See the article "".
We read with interest the article of Lee et al. (1) about the diagnostic implementation of an automated liquid culture system in tuberculous pleural effusion (TPE). They reported that the performance of liquid culture system proved superior to that of solid media in pleural fluid culture and the combined use of liquid and solid media increased the sensitivity only by a further 1% when compared to that observed using liquid media alone. Therefore, they expressed that supplemental solid media might have a limited impact on maximizing sensitivity in pleural fluid culture but recommended further studies. Recently, an automated liquid culture system has been widely used for mycobacterial culture from respiratory specimens including pleural fluid. However, limited data are available regarding the respective contribution of liquid and solid media to the microbiologic yields from pleural fluid in human immunodeficiency virus- uninfected patients with TPE. Therefore, we investigated the respective diagnostic contribution of liquid and solid media in pleural fluid culture of patients with TPE.
Data from 182 consecutive patients who were diagnosed with TPE between 2011, May, when the mandatory implementation of the combined solid and liquid media has been introduced on mycobacterial culture, and 2014, December at Kyungpook National University Hospital, South Korea, were retrospectively reviewed. These 182 TPE patients included confirmed 123 (68%) cases (positive Mycobacterium tuberculosis [MTB] culture from respiratory specimens [n = 106] and granulomatous inflammation in pleural biopsy tissue [n = 17]) and probable 59 (32%) cases (lymphocytic exudate, high adenosine deaminase > 40 U/L, and clinical and radiological improvement after anti-tuberculosis treatment). MTB culture was performed by inoculating the respiratory specimens including pleural fluid into BACTEC MGIT 960 liquid medium (BD Diagnostic Systems, USA) and 3% Ogawa solid medium (Shin-yang Chemical, Korea) at the laboratory by incubating them for 6 weeks and 8 weeks, respectively.
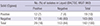
The culture-positive yields of liquid and solid media from pleural fluid were summarized in Table 1. Of the 182 pleural fluid samples, 36 (20%) were culture-positive on either liquid or solid medium and 12 (7%) positive on both media. Seventeen (9%) and 7 (4%) were culture-positive in liquid and solid media alone, respectively. The positive yield (16%) of liquid media was significantly higher than that of solid media (10%) (P = 0.032 by McNemar's test). However, approximately 20% (7/36) of overall culture-positive yields from pleural fluid were achieved by the solid media alone, and the combined use of liquid and solid media increased the recovery rate of MTB by a further 4% as compared to use of liquid media alone (20% vs. 16%, P = 0.016).
Our finding showed that solid media provided a significant contribution to the microbiologic yields from pleural fluid, which cannot be neglected. This finding is supported by a previous prospective study that solid media increased the diagnostic yields by a further 13% when compared to use of liquid media alone (2). Discrepant results between our and Lee et al.'s (1) studies using the same culture methods may be partly attributable to relatively lower positive yield of our liquid media compared to previous studies. However, the positive yield of liquid culture system has been reported to vary greatly from 21% to 63% (34), and data of liquid media from pleural fluid, in our area with an intermediate prevalence of tuberculosis, are limited. In addition, our liquid culture results are not significantly different from a 23% positive rate of laboratory inoculation (2) (P = 0.250), and a 24% positive yield of bedside inoculation (5) (P = 0.314) which usually provides better results than laboratory inoculation (23).
Direct comparisons with the results of liquid media obtained from other studies are limited due to differences in the volumes of sediment inoculated, time from sampling to inoculation, or population studied, even though the same culture technique was used. The contribution of solid media in Lee et al.'s study appears negligible. However, it should be further observed whether this finding is consistent, through the long term follow-up with a large sample size. Our results support the current guidelines to recommend the combined use of liquid and solid media in pleural fluid culture of patients suspected of having TPE (6).
Figures and Tables
References
1. Lee BH, Yoon SH, Yeo HJ, Kim DW, Lee SE, Cho WH, Lee SJ, Kim YS, Jeon D. Impact of implementation of an automated liquid culture system on diagnosis of tuberculous pleurisy. J Korean Med Sci. 2015; 30:871–875.
2. Maartens G, Bateman ED. Tuberculous pleural effusions: increased culture yield with bedside inoculation of pleural fluid and poor diagnostic value of adenosine deaminase. Thorax. 1991; 46:96–99.
3. Cheng AF, Tai VH, Li MS, Chan CH, Wong CF, Yew WW, Hui M, Chan CY, Lee JC. Improved recovery of Mycobacterium tuberculosis from pleural aspirates: bedside inoculation, heparinized containers and liquid culture media. Scand J Infect Dis. 1999; 31:485–487.
4. Ruan SY, Chuang YC, Wang JY, Lin JW, Chien JY, Huang CT, Kuo YW, Lee LN, Yu CJ. Revisiting tuberculous pleurisy: pleural fluid characteristics and diagnostic yield of mycobacterial culture in an endemic area. Thorax. 2012; 67:822–827.
5. Luzze H, Elliott AM, Joloba ML, Odida M, Oweka-Onyee J, Nakiyingi J, Quigley M, Hirsch C, Mugerwa RD, Okwera A, et al. Evaluation of suspected tuberculous pleurisy: clinical and diagnostic findings in HIV-1-positive and HIV-negative adults in Uganda. Int J Tuberc Lung Dis. 2001; 5:746–753.
6. Canadian Thoracic Society. Canadian Tuberculosis Standards, 7th edition. Can Respir J. 2013; 20:1A–173A.
We appreciate their interest in our manuscript entitled "Impact of Implementation of an Automated Liquid Culture System on Diagnosis of Tuberculous Pleurisy" (1) and would like to thank them for sharing their valuable data. Both these studies are comparable because the same culture technique was used for similar populations.
The results of both studies were consistent in that the culture yields obtained using liquid media from pleural fluid were higher than that using solid media. In addition, there was no bacterial contamination or isolation of nontuberculous mycobacteria in the effusion culture, although this was not clearly mentioned in their letter.
The differences in findings between both studies were with respect to the diagnostic contribution of supplemental solid media and overall sensitivity of pleural fluid culture. When compared to the use of liquid culture, they showed that the solid media increased the diagnostic yields by 4%, in contrast to only 1% in our study. Therefore, they suggested that solid media could significantly contribute to the microbiologic yields from pleural fluid. We agree that additional, large scale studies are required to resolve this discrepancy, because both studies used small sample size from a single institute.
However, we would like emphasize that the main finding of our study was high microbial yields from pleural fluid with the implementation of liquid media. In our study, effusion culture using liquid media alone provided a confirmatory diagnosis in about 40% of the patients, in contrast to the combined 20% for liquid and solid media in their study, and in nearly two thirds of the patients when combined with the sputum culture. Therefore, the combination of effusion and sputum cultures could be a reasonable approach for the diagnosis of tuberculous pleurisy. Furthermore, high microbial yield using liquid media may facilitate early and adequate treatment especially in highly drug resistant areas, consequently improving the outcome of patients with tuberculous pleurisy. We believe that such advances in culture techniques may have an impact on the diagnosis and management of tuberculous pleurisy. We also agree with their explanation regarding the inconsistency in culture yields between the two studies and the need for further studies.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download