Abstract
A 51-yr-old man presented exertional dyspnea as a consequence of iliocaval fistula combined with paradoxical pulmonary embolism and high-output heart failure. Endovascular stent-graft repair was performed to cover iliocaval fistula and restore the heart function. After the procedure, dyspnea was improved and procedure related complication was not seen. A 6-month follow-up computed tomography showed regression of pulmonary thromboembolism and well-positioned stent-graft without graft migration, aortacaval communication or endoleak. Stent graft implantation should be considered an alternative of open repair surgery for treament of abdominal arteriovenous fisula, especially in patient with high risk for surgery.
Spontaneous abdominal arteriovenous fistula is a very uncommon clinical condition found in only 1% of all abdominal aortic aneurysm (1). Such fistula classically present with a triad of high-output heart failure, pulsatile abdominal mass with a bruit and unilateral leg ischemia or venous congestion (2). Paradoxical pulmonary embolism related with arteriovenous fistula is exceedingly rare, but this situation can be developed and is very serious complication of arteriovenous fistula (3). Therefore, prompt repair of arteriovenous fistula is mandatory to restore hemodynamics and prevent recurrent pulmonary embolism in such condition. However, traditional treatment consists of open surgery is associated with high morbidity and mortality (4). Thus endovascular treatment may be considered as alternative.
Here, we report the case of a iliocaval fistula presenting with paradoxical pulmonary embolism combined with high-output heart failure that was successfully treated by endovascular stent-graft repair.
A 51-yr-old male was admitted on April 4, 2012, with palpitation and exertional dyspnea gradually deteriorated for a week. He visited other hospital a week ago, because anorexia, nausea, vomiting and abdominal discomfort developed and continued for three weeks without any improvement. In that hospital, right iliac artery aneurysm (4.5 cm in diameter) with iliocaval shunt combined with thrombus was found incidentally by contrast-enhanced computed tomography (CT) (Fig. 1A-C). He was referred to our hospital for proper management of iliocaval fistula. His risk factor of iliac aneurysm was hypertension. However, he have not underwent any abdominal trauma or surgery.
On admission to our hospital, his vital sign were blood pressure of 137/82 mmHg, heart rate of 103 beats/min, respiratory rate of 20/min, body temperature of 36.5℃, and oxygen saturation of 96%. His heart sound was regular and rapid. Rale was auscultated on both lower lung field. Bruit detected by auscultation of right inguinal area and palpable mass was not identified. There was no leg edema and normal peripheral arterial pulse was detected in both lower extremities.
Laboratory test showed a slight elevated C-reactive protein of 0.95 mg/dL (normal range < 0.3 mg/dL) without leukocytosis, creatinine level of 1.45 mg/dL (normal range: 0.5-1.3 mg/dL), aspartate transaminase of 56 IU/L (normal range: 12-33 IU/L) and alanine transaminase of 119 IU/L (normal range: 5-35 IU/L). Platelet, bilirubin, and international normalized ratio was within normal range and electrolyte or acid-base imbalance was not found. CK-MB and Troponin T was within normal range, but NT pro-BNP was elevated to 2,404 pg/mL (normal range: 5-125 pg/mL). Electrocardiogram showed sinus tachycardia without abnormal ST segment or T wave change. Cardiomegaly with pulmonary edema and bilateral pleural effusion in simple chest x-ray was detected. We considered possibility of heart failure, and examined echocardiogram. Ejection fraction was 63% and regional wall motion abnormalities was not observed. These findings suggested high-output heart failure. Right atrial and ventricular dilatation, D-shaped left ventricle, and the dilatation of inferior vena cava was identified incidentally. Contrast-enhanced chest CT was performed and showed pulmonary thromboembolism involved right lower lobe base segmental pulmonary artery (Fig. 2A, B). We checked doppler sonography of lower extremities, tumor markers, and upper and lower endoscopy for evaluate origin of emboli. There were no evidence of deep vein thrombosis or malignancy. Therefore, we concluded that pulmonary emboli was originated from thrombus in iliac aneurysmal sac.
