Abstract
Graphical Abstract
Figures and Tables
Table 1
Demographic data on the nursing home residents (NHR) and community-dwelling individuals (CDI) group

Table 2
External factors related to nursing home residents' hip fractures (n = 46)
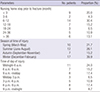
Table 3
Comparison of capacity for activity at time of final follow-up among the nursing home residents (NHR) and community-dwelling individuals (CDI) group
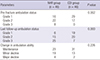
Table 4
Comparison of external factors at time of final follow-up among the nursing home residents (NHR) (n = 35) and community-dwelling individuals (CDI) (n = 36) group
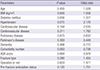
Table 5
Comparison of capacity for activity at time of final follow-up among patients who survived at least one year in the nursing home residents (NHR) and community-dwelling individuals (CDI) group
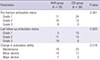
Table 6
Comparison of external factors at time of final follow-up among patients who survived at least one year in the nursing home residents (NHR) (n = 35) and community-dwelling individuals (CDI) (n = 36) group
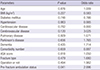
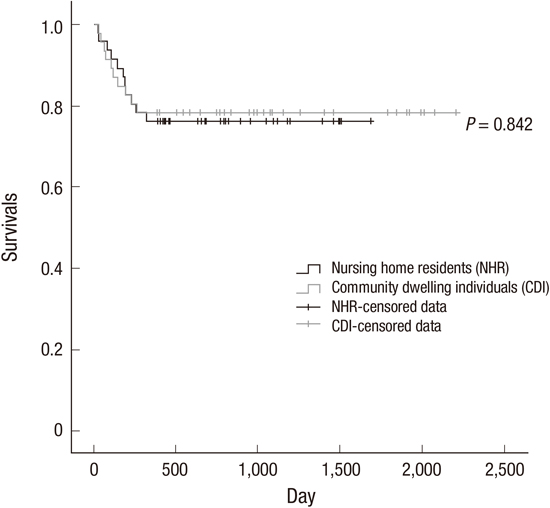
Table 7
Comparison of rates of death between the nursing home residents (NHR) and community-dwelling individuals (CDI) groups
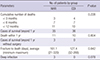
Table 8
Comparison between those who died within one year and those who survived for at least one year among patients in NHR group

Notes
AUTHOR CONTRIBUTION Conception and coordination of the study: Cho HM. Design of ethical issues: Cho HM, Min W, Lee K. Acquisition of data: Cho HM, Min W. Data review: Cho HM, Min W. Statistical analysis: Cho HM, Min W. Manuscript preparation: Cho HM, Min W, Lee K. Administrative, technical, or material support: Choi YS, Min W, Lee HS, Mun HJ, Shim HY, Lee DG, Yoo MJ. Manuscript approval: all authors.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download