1. Polonsky KS, Sturis J, Bell GI. Seminars in Medicine of the Beth Israel Hospital, Boston. Non-insulin-dependent diabetes mellitus: a genetically programmed failure of the beta cell to compensate for insulin resistance. N Engl J Med. 1996; 334:777–783.
2. Schäfer SA, Machicao F, Fritsche A, Häring HU, Kantartzis K. New type 2 diabetes risk genes provide new insights in insulin secretion mechanisms. Diabetes Res Clin Pract. 2011; 93:S9–S24.
3. Costanzo BV, Trischitta V, Di Paola R, Spampinato D, Pizzuti A, Vigneri R, Frittitta L. The Q allele variant (GLN121) of membrane glycoprotein PC-1 interacts with the insulin receptor and inhibits insulin signaling more effectively than the common K allele variant (LYS121). Diabetes. 2001; 50:831–836.
4. Abate N, Chandalia M, Satija P, Adams-Huet B, Grundy SM, Sandeep S, Radha V, Deepa R, Mohan V. ENPP1/PC-1 K121Q polymorphism and genetic susceptibility to type 2 diabetes. Diabetes. 2005; 54:1207–1213.
5. Wang M, Peng C, Qu YL, Huang QY. Association and meta-analysis of ENPP1 K121Q with type 2 diabetes in Han Chinese. Yi Chuan. 2010; 32:808–816.
6. Seo HJ, Kim SG, Kwon OJ. The K121Q polymorphism in ENPP1 (PC-1) is not associated with type 2 diabetes or obesity in Korean male workers. J Korean Med Sci. 2008; 23:459–464.
7. Keshavarz P, Inoue H, Sakamoto Y, Kunika K, Tanahashi T, Nakamura N, Yoshikawa T, Yasui N, Shiota H, Itakura M. No evidence for association of the ENPP1 (PC-1) K121Q variant with risk of type 2 diabetes in a Japanese population. J Hum Genet. 2006; 51:559–566.
8. Zhao T, Liu Z, Zhang D, Liu Y, Yang Y, Zhou D, Chen Z, Yu L, Zhang Z, Feng G, et al. The ENPP1 K121Q polymorphism is not associated with type 2 diabetes or obesity in the Chinese Han population. J Hum Genet. 2011; 56:12–16.
9. German JB. Genetic dietetics: nutrigenomics and the future of dietetics practice. J Am Diet Assoc. 2005; 105:530–531.
10. McClenaghan NH. Determining the relationship between dietary carbohydrate intake and insulin resistance. Nutr Res Rev. 2005; 18:222–240.
11. Kosaka K, Noda M, Kuzuya T. Prevention of type 2 diabetes by lifestyle intervention: a Japanese trial in IGT males. Diabetes Res Clin Pract. 2005; 67:152–162.
12. Stefan N, Thamer C, Staiger H, Machicao F, Machann J, Schick F, Venter C, Niess A, Laakso M, Fritsche A, et al. Genetic variations in PPARD and PPARGC1A determine mitochondrial function and change in aerobic physical fitness and insulin sensitivity during lifestyle intervention. J Clin Endocrinol Metab. 2007; 92:1827–1833.
13. Müssig K, Heni M, Thamer C, Kantartzis K, Machicao F, Stefan N, Fritsche A, Häring HU, Staiger H. The ENPP1 K121Q polymorphism determines individual susceptibility to the insulin-sensitising effect of lifestyle intervention. Diabetologia. 2010; 53:504–509.
14. Moore AF, Jablonski KA, Mason CC, McAteer JB, Arakaki RF, Goldstein BJ, Kahn SE, Kitabchi AE, Hanson RL, Knowler WC, et al. The association of ENPP1 K121Q with diabetes incidence is abolished by lifestyle modification in the diabetes prevention program. J Clin Endocrinol Metab. 2009; 94:449–455.
15. Weyrich P, Stefan N, Häring HU, Laakso M, Fritsche A. Effect of genotype on success of lifestyle intervention in subjects at risk for type 2 diabetes. J Mol Med (Berl). 2007; 85:107–117.
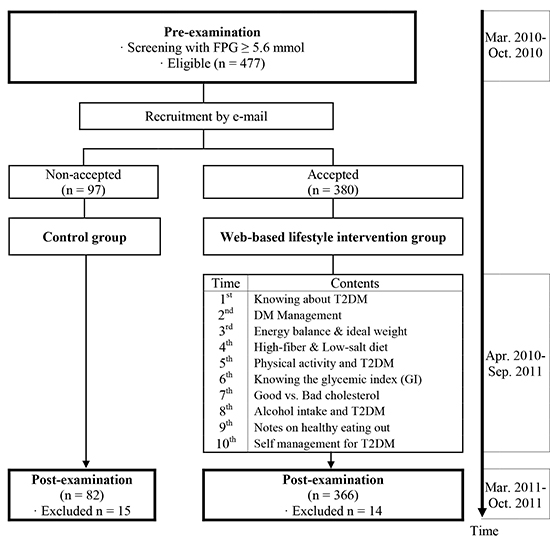
16. Kang JY, Cho SW, Sung SH, Park YK, Paek YM, Choi TI. Effect of a continuous diabetes lifestyle intervention program on male workers in Korea. Diabetes Res Clin Pract. 2010; 90:26–33.
17. Diabetes Prevention Program (DPP) Research Group. The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care. 2002; 25:2165–2171.
18. American Diabetes Association. Bantle JP, Wylie-Rosett J, Albright AL, Apovian CM, Clark NG, Franz MJ, Hoogwerf BJ, Lichtenstein AH, Mayer-Davis E, et al. Nutrition recommendations and interventions for diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2008; 31:S61–S78.
19. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985; 28:412–419.
