Abstract
This phase II clinical trial was conducted to compare the immunogenicity and safety of a newly developed tetanus-reduced diphtheria (Td) vaccine (GC1107-T5.0 and GC1107-T7.5) and control vaccine. This study was also performed to select the proper dose of tetanus toxoid in the new Td vaccines. Healthy adolescents aged between 11 and 12 yr participated in this study. A total of 130 subjects (44 GC1107-T5.0, 42 GC1107-T7.5 and 44 control vaccine) completed a single dose of vaccination. Blood samples were collected from the subjects before and 4 weeks after the vaccination. In this study, all subjects (100%) in both GC1107-T5.0 and GC1107-T7.5 groups showed seroprotective antibody levels (≥ 0.1 U/mL) against diphtheria or tetanus toxoids. After the vaccination, the geometric mean titer (GMT) against diphtheria was significantly higher in Group GC1107-T5.0 (6.53) and GC1107-T7.5 (6.11) than in the control group (3.96). The GMT against tetanus was 18.6 in Group GC1107-T5.0, 19.94 in GC1107-T7.5 and 19.01 in the control group after the vaccination. In this study, the rates of local adverse reactions were 67.3% and 59.1% in GC1107-T5.0 and GC1107-7.5, respectively. No significant differences in the number of adverse reactions, prevalence and degree of severity of the solicited and unsolicited adverse reactions were observed among the three groups. Thus, both newly developed Td vaccines appear to be safe and show good immunogenicity. GC1107-T5.0, which contains relatively small amounts of tetanus toxoid, has been selected for a phase III clinical trial.
Diphtheria is a toxin-mediated respiratory disease caused by Corynebacterium diphtheriae with a high mortality rate and a range of symptoms through a systemic blood-borne infection (1). Tetanus is also a fatal disease caused by the exotoxin of Clostridium tetani, an anaerobic Gram-positive bacillus, which is ubiquitous in the soil and gastrointestinal tract of many animals. The organism can invade through a contaminated wound, as well as after surgery, burns, acute otitis media, periodontal infection, animal bites, miscarriage and pregnancy (2).
Natural protective immunity is not formed after being exposed to diphtheria and tetanus. According to a diphtheria and tetanus seroepidemiology study conducted in Korea, the seroprotective antibodies for these infections are not maintained in adults over the age of 20 yr (3-5). Therefore, the necessity of tetanus-reduced diphtheria (Td) vaccination became apparent, and was introduced in Korea in 2003 (6).
The Td vaccine currently distributed in Korea is manufactured from imported concentrates, as there is no manufacturer of the concentrate of this Td vaccine in Korea. Accordingly, to produce Td vaccine self-reliantly, the Korea Green Cross Corporation developed a vaccine, and obtained approval for a phase I clinical trial from the Korea Food & Drug Administration in 2009. Evidence of the immunogenicity and safety was offered by injecting this vaccine into the deltoid muscle of healthy adult men (7). The Td vaccine (GC1107-T7.5) used in the phase I clinical trial contained 7.5 Lf (flocculation units) of tetanus toxoid, which is higher than the 5 Lf tetanus toxoid contained in the Td vaccine distributed worldwide. The recent outbreak of pertussis has led to the recommendation of combined Tetanus, Diphtheria and Pertussis (Tdap) vaccinations to adolescents and adults in epidemic areas with a minimum 5-yr vaccination interval. In this situation, the high rate of adverse reactions of Td vaccination may create a great deal of concern due to this short interval of vaccination.
The objective of this study was to compare the immunogenicity and safety of a newly developed Td vaccine (GC1107-T5.0 and GC1107-T7.5) and control vaccine (Td pure®, SK Chemical, Seongnam, Korea). At the same time, this study was performed to select the proper dose of tetanus toxoid in the new Td vaccines for phase III clinical study.
Healthy adolescents aged between 11 and 12 yr were invited to participate in this study. This clinical trial was a double-blind, randomized, multi-center trial, and was conducted in the pediatric departments of ten hospitals (The Catholic University of Korea, Seoul St. Mary's Hospital, St. Vincent's Hospital, Daejeon St. Mary's Hospital, Incheon St. Mary's Hospital and Bucheon St. Mary's Hospital, Wonju Yeonsei University Hospital, Keimyung University Dongsan Medical Center, Changwon Fatima Hospital, Chonnam National University Hospital, Korea Cancer Center Hospital). To ensure blindness among these trials, the clinical vaccine in dose group 1, dose group 2 and control vaccine group were packaged with the same appearance. Details of the subjects' random code were managed under sealed conditions and were not opened until the end of the trial.
Based on the premise of a 98% production rate of diphtheria and tetanus protective antibody, a 5% allowable error for the trial and 5% level of significance, the necessary number of subjects was found to be 31 per group; 35 per group considering a 10% wastage rate (r = 0.1). The section standard of the subjects were children aged eleven to twelve, who had been vaccinated 5 times including 3 basic diphtheria-tetanus-acellular pertussis (DTaP) vaccinations and 2 booster DTaP vaccinations before they were 6 yr of age. Patients with a diphtheria antitoxin antibody titer and tetanus antitoxin antibody titer > 1.0 IU/mL before the clinical trial, no proven vaccination history, and patients treated for fever, acute disease or chronic diseases were excluded. Antibody titers were measured before diphtheria and tetanus toxoid vaccination. If the diphtheria antitoxin antibody titer and tetanus antitoxin antibody titer were < 1.0 IU/mL, the newly developed Td vaccine and control vaccine were injected by a random allocation. Blood sampling was conