Abstract
Purpose
To compare early postoperative pain and visual outcomes after epipolis-laser in situ keratomileusis (epi-LASIK) and photorefractive keratectomy (PRK) in the treatment of myopia.
Methods
A retrospective chart review was designed and included 49 eyes in 30 patients who underwent epi-LASIK and 54 eyes in 29 patients who underwent PRK. During the early postoperative period (days 1 to 5), pain, uncorrected visual acuity (UCVA), and time to epithelial healing were recorded. Visual outcomes were followed for up to six months.
Results
Mean preoperative spherical equivalent refraction for the epi-LASIK group was -3.99±1.39 diopters (D) and that of the PRK group was -3.54±1.27 D. The pain scores on the fourth postoperative day were significantly higher in the epi-LASIK group than in the PRK group (p=0.017). Duration of pain in the epi-LASIK group was longer than in the PRK group (p=0.010). Mean healing time was significantly longer in the epi-LASIK group than in the PRK group (p<0.000). In addition, UCVA in the epi-LASIK group at postoperative days 1 and 3 were significantly lower than those in the PRK group (p=0.021 and p<0.000, respectively). Uncorrected visual acuity at one week and one month after epi-LASIK were lower than those after PRK (p=0.023 and p=0.004, respectively).
Conclusions
In the epi-LASIK patients, pain relief, corneal healing, and visual recovery seemed to be slower during the early postoperative period compared to those of the PRK patients. With longer duration of follow-up, however, there were no significant differences in visual outcome between the two groups.
Epipolis-laser in situ keratomileusis (epi-LASIK) is a new option for advanced surface ablation [1,2]. The procedure has some theoretical advantages over other surface ablation procedures. Preservation of the basement membrane of the epithelial flap probably acts as a barrier to prevent penetration of cytokines into the corneal stroma [3]. In addition, mechanical separation of the epithelial flap means that the use of toxic alcohol can be avoided [1,2]. Therefore, epi-LASIK should theoretically be associated with less pain and faster recovery than those of other procedures [1,4].
Some studies have reported that epi-LASIK is a safe and efficient method for correcting low-to-moderate myopia and myopic astigmatism [4-7]. However, there is some debate regarding postoperative pain after various procedures. Some studies have reported that epi-LASIK patients have similar or less postoperative pain than that suffered by patients undergoing other procedures, but only during the first two postoperative hours [7]. However, other reports claim that patients suffer more postoperative pain after epi-LASIK than after other procedures, and that most epithelial cells in the epithelial flap are dead when observed histologically, thereby leading to increased pain [8-10]. Our group previously showed that epi-LASIK and photorefractive keratectomy (PRK) were associated with similar levels of postoperative pain and visual acuity in a small group study (presented at the XXIV Congress of the European Society of Cataract & Refractive Surgeons, London, UK, September 2006). There have been few reports on postoperative pain during the first week after these procedures. Therefore, after including data from more patients, we again compare the pain and visual outcomes associated with epi-LASIK and PRK.
A retrospective chart review was designed in which records from all patients who underwent epi-LASIK or PRK at our institution between October 2005 and October 2007 were reviewed. Forty-nine eyes in 30 patients who underwent epi-LASIK and 54 eyes in 29 patients who underwent PRK were included. The inclusion criteria were myopia characterized by spherical equivalents less than 6.5 diopters, astigmatism less than 1.0 diopter, 18 or more years of age, stable refraction of at least one year duration, and normal corneal topography. Exclusion criteria were previous refractive surgery, unstable refraction, blepharitis, corneal disease, glaucoma, collagen vascular disease, diabetes, and topographical evidence of keratoconus. The study had the approval of the Institutional Review Board, and informed consent was obtained from all patients. All procedures were performed by the same surgeon.
The pain scoring system used in this study was the visual analogue scale, graded 0 to 10 [11]. A 0 represents no pain and a 10 means the worst pain imaginable. The scores were recorded daily and used to compare between-group pain. The total pain was the sum of pain scores during the first five postoperative days. The maximum pain was the highest pain score recorded during this period. The duration of pain was the number of days in which pain scores were recorded during the five-day period. The mean healing time was the time from the procedure to the day when the therapeutic contact lens was removed after the epithelium had healed.
