compared to patients that did not receive the agent, this situation is advantageous to the operator in an urgent or emergency situation (14).
The arterial blood supply of the esophagus is divided into three parts. Primarily, the descending branches of the inferior thyroid artery supply the cervical esophagus. Branches of the bronchial arteries, and one or two esophageal arteries that arise directly from the aorta, supply the midthoracic portion. Lastly, branches of the left gastric or left inferior phrenic arteries supply the distal portion (6, 15). Interventional radiologists should be aware of variations in the arterial blood supply of the esophagus for a complete investigation of a bleeding focus. Branches of the subclavian, thyroidea ima, common carotid, or superior thyroid arteries may also supply the cervical esophagus. Branches of the right third or fourth intercostal arteries may also supply the midthoracic esophagus. Lastly, branches from the celiac, splenic, short gastric, or left hepatic arteries may supply the distal esophagus (6, 16).
The origins of previously embolized esophageal arteries varied and have included an esophageal branch that arose from the thoracic aorta (6, 8), an esophageal branch that arose from the right intercostal artery (7) and an esophageal branch that arose from the left gastric artery and inferior phrenic artery (5). In our study, the embolized esophageal branches originated from the aorta in four patients, and from the left inferior phrenic artery in one patient. Also, although all five patients had bleeding at the distal esophagus, there was no bleeding from the left gastric artery.
The various types of embolic materials used for the embolization of esophageal artery include gelatin sponge particles (5, 6), polyvinyl alcohol particles (7), and microcoils (8). As the esophageal arteries form collateral capillary networks before they penetrate the esophageal muscle layer and perfuse the submucosa (8), they can cause back bleeding (hemorrhaging from potential collateral channels) that is of concern. For this reason, in a case report on embolization of arterial esophageal bleeding with microcoils, Vogten et al. (8) catheterized another two esophageal branches after embolization just proximal and distal to the embolized branch. In our study, back bleeding from collateral channels did not occur. We believe that due to its liquid characteristics, NBCA can penetrate potential collateral channels and effectively embolize the channels with a single injection if properly mixed with oily contrast medium. Recently, NBCA has been used as an embolic agent in upper gastrointestinal bleeding patients with promising results (9, 17). In addition, Toyoda et al. (14) reported a significant reduction in the time of completion for a TAE with NBCA for the treatment of gastric or duodenal ulcer bleeding than TAE without NBCA. In a study of the embolization of acute upper gastrointestinal bleeding, Lee et al. (17) reported the practical application of controlling NBCA concentration when the bleeding artery could not be catheterized. They occluded the distal portion to the orifice of the bleeding vessel with a very slow injection rate of a higher concentration (40%) of NBCA. Next, the microcatheter was withdrawn to the proximal portion for continuous injection. If the catheter could not reach the distal portion of the orifice of the bleeding artery, 20-30% NBCA was injected at a proximal segment.
The diagnosis of coagulopathy in patients has been shown to adversely affect the success rate of embolotherapy in gastrointestinal bleeding, as well as an increase in the odds for clinical failure, which ranges from 2.9 to 19.46 (2, 10, 11). However, previous studies have reported that the use of NBCA was accompanied with a high angiographic and clinical success rate for cases of upper gastrointestinal bleeding in patients with coagulopathy (9, 17) since NBCA does not require the coagulation process for its effect. Similarly, although four of the five patients in our study had coagulopathy, we achieved technical and clinical success in all five case studies.
With the advancement of microcatheter and embolic agents, TAE quickly has become a safe and effective treatment for many cases of upper gastrointestinal bleeding (1, 9, 17). Although the first line therapy for esophageal hemorrhage is endoscopy (1), a TAE can be an alternative option for arterial esophageal bleeding when a skillful endoscopist is not available, endoscopic hemostasis fails, or patients could not cooperate to undergoing endoscopic treatment.
Our study has several limitations. First, the study population is so small because arterial esophageal bleeding is a very rare condition. Second, four patients died within one month after the embolization, due to various underlying disease.
In conclusion, we suggest that NBCA can be an effective and feasible embolic agent in patients with arterial esophageal bleeding, even in patients with coagulopathy. Patients with arterial esophageal bleeding should undergo a careful search for the esophageal branch that directly arises from the aorta.
References
1. Burke SJ, Golzarian J, Weldon D, Sun S. Nonvariceal upper gastrointestinal bleeding. Eur Radiol. 2007; 17:1714–1726. PMID: 17058080.

2. Schenker MP, Duszak R Jr, Soulen MC, Smith KP, Baum RA, Cope C, et al. Upper gastrointestinal hemorrhage and transcatheter embolotherapy: clinical and technical factors impacting success and survival. J Vasc Interv Radiol. 2001; 12:1263–1271. PMID: 11698624.

3. Kuo WT, Lee DE, Saad WE, Patel N, Sahler LG, Waldman DL. Superselective microcoil embolization for the treatment of lower gastrointestinal hemorrhage. J Vasc Interv Radiol. 2003; 14:1503–1509. PMID: 14654483.

