Abstract
Percutaneous device closure for secundum atrial septal defects (ASDs) has been performed commonly and safely with high success rates. However, it is still challenging to close ASDs that are surrounded with deficient or hypermobile rims and could be compromised with an unexpected migration of device. We report a case of percutaneous Amplazter Septal Occluder (ASO; St. Jude Medical Inc., St. Paul, Minnesota, USA) device closure for an ASD with a thin and floppy interatrial septum, which immediately migrated into the right atrium and was not pulled back into the delivery sheath. To our knowledge, this is the first report on a successful percutaneous retrieval and redeployment of the device in such a situation, preventing any vascular injury or unplanned emergency open heart surgery.
The Amplazter Septal Occluder (ASO; St. Jude Medical Inc., St. Paul, Minnesota, USA) has been widely used to occlude secundum atrial septal defects (ASDs) (1, 2). ASO migration or embolization after deployment is rare, with a reported rate ranging from 0.5% to 3% (3, 4), and it occurs more frequently in cases of ASD without sufficient surrounding rims. Once it arises it may lead to an emergency surgical approach, however the unique design of the ASO allows for retrieval of the migrated device percutaneously. Herein, we report a case of percutaneous retrieval of a migrated ASO into the right atrium and its successful redeployment without any complications.
A 45-yr-old woman with no previous illnesses presented with exercise intolerance on 7th March 2013. Physical examination showed a normal blood pressure of 110/70 mmHg with a regular heart rate of 68 beats/min and an oxygen saturation of 97% on room air. Cardiac auscultation revealed the fixed splitting second heart sound. An oval-shaped secundum-type ASD with a left-to-right shunt was detected on transthoracic echocardiography (TTE). The defect size was 12 mm×18 mm on 3D-transesophageal echocardiography (TEE), which was surrounded with thin, floppy interatrial septum (IAS) and deficient aortic rim (Fig. 1A-C). On cardiac catheterization, the calculated Qp/Qs and Rp/Rs were 1.88 and 0.03, respectively. We decided to close the defect percutaneously with the ASO under TEE and fluoroscopic guidance. Since the balloon stretched diameter was 19 mm, we chose a 20 mm-sized ASO. The device was loaded onto an 8-French (Fr) delivery system (AGA Medical, Golden Valley, Minnesota, USA) and advanced into the left atrium. At first, improper alignment of the ASO with the plane of IAS and the flimsy rim prohibited the left atrial (LA) disc from holding the inferior rim firmly, resulting in herniation into the right atrium. To overcome these difficulties, we used the left upper pulmonary vein technique; opened the LA disc partially in the left upper pulmonary vein and released the waist and the right atrial (RA) disc quickly before the alignment of the system changed significantly. With this maneuver we could place the ASO in a proper position confirmed by 2D-TEE. We performed the "Minnesota wiggle" to ensure a firm position of the device. However, the 3D-TEE just after detachment of the ASO from the delivery cable noted that the device settled in an oblique position with its superior portion prolapsing into the right atrium (Fig. 1D). Although more than 75% of the rim was trapped by the discs, it was slipping down into the right atrium with the heart movements, resulting in a left-to-right shunt (Fig. 1E). Given the high risk of migration, we captured the device using a GooseNeck snare (St. Jude Medical, Sylmar, CA, USA) with surgical backup. We paid special attention not to lose the accessibility to the snared ASO. The attempt to reposition the prolapsed part of the disc using a 7-Fr internal mammary catheter via another approach through femoral vein was failed. The device completely migrated into the right atrium but still was held on to the snare (Fig. 2A). We pulled back the snared ASO into the femoral vein because the 8-Fr delivery sheath could not accommodate it. At that position, the delivery sheath was replaced by a 12-Fr femoral sheath through which the device was re-snared and retrieved (Fig. 2B). The device was remounted on the cable and the defect was closed successfully in the same manner (Fig. 1F, 2C). The patient was discharged uneventfully on the next day. The occluder has been in the correct position without a residual shunt on Doppler echocardiography at 30 days after the procedure.