Briefly, the epi-LASIK operation can be described as follows. The operative eye is anesthetized with three drops of topical proparacaine hydrochloride 0.5% (Alcaine®; Alcon Laboratories Inc., Fort Worth, TX, USA). The eye is prepared with povidone iodine and covered with a sterile drape. A speculum is applied. The corneal marking is made using an epi-LASIK marker. The Amadeus II epi-keratome handpiece (Advanced Medical Optics, Santa Ana, CA, USA) is applied to the eye, and suction is activated. Balanced salt solution acts as a lubricant to the operative cornea. The oscillating block runs parallel to the horizontal corneal plane to separate the epithelial sheet, the diameter of which is 9.0 mm. After the epithelial sheet has been successfully constructed, it is reflected nasally to allow for ablation. Surface ablation is performed with the Zywave Z100 (Bausch & Lomb, Rochester, NY, USA). After ablation, the epithelial sheet is replaced with a moistened Merocel sponge. A therapeutic contact lens (Focus 1-2 Week; CIBA Vision, Duluth, GA, USA) is then applied.
The contact lens remained in the eye until corneal surface re-epithelization was complete. Patients were given levofloxacin eye drops (Cravit®; Santen pharmaceutical, Osaka, Japan) four times daily for the first postoperative week. Fluorometholone eye drops (Santen pharmaceutical) four times daily were administered when re-epithelization was complete and were then tapered over the following four weeks. A Durogesic D-trans patch 12 µg/hr (Janssen Pharmaceutica, Piscataway, NJ, USA) and acetaminophen 650 mg were prescribed when necessary.
The operative methods for, and the postoperative management of, PRK patients are similar, the only difference being formation of the epithelial sheet in the epi-LASIK procedure. The epithelium is marked with a 9.0-mm trephine on the center of the cornea and removed mechanically in the PRK procedure, instead of forming an epithelial sheet as in the epi-LASIK technique.
Statistical analysis was performed using SPSS ver. 11.5 (SPSS Inc., Chicago, IL, USA). All visual acuity measurements were converted from Snellen acuity data to logarithms of the minimum angle of resolution. The comparisons of visual outcomes and pain scores between the two groups were performed using Student's t-tests. A p-value<0.05 was considered to be statistically significant.
The mean age in the epi-LASIK group was 28.50±6.65 years (range, 19 to 43 years) and was 28.24±4.29 years (range, 20 to 37 years) in the PRK group. There were no significant differences in spherical equivalents, astigmatism, mean keratometry, or best corrected visual acuity before surgery between the epi-LASIK and PRK groups (Table 1).
The pain score results are shown in Fig. 1. Postoperative pain scores were greater in the epi-LASIK group than in the PRK group on the fourth postoperative day. The pain score averages in the epi-LASIK and PRK groups were 0.82±1.47 and 0.26±0.78, respectively (p-value=0.017). On the other days, however, the scores did not differ significantly.
Total pain and maximal pain did not differ between the groups. The total pain score was 10.90±7.37 in the epi-LASIK group and 9.15±5.03 in the PRK group, and the maximal pain score was 4.78±2.37 in the epi-LASIK group and 5.04±2.26 in the PRK group. However, there were significant differences in pain duration between the two groups; the average number of days with pain was 2.94±1.23 in the epi-LASIK group and 2.35±1.01 days in the PRK group (p-value=0.010). The mean healing time in the epi-LASIK group was 4.53±0.77 days, which was significantly longer than the 3.76±0.85 days in the PRK group (p-value<0.001).
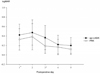
Early postoperative uncorrected visual acuities are shown in Fig. 2. On postoperative days 1 and 3, visual acuity was lower in the epi-LASIK group (0.42±0.23 and 0.36±0.26, respectively) than in the PRK group (0.31±0.21 and 0.19±0.16, respectively). At one week and one month after the surface ablation procedure, visual acuities were lower in the epi-LASIK group than in the PRK group (Fig. 3). The average visual acuities after one week and after one month were 0.18±0.17 and 0.08±0.11 in the epi-LASIK group and 0.11±0.13 and 0.02±0.08, respectively, in the PRK group. However, after further follow-up, there were no significant differences in visual acuity between the two groups.