4. Ripoll C, Bañares R, Beceiro I, Menchén P, Catalina MV, Echenagusia A, et al. Comparison of transcatheter arterial embolization and surgery for treatment of bleeding peptic ulcer after endoscopic treatment failure. J Vasc Interv Radiol. 2004; 15:447–450. PMID: 15126653.

5. Carsen GM, Casarella WJ, Spiegel RM. Transcatheter embolization for treatment of Mallory-Weiss tears of the esophagogastric junction. Radiology. 1978; 128:309–313. PMID: 307258.

6. Michal JA 3rd, Brody WR, Walter J, Wexler L. Transcatheter embolization of an esophageal artery for treatment of a bleeding esophageal ulcer. Radiology. 1980; 134:246. PMID: 6965326.

7. Kos X, Trotteur G, Dondelinger RF. Delayed esophageal hemorrhage caused by a metal stent: treatment with embolization. Cardiovasc Intervent Radiol. 1998; 21:428–430. PMID: 9853152.

8. Vogten JM, Overtoom TT, Lely RJ, Quispel R, de Vries JP. Superselective coil embolization of arterial esophageal hemorrhage. J Vasc Interv Radiol. 2007; 18:771–773. PMID: 17538140.

9. Jae HJ, Chung JW, Jung AY, Lee W, Park JH. Transcatheter arterial embolization of nonvariceal upper gastrointestinal bleeding with N-butyl cyanoacrylate. Korean J Radiol. 2007; 8:48–56. PMID: 17277563.

10. Encarnacion CE, Kadir S, Beam CA, Payne CS. Gastrointestinal bleeding: treatment with gastrointestinal arterial embolization. Radiology. 1992; 183:505–508. PMID: 1561358.

11. Aina R, Oliva VL, Therasse E, Perreault P, Bui BT, Dufresne MP, et al. Arterial embolotherapy for upper gastrointestinal hemorrhage: outcome assessment. J Vasc Interv Radiol. 2001; 12:195–200. PMID: 11265883.

12. Cromwell LD, Kerber CW. Modification of cyanoacrylate for therapeutic embolization: preliminary experience. AJR Am J Roentgenol. 1979; 132:799–801. PMID: 107749.

13. Stoesslein F, Ditscherlein G, Romaniuk PA. Experimental studies on new liquid embolization mixtures (histoacryl-lipiodol, histoacryl-panthopaque). Cardiovasc Intervent Radiol. 1982; 5:264–267. PMID: 6297733.

14. Toyoda H, Nakano S, Kumada T, Takeda I, Sugiyama K, Osada T, et al. Estimation of usefulness of N-butyl-2-cyanoacrylate-lipiodol mixture in transcatheter arterial embolization for urgent control of life-threatening massive bleeding from gastric or duodenal ulcer. J Gastroenterol Hepatol. 1996; 11:252–258. PMID: 8742922.

15. Swigart LL, Siekert RG, Hambley WC, Anson BJ. The esophageal arteries; an anatomic study of 150 specimens. Surg Gynecol Obstet. 1950; 90:234–243. PMID: 15401971.
16. Michels NA. Underlying blood supply and anatomy of the upper abdominal organs, with a descriptive atlas. 1955. Philadelphia: Lippincott;p. 266–270.
17. Lee CW, Liu KL, Wang HP, Chen SJ, Tsang YM, Liu HM. Transcatheter arterial embolization of acute upper gastrointestinal tract bleeding with N-butyl-2-cyanoacrylate. J Vasc Interv Radiol. 2007; 18:209–216. PMID: 17327553.

Fig. 1
41-year-old man (patient 3) presenting with arterial esophageal bleeding and underwent liver transplant 30 days prior.
A. Selective angiography of esophageal artery arising from descending thoracic aorta shows extravasation of contrast media (arrows) in distal esophagus.
B. Image obtained after embolization shows N-butyl cyanoacrylate and Lipiodol mixture in esophageal artery (arrow) and in lumen of esophagus (arrowhead).
C. Selective angiography of esophageal artery after performing embolization shows no evidence of extravasation of contrast media. Note subtraction artifact (arrow) caused by N-butyl cyanoacrylate and Lipiodol mixture in esophageal artery.
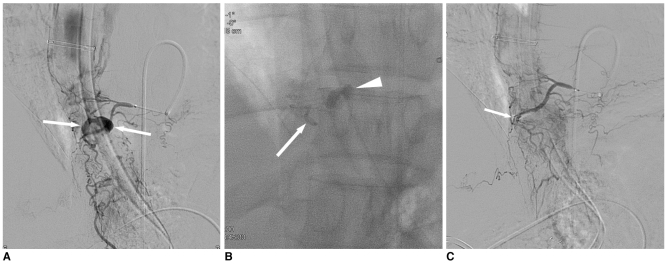
Fig. 2
64-year-old man (patient 2) with arterial esophageal bleeding that underwent subtotal gastrectomy 49 days prior.
A. Selective angiography of left inferior phrenic artery shows extravasation of contrast media (arrowhead) originating from esophageal branch (arrow).
B. Image during embolization shows N-butyl cyanoacrylate and Lipiodol mixture in esophageal artery (arrowhead) and in lumen of esophagus (open arrowhead). Note tip (arrow) of microcatheter in esophageal branch.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download