1. Nakashima S, Watanabe A, Obama T, Yamada G, Takahashi H, Higami T. Need for preoperative computed tomography-guided localization in video-assisted thoracoscopic surgery pulmonary resections of metastatic pulmonary nodules. Ann Thorac Surg. 2010; 89:212–218.
2. Chen S, Zhou J, Zhang J, Hu H, Luo X, Zhang Y, Chen H. Video-assisted thoracoscopic solitary pulmonary nodule resection after CT-guided hookwire localization: 43 cases report and literature review. Surg Endosc. 2011; 25:1723–1729.
3. Ciriaco P, Negri G, Puglisi A, Nicoletti R, Del Maschio A, Zannini P. Video-assisted thoracoscopic surgery for pulmonary nodules: rationale for preoperative computed tomography-guided hookwire localization. Eur J Cardiothorac Surg. 2004; 25:429–433.
4. Suzuki K, Nagai K, Yoshida J, Ohmatsu H, Takahashi K, Nishimura M, Nishiwaki Y. Video-assisted thoracoscopic surgery for small indeterminate pulmonary nodules: indications for preoperative marking. Chest. 1999; 115:563–568.
5. Seo JM, Lee HY, Kim HK, Choi YS, Kim J, Shim YM, Lee KS. Factors determining successful computed tomography-guided localization of lung nodules. J Thorac Cardiovasc Surg. 2012; 143:809–814.
6. Gossot D, Miaux Y, Guermazi A, Celerier M, Friga J. The hook-wire technique for localization of pulmonary nodules during thoracoscopic resection. Chest. 1994; 105:1467–1469.
7. Pittet O, Christodoulou M, Pezzetta E, Schmidt S, Schnyder P, Ris HB. Video-assisted thoracoscopic resection of a small pulmonary nodule after computed tomography-guided localization with a hook-wire system: experience in 45 consecutive patients. World J Surg. 2007; 31:575–578.
8. Chen W, Chen L, Yang S, Chen Z, Qian G, Zhang S, Jing J. A novel technique for localization of small pulmonary nodules. Chest. 2007; 131:1526–1531.
9. Bernard A. Resection of pulmonary nodules using video-assisted thoracic surgery: the Thorax Group. Ann Thorac Surg. 1996; 61:202–204.
10. Martin AE, Chen JY, Muratore CS, Mayo-Smith WW, Luks FI. Dual localization technique for thoracoscopic resection of lung lesions in children. J Laparoendosc Adv Surg Tech A. 2009; 19:S161–S164.
11. Kawanaka K, Nomori H, Mori T, Ikeda K, Ikeda O, Tomiguchi S, Yamashita Y. Marking of small pulmonary nodules before thoracoscopic resection: injection of lipiodol under CT-fluoroscopic guidance. Acad Radiol. 2009; 16:39–45.
12. Yamagami T, Miura H, Yoshimatsu R, Tanaka O, Ono S, Iehara T, Hosoi H, Nishimura T. Experience of fluoroscopy-aided thoracoscopic resection of pulmonary nodule localised with Lipiodol in a child. J Med Imaging Radiat Oncol. 2011; 55:401–403.
13. Iwasaki Y, Nagata K, Yuba T, Hosogi S, Kohno K, Ohsugi S, Kuwahara H, Takemura Y, Yokomura I. Fluoroscopy-guided barium marking for localizing small pulmonary lesions before video-assisted thoracic surgery. Respir Med. 2005; 99:285–289.
14. Yoshida J, Nagai K, Nishimura M, Takahashi K. Computed tomography-fluoroscopy guided injection of cyanoacrylate to mark a pulmonary nodule for thoracoscopic resection. Jpn J Thorac Cardiovasc Surg. 1999; 47:210–213.
15. Nomori H, Horio H. Colored collagen is a long-lasting point marker for small pulmonary nodules in thoracoscopic operations. Ann Thorac Surg. 1996; 61:1070–1073.
16. McConnell PI, Feola GP, Meyers RL. Methylene blue-stained autologous blood for needle localization and thoracoscopic resection of deep pulmonary nodules. J Pediatr Surg. 2002; 37:1729–1731.
17. Hu J, Zhang C, Sun L. Localization of small pulmonary nodules for videothoracoscopic surgery. ANZ J Surg. 2006; 76:649–651.
18. Wicky S, Mayor B, Cuttat JF, Schnyder P. CT-guided localizations of pulmonary nodules with methylene blue injections for thoracoscopic resections. Chest. 1994; 106:1326–1328.
19. Vandoni RE, Cuttat JF, Wicky S, Suter M. CT-guided methylene-blue labelling before thoracoscopic resection of pulmonary nodules. Eur J Cardiothorac Surg. 1998; 14:265–270.
20. Lenglinger FX, Schwarz CD, Artmann W. Localization of pulmonary nodules before thoracoscopic surgery: value of percutaneous staining with methylene blue. AJR Am J Roentgenol. 1994; 163:297–300.
21. Ikeda K, Nomori H, Mori T, Kobayashi H, Iwatani K, Yoshimoto K, Kawanaka K. Impalpable pulmonary nodules with ground-glass opacity: success for making pathologic sections with preoperative marking by lipiodol. Chest. 2007; 131:502–506.
22. Nomori H, Horio H, Naruke T, Suemasu K. Fluoroscopy-assisted thoracoscopic resection of lung nodules marked with lipiodol. Ann Thorac Surg. 2002; 74:170–173.
23. Watanabe K, Nomori H, Ohtsuka T, Kaji M, Naruke T, Suemasu K. Usefulness and complications of computed tomography-guided lipiodol marking for fluoroscopy-assisted thoracoscopic resection of small pulmonary nodules: experience with 174 nodules. J Thorac Cardiovasc Surg. 2006; 132:320–324.
24. Kim YD, Jeong YJ, I H, Cho JS, Lee JW, Kim HJ, Lee SH, Kim DH. Localization of pulmonary nodules with lipiodol prior to thoracoscopic surgery. Acta Radiol. 2011; 52:64–69.
25. Mayo JR, Clifton JC, Powell TI, English JC, Evans KG, Yee J, McWilliams AM, Lam SC, Finley RJ. Lung nodules: CT-guided placement of microcoils to direct video-assisted thoracoscopic surgical resection. Radiology. 2009; 250:576–585.
26. Lee NK, Park CM, Kang CH, Jeon YK, Choo JY, Lee HJ, Goo JM. CT-guided percutaneous transthoracic localization of pulmonary nodules prior to video-assisted thoracoscopic surgery using barium suspension. Korean J Radiol. 2012; 13:694–701.
27. Kamiyoshihara M, Ishikawa S, Morishita Y. Pulmonary cryptococcosis diagnosed by video-assisted thoracoscopic surgery with CT-guided localization: report of a case. Kyobu Geka. 2000; 53:795–797.
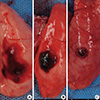
28. Kwon WJ, Kim HJ, Jeong YJ, Lee CH, Kim KI, Kim YD, Lee JH. Direct lipiodol injection used for a radio-opaque lung marker: stability and histopathologic effects. Exp Lung Res. 2011; 37:310–317.
29. Jang HS. Effect of drugs for preoperative localization of thoracoscopy to histopathologic change in rabbit lung. Seoul: the Catholic University of Korea;2000. 27. Dissertation.
30. Okumura T, Kondo H, Suzuki K, Asamura H, Kobayashi T, Kaneko M, Tsuchiya R. Fluoroscopy-assisted thoracoscopic surgery after computed tomography-guided bronchoscopic barium marking. Ann Thorac Surg. 2001; 71:439–442.







 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download