We decided to treat his iliocaval shunt by endovascular stent graft implantation for restoring heart function and preventing recurrent pulmonary embolism. For a start embolization of right common iliac artery was performed with PLUG 10mm (Amplatzer vascluar plug, Aga Medical Corp) (Fig. 3A). Angiogram showed aneurysmal dilatation of right common iliac artery and iliocaval shunt. Some filling defects near the aneurysm, suggesting of thrombi (Fig. 3B). Then two graft stents (Excluder contralateral leg 12/100 mm, 12/120 mm, W.L Gore and Associates) are placed at right common iliac artery. Post-stenting balloon angioplasties were performed (EverCross 12/40 mm, EV3 Inc). After the procedure, aortogram showed well implanted graft stents and no visible of IVC and endoleak (Fig. 3C). After the implantation of graft stents, dyspnea was improved and follow up creatinine level and liver enzymes were normalized. Simple chest x-ray showed no pulmonary edema or pleural effusion at discharge. Coumadization was started for resolution and prevention of pulmonary embolism.
At routine follow up 6 months after the procedure, the patient was in good clinical condition. Echocardiogram showed that D-shaped left ventricle was completely resolved and right atrial and ventricular size was normalized. CT demonstrated that the stent-graft was patent and well-postioned, without evidence of graft migration, aortacaval communication or endoleak (Fig. 1D-F). Pulmonary embolism was mostly regressed (Fig. 2C, D).
Iliocaval fistula is an abnormal connection between the iliac artery and the inferior vena cava (IVC) that can be occurred spontaneously as a result of the complication of iliac artery aneurysm (1). Other possible causes of iliocaval fistula include trauma, iatrogenic injury, mycotic aneurysm, syphilitic aneurysm and connective tissue disease, such as Ehler-Danlos syndrome (5). The patient described in this report did not undergo trauma or operation and did not have a specific medical history except hypertension. Presumably iliocaval fisula of the patient might be associated with atherosclerotic or degenerative iliac artery aneurysm that had spontaneously eroded into the IVC.
Abdominal arteriovenous fistula have various hemodynamic consequence. Pulsatile abdominal mass with bruit, high-ouput cardiac failure and manifestations of regional venous hypertension and stasis are common symptoms associated with arteriovenous fistula (6). Sometimes there are no regional symptoms and could progress to multiple organ failure (7). In the present patient, there was no pulsatile abdominal mass.
Traditionally, angiography has been used as a diagnostic method to confirm the clinical suspicion of arteriovenous fistula and essential in deciding the treatment modality. Recently, CT play an important role in identifying arteriovenous fistula as a easily available and non-invasive tool after Cheung et al. (8) firstly described arteriovenous fistula that was diagnosed by CT in 1987. Important radiologic features include iliac artery aneurysm, vena caval dilatation, and increased density of IVC similar to that of the aorta and visualization of the fistula (2,8,9). The CT findings of our patient showed that iliac artery aneurysm including thrombi and increased density of IVC similar to that of iliac artery in arterial phase.
Symptoms and signs related with pulmonary thromboembolism are similar to high-ouput cardiac failure. Therefore, pulmonary thromboembolism combined with abdominal arteriovenous fistulas could be ignored easily. In our patients, echocardiographic findings such as D-shaped left ventricle were helpful in detecting pulmonary embolism. Therefore echocardiogram may be necessary to exclude low ejection fraction heart failure and find pulmonary embolism in patients with abdominal arteriovenous fistula.
Although excessively rare, there are reports have described paradoxical pulmonary embolism as a consequence of emboli passing from an iliac artery aneurysm through an iliaocaval fistula into the venous circulation. We reviewed systematically with the keywords "paradoxical embolism", "paradoxical pulmonary embolism", "arteriovenous fistula", "arteriocaval fistula", and "iliocarval fistula". A toal of ten cases was reported in literature. Cases related to iliac artery were three. Only two cases were treated by endovascular repair and other seven cases were treated by surgery and another case was described autopsy finding (3, 10) The present iliocaval fistula was the third case treated by endovascular repair.
Until recently, open surgery was a traditional treatment, but mortality rate is high, ranging from 20%-50% according to previous reports (9, 11). Additionally, in case of combined pulmonary embolism like the present patient, the risk of mortality may be increasing. Furthermore, open surgery increase bleeding risk and can make a difficulty in using coumadization for treating pulmonary embolism. Endovascular repair used as a alternative method since the early 1990s. Endovascular repair showed successful result and decreased morbidity, mortality, and hospitalized period in the previous literatures (7). However, only small numbers of patients have been treated by endovascular repair and long-term follow up is lacking (7). Endovascular repair had limitation that patient condition, anatomical suitability, and technical availability (3, 7). The present patient had the high risk of mortality or morbidity in open surgery. The site of iliocaval fistula was anatomically and technically suitable and feasible for endovascular repair as the proximal and distal margin of stent-graft landing zone was enough and adequate. Therefore, we successfully performed stent-graft repair for iliocaval fistula and 6-month follow up result was satisfied.