The overall incidence of ASD occluder complications has been reported as ranging from 5.2% to 8.6% (1). Among them, device embolization or migration are the most frequent major complications with an incidence from 0.5% to 3% (2). A deficient aortic rim and a thin and floppy posterior rim have been known as the causative factors for migration (5). One of the solutions to this problem is slight oversizing - that is, using a device 2 to 4 mm larger than the stretched diameter. However, because of concerns about erosion, we selected a just 1 mm larger device in this case. (6). Although we could achieve an acceptable position wherein more than 75% of the rim was trapped around the defect, the hypermobile atrial septum could not offer enough support for device stabilization, leading to migration. Once it is migrated, adjusting the device into a safe position to prevent further embolization is the first key step. It can be achieved by supporting with some devices including stiff wire or bioptome for stabilization and snare loop, tulip shaped snare, basket or alligator clamps to grab the device (4, 7, 8). When this step is failed or not suitable, an emergency surgical correction should be considered. If the device is recaptured again, it can be retrieved into the delivery sheath and this procedure could be done more easily with use of a 2-Fr sizes larger sheath than the recommended size for device delivery. We believe that when it is difficult to pull back the snared device into the delivery sheath and size of the device is considered suitable enough not to cause vascular or any surrounding structural injuries, it is prudent to place the device in the femoral vein, from where it can be easily retrieved through another large-sized femoral sheath, as in the present case.
Our case demonstrated several points: 1) 3D-TEE can provide additional information on the anatomic relationship between the device and the ASD; 2) the device slipping in one portion and sitting on a floppy septum should be rectified, and 3) moving the migrated device into the femoral vein could be an alternative method for a safe retrieval in such a situation for the moderate sized ASO.
Figures and Tables
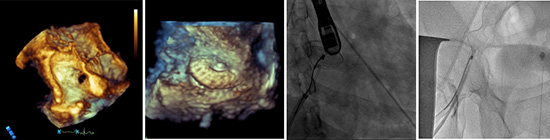
Fig. 1
Echocardiographic findings. (A) 3D multi-planar reconstruction (MPR) view showed inferior and superior vena cava (SVC) rims. (B) While aortic rim was almost absent, posterior rim seemed to be sufficient but was thin and floopy. (C) On the view from right atrium (RA), an oval-shaped, secundum-type atrial septal defect (*) was shown in this 3D MPR image. (D) Just after device deployment, 3D transesophageal echocardiography (TEE) showed the oblique settlement of the device with its superior portion slipping into the RA. (E) Remnant shunt flow at the side of SVC rim was noted in color doppler image. (F) The successfully closed defect with the device was shown in this 3D-TEE image. IVC, inferior vena cava; SVC, superior vena cava; LA, left atrium; RA, right atrium; ASO, Amplater Septal Occluder.

Fig. 2
Fluoroscopic findings during procedure. (A) The GooseNeck snare captured the screw on the right atrial side of the device. (B) After femoral sheath change into the larger one, the device was jammed into the sheath and was removed. (C) Subsequently, the same device was deployed successfully. TEE, transesophageal echocardiography; ASO, Amplatzer Septal Occluder.

References
1. Chessa M, Carminati M, Butera G, Bini RM, Drago M, Rosti L, Giamberti A, Pomè G, Bossone E, Frigiola A. Early and late complications associated with transcatheter occlusion of secundum atrial septal defect. J Am Coll Cardiol. 2002; 39:1061–1065.
2. Du ZD, Hijazi ZM, Kleinman CS, Silverman NH, Larntz K. Amplatzer Investigators. Comparison between transcatheter and surgical closure of secundum atrial septal defect in children and adults: results of a multicenter nonrandomized trial. J Am Coll Cardiol. 2002; 39:1836–1844.
3. Losay J, Petit J, Lambert V, Esna G, Berthaux X, Brenot P, Angel C. Percutaneous closure with Amplatzer device is a safe and efficient alternative to surgery in adults with large atrial septal defects. Am Heart J. 2001; 142:544–548.
4. Levi DS, Moore JW. Embolization and retrieval of the Amplatzer septal occluder. Catheter Cardiovasc Interv. 2004; 61:543–547.
5. Pedra CA, Pedra SR, Esteves CA, Cassar R, Pontes SC Jr, Braga SL, Fontes VF. Transcatheter closure of secundum atrial septal defects with complex anatomy. J Invasive Cardiol. 2004; 16:117–122.
6. Moore J, Hegde S, El-Said H, Beekman R 3rd, Benson L, Bergersen L, Holzer R, Jenkins K, Ringel R, Rome J, et al. Transcatheter device closure of atrial septal defects: a safety review. JACC Cardiovasc Interv. 2013; 6:433–442.
7. Guimaraes M, Denton CE, Uflacker R, Schonholz C, Selby B Jr, Hannegan C. Percutaneous retrieval of an Amplatzer septal occluder device that had migrated to the aortic arch. Cardiovasc Intervent Radiol. 2012; 35:430–433.
8. Goel PK, Kapoor A, Batra A, Khanna R. Transcatheter retrieval of embolized AMPLATZER Septal Occluder. Tex Heart Inst J. 2012; 39:653–656.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download