After introduction by Pallikaris et al. [1,2], the epi-LASIK procedure was suggested to be a safe and efficient method for the correction of low-to-moderate myopia and myopic astigmatism [4,12,13]. In addition, compared with earlier techniques, reduced postoperative pain and haze levels were expected after epi-LASIK and were confirmed by some reports [4,14]. However, other reports and our results have shown that the epithelium recovers a little more slowly during the early postoperative period after the procedure, and patients have slightly more pain on postoperative day 4 as well as a longer duration of pain and slower recovery of visual acuity [10,15].
In previous studies, preservation of the intact epithelial flap separated at the level of the Bowman's layer was shown to be important for the viability of epithelial basal cells [3,16-19]. Tanioka et al. [8], however, reported that the basement membrane was partially or totally lost after epi-LASIK, and that most basal cells in the epithelial flaps appeared to be dead. In addition, it has been reported that flap viability seems to be less important in reducing postoperative pain and recovery time than is preservation of the intact lamina lucida layer of the basement membrane [20]. These differences could be related to the use of different epikeratomes. We have previously reported that mechanical scraping and epi-LASIK were superior to laser epithelial keratomileusis in terms of preservation of the epithelial basement membrane and basal epithelial cells [21]. However, the preservation ratio seemed to differ between polymethylmethacrylate and metal blade versions of the procedure [21]. In this study, the Amadeus II microkeratome was used, as in a previous report that showed intact epithelial flaps at the level of the Bowman's layer [17]. In spite of this, in some patients the retained epithelial sheet became whitish apoptotic tissue. We believe that the epithelium remaining on the stromal bed became whitish apoptotic tissue which then caused more inflammation and slowed recovery. It has been suggested that in these cases the basement membrane could not act as a barrier, and that apoptosis of the residual epithelial flap could cause inflammation and postoperative pain. In addition, redundancy of the flap could also be a cause of inflammation and pain [9]. In the current study, visual recovery after the epi-LASIK procedure was slower than that after PRK. This difference could also be related to the remaining epithelial sheet. The authors speculated that residual epithelium could cause inflammation and could also act as an obstacle to re-epithelialization; longer pain duration and mean healing time support this hypothesis. However, consistent with previous data, no significant difference was noted in the uncorrected visual acuities three and six months after operation [7]. Moreover, other studies have reported that epi-LASIK provides excellent refractive and visual outcomes 12 months after surgery [5,7].
In the study presented here, there were no differences in pain scores on the first and second postoperative days, when almost all patients felt some discomfort. Although there was a significant difference in pain scores between the two groups on the fourth postoperative day, this could be clinically less meaningful. However, epi-LASIK resulted in a longer pain duration and a longer mean healing time. These could be meaningful differences between the two procedures.
The major limitation of this study was the retrospective, case-control nature of the study design. To obtain a more accurate comparison between groups, a prospective contralateral blind study should be designed for future investigation. Another limitation of this study is the small number of subjects in each group due to the attempts to match preoperative data between the two groups. Another limitation is that our report could not exclude differences arising from the use of different epikeratomes. More studies are needed to investigate this aspect. The residual epithelial sheet could be a cause of postoperative pain and slow epithelial healing in our study. Therefore, further studies should investigate other epithelial flap-management techniques, such as off-flap epi-LASIK, as well as histological comparisons between flap-management techniques.
Figures and Tables
Fig. 1
Early postoperative daily pain scores. epi-LASIK=epithelial laser in situ keratomileusis; PRK=photorefractive keratectomy. *p-value=0.017.
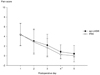
Fig. 2
Early postoperative uncorrected visual acuities. logMAR=logarithm of the minimum angle of resolution; epi-LASIK=epithelial laser in situ keratomileusis; PRK=photorefractive keratectomy. *p-value=0.021; †p-value<0.001.
Notes
References
1. Pallikaris IG, Naoumidi II, Kalyvianaki MI, Katsanevaki VJ. Epi-LASIK: comparative histological evaluation of mechanical and alcohol-assisted epithelial separation. J Cataract Refract Surg. 2003. 29:1496–1501.