20. Saely CH, Aczel S, Marte T, Langer P, Hoefle G, Drexel H. The metabolic syndrome, insulin resistance, and cardiovascular risk in diabetic and nondiabetic patients. J Clin Endocrinol Metab. 2005; 90:5698–5703.
21. Chen J, Wildman RP, Hamm LL, Muntner P, Reynolds K, Whelton PK, He J. Association between inflammation and insulin resistance in US nondiabetic adults: results from the Third National Health and Nutrition Examination Survey. Diabetes Care. 2004; 27:2960–2965.
22. Bonora E, Targher G, Alberiche M, Bonadonna RC, Saggiani F, Zenere MB, Monauni T, Muggeo M. Homeostasis model assessment closely mirrors the glucose clamp technique in the assessment of insulin sensitivity: studies in subjects with various degrees of glucose tolerance and insulin sensitivity. Diabetes Care. 2000; 23:57–63.
23. Vogeser M, König D, Frey I, Predel HG, Parhofer KG, Berg A. Fasting serum insulin and the homeostasis model of insulin resistance (HOMA-IR) in the monitoring of lifestyle interventions in obese persons. Clin Biochem. 2007; 40:964–968.
24. Maranghi M, Prudente S, D'Erasmo L, Morini E, Ciociola E, Coletta P, Verrienti A, Arciello S, Copetti M, Pellegrini F, et al. The ectonucleotide pyrophosphatase phosphodiesterase 1 (ENPP1) K121Q polymorphism modulates the beneficial effect of weight loss on fasting glucose in non-diabetic individuals. Nutr Metab Cardiovasc Dis. 2013; 23:505–510.
25. Chandalia M, Grundy SM, Adams-Huet B, Abate N. Ethnic differences in the frequency of ENPP1/PC1 121Q genetic variant in the Dallas Heart Study cohort. J Diabetes Complications. 2007; 21:143–148.
26. Sortica DA, Crispim D, Zaffari GP, Friedman R, Canani LH. The role of ecto-nucleotide pyrophosphatase/phosphodiesterase 1 in diabetic nephropathy. Arq Bras Endocrinol Metabol. 2011; 55:677–685.
27. DeFronzo RA, Ferrannini E. Insulin resistance. A multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic cardiovascular disease. Diabetes Care. 1991; 14:173–194.
28. Kang HM, Kim DJ. Total energy intake may be more associated with glycemic control compared to each proportion of macronutrients in the korean diabetic population. Diabetes Metab J. 2012; 36:300–306.
29. Black MH, Watanabe RM, Trigo E, Takayanagi M, Lawrence JM, Buchanan TA, Xiang AH. High-fat diet is associated with obesity-mediated insulin resistance and β-cell dysfunction in Mexican Americans. J Nutr. 2013; 143:479–485.
30. Harding AH, Sargeant LA, Welch A, Oakes S, Luben RN, Bingham S, Day NE, Khaw KT, Wareham NJ. Fat consumption and HbA(1c) levels: the EPIC-Norfolk study. Diabetes Care. 2001; 24:1911–1916.
31. Gaboon NEA. Nutritional genomics and personalized diet. Egypt J Med Hum Genet. 2011; 12:1–7.
32. Phillips C, Lopez-Miranda J, Perez-Jimenez F, McManus R, Roche HM. Genetic and nutrient determinants of the metabolic syndrome. Curr Opin Cardiol. 2006; 21:185–193.
33. Gami AS, Witt BJ, Howard DE, Erwin PJ, Gami LA, Somers VK, Montori VM. Metabolic syndrome and risk of incident cardiovascular events and death: a systematic review and meta-analysis of longitudinal studies. J Am Coll Cardiol. 2007; 49:403–414.
34. Bu J, Feng Q, Ran J, Li Q, Mei G, Zhang Y. Visceral fat mass is always, but adipokines (adiponectin and resistin) are diversely associated with insulin resistance in Chinese type 2 diabetic and normoglycemic subjects. Diabetes Res Clin Pract. 2012; 96:163–169.
35. Shea JL, King MT, Yi Y, Gulliver W, Sun G. Body fat percentage is associated with cardiometabolic dysregulation in BMI-defined normal weight subjects. Nutr Metab Cardiovasc Dis. 2012; 22:741–747.
36. Lim SY, Ha HS, Kwon HS, Lee JH, Yim HW, Yoon KH, Lee WC, Son HY, Park YM. Factors associated with insulin resistance in a middle-aged non-obese rural population: the Chungju Metabolic Disease Cohort (CMC) Study. Epidemiol Health. 2011; 33:e2011009.
37. Gillies CL, Abrams KR, Lambert PC, Cooper NJ, Sutton AJ, Hsu RT, Khunti K. Pharmacological and lifestyle interventions to prevent or delay type 2 diabetes in people with impaired glucose tolerance: systematic review and meta-analysis. BMJ. 2007; 334:299.
38. Bouchard DR, Baillargeon JP, Gagnon C, Brown C, Langlois MF. Impact of health professionals' contact frequency on response to a lifestyle intervention with individuals at high risk for diabetes. Diabetes Res Clin Pract. 2012; 96:129–134.
39. Choi MJ, Yoo SH, Kim KR, Bae YM, Ahn SH, Kim SS, Min SA, Choi JS, Lee SE, Moon YJ, et al. Effect on glycemic, blood pressure, and lipid control according to education types. Diabetes Metab J. 2011; 35:580–586.
40. Abate N, Chandalia M, Di Paola R, Foster DW, Grundy SM, Trischitta V. Mechanisms of disease: ectonucleotide pyrophosphatase phosphodiesterase 1 as a 'gatekeeper' of insulin receptors. Nat Clin Pract Endocrinol Metab. 2006; 2:694–701.






 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download