In conclusion, paradoxical pulmonary embolism have to be considered in case of abdominal arteriovenous fistula although excessive rare. Endovascular repair by stent-graft is one of the treatment of available option for the treatment of arteriovenous fistula combinded with pulmonary embolism.
Figures and Tables
Fig. 1
Contrast-enhanced abdominal CT images. (A-C) Images at diagnosis showed 40×38 mm sized right iliac artery aneurysm and iliocaval fistula (black arrow) with thrombus (white arrows). (D-F) Follow-up images at 6 months after endovascular stent-graft repair demonstrated patency of the graft, without evidence of graft migration or aortocaval communication. (A, D) Transverse veiw; (B) Coronal view; (C) Sagittal view; (E) Coronal maximal intensity projection view; (F) Sagittal maximal intensity projection view.
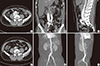
Fig. 2
Contrast-enhanced chest CT images. (A, B) Images at diagnosis showed pulmonary thromboembolism (arrows) that involved right lower lobe base segmental pulmonary artery. (C, D) Follow-up chest CT scans at 6 months after coumadization showed much regressed pulmonary embolism. (A, C) Arterial phase; (B, D) Venous phase.

Fig. 3
Angiography findings. (A) Embolization of right common iliac artery was performed with PLUG 10 mm (dotted arrow). (B) Pelvic arteriogram showed aneurysmal dilatation of right common iliac artery, iliocaval shunt and some filling defects near the aneurysm (white arrow indicate thrombus). (C) Angiography after deployment of the stents showed well implanted graft stents and no visible of IVC.

References
1. Gilling-Smith GL, Mansfield AO. Spontaneous abdominal arteriovenous fistulae: report of eight cases and review of the literature. Br J Surg. 1991; 78:421–425.
2. Lim RP, Stella DL, Dowling RJ, Campbell WA, Hebbard GS. Iliocaval arteriovenous fistula presenting with multiple organ failure. Australas Radiol. 2006; 50:381–385.
3. De Rango P, Parlani G, Cieri E, Verzini F, Isernia G, Silvestri V, Cao P. Paradoxical pulmonary embolism with spontaneous aortocaval fistula. Ann Vasc Surg. 2012; 26:739–746.
4. Schmidt R, Bruns C, Walter M, Erasmi H. Aorto-caval fistula--an uncommon complication of infrarenal aortic aneurysms. Thorac Cardiovasc Surg. 1994; 42:208–211.
5. Rajmohan B. Spontaneous aortocaval fistula. J Postgrad Med. 2002; 48:203–205.
6. Leigh-Smith S, Smith RC. Aorto caval fistula: the "bursting heart syndrome". J Accid Emerg Med. 2000; 17:223–225.
7. Antoniou GA, Koutsias S, Karathanos C, Sfyroeras GS, Vretzakis G, Giannoukas AD. Endovascular stent-graft repair of major abdominal arteriovenous fistula: a systematic review. J Endovasc Ther. 2009; 16:514–523.
8. Cheung A, Shuman WP, Kohler TR. Diagnosis by computed tomography of arteriovenous fistula complicating ruptured iliac artery aneurysm. J Vasc Surg. 1987; 6:605–608.
9. Brewster DC, Cambria RP, Moncure AC, Darling RC, LaMuraglia GM, Geller SC, Abbott WM. Aortocaval and iliac arteriovenous fistulas: recognition and treatment. J Vasc Surg. 1991; 13:253–264.
10. Melas N, Saratzis A, Abbas A, Sarris K, Saratzis N, Lazaridis I, Kiskinis D. Endovascular repair of a spontaneous ilio-iliac fistula presenting as pulmonary embolism. Vasa. 2011; 40:246–250.
11. Woolley DS, Spence RK. Aortocaval fistula treated by aortic exclusion. J Vasc Surg. 1995; 22:639–642.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download