2. Pallikaris IG, Katsanevaki VJ, Kalyvianaki MI, Naoumidi II. Advances in subepithelial excimer refractive surgery techniques: Epi-LASIK. Curr Opin Ophthalmol. 2003. 14:207–212.
3. Netto MV, Mohan RR, Ambrosio R Jr, et al. Wound healing in the cornea: a review of refractive surgery complications and new prospects for therapy. Cornea. 2005. 24:509–522.
4. Pallikaris IG, Kalyvianaki MI, Katsanevaki VJ, Ginis HS. Epi-LASIK: preliminary clinical results of an alternative surface ablation procedure. J Cataract Refract Surg. 2005. 31:879–885.
5. Dai J, Chu R, Zhou X, et al. One-year outcomes of epi-LASIK for myopia. J Refract Surg. 2006. 22:589–595.
6. Katsanevaki VJ, Kalyvianaki MI, Kavroulaki DS, Pallikaris IG. One-year clinical results after epi-LASIK for myopia. Ophthalmology. 2007. 114:1111–1117.
7. O'Doherty M, Kirwan C, O'Keeffe M, O'Doherty J. Postoperative pain following epi-LASIK, LASEK, and PRK for myopia. J Refract Surg. 2007. 23:133–138.
8. Tanioka H, Hieda O, Kawasaki S, et al. Assessment of epithelial integrity and cell viability in epithelial flaps prepared with the epi-LASIK procedure. J Cataract Refract Surg. 2007. 33:1195–1200.
9. Nishi Y, Nishi O, Nishi K, Auffarth G. Pain reduction after epi-LASIK with a simple surgical procedure. J Cataract Refract Surg. 2007. 33:555–557.
10. Torres LF, Sancho C, Tan B, et al. Early postoperative pain following Epi-LASIK and photorefractive keratectomy: a prospective, comparative, bilateral study. J Refract Surg. 2007. 23:126–132.
11. Blake CR, Cervantes-Castaneda RA, Macias-Rodriguez Y, et al. Comparison of postoperative pain in patients following photorefractive keratectomy versus advanced surface ablation. J Cataract Refract Surg. 2005. 31:1314–1319.
12. Matsumoto JC, Chu YS. Epi-LASIK update: overview of techniques and patient management. Int Ophthalmol Clin. 2006. 46:105–115.
13. Shin SJ, Kim MJ, Park SH, Joo CK. Clinical outcomes of wavefront-guided Epi-LASIK: 6-months follow-up. J Korean Ophthalmol Soc. 2007. 48:642–648.
14. Gamaly TO, El Danasoury A, El Maghraby A. A prospective, randomized, contralateral eye comparison of epithelial laser in situ keratomileusis and photorefractive keratectomy in eyes prone to haze. J Refract Surg. 2007. 23:S1015–S1020.
15. Hondur A, Bilgihan K, Hasanreisoglu B. A prospective bilateral comparison of epi-LASIK and LASEK for myopia. J Refract Surg. 2008. 24:928–934.
16. Katsanevaki VJ, Naoumidi II, Kalyvianaki MI, Pallikaris G. Epi-LASIK: histological findings of separated epithelial sheets 24 hours after treatment. J Refract Surg. 2006. 22:151–154.
17. Kollias A, Ulbig MW, Spitzlberger GM, et al. Epi-LASIK using the Amadeus II microkeratome: evaluation of cut quality using light and electron microscopy. J Cataract Refract Surg. 2007. 33:2118–2121.
18. Shah S, Sebai Sarhan AR, Doyle SJ, et al. The epithelial flap for photorefractive keratectomy. Br J Ophthalmol. 2001. 85:393–396.
19. Alio JL, Rodriguez AE, Mendez MC, Kanellopoulos J. Histopathology of epi-LASIK in eyes with virgin corneas and eyes with previously altered corneas. J Cataract Refract Surg. 2007. 33:1871–1876.
20. Camellin M, Wyler D. Epi-LASIK versus epi-LASEK. J Refract Surg. 2008. 24:S57–S63.
21. Choi CY, Kim JY, Kim MJ, Tchah H. Transmission electron microscopy study of corneal epithelial flaps following removal using mechanical scraping, alcohol, and epikeratome techniques. J Refract Surg. 2008. 24:667–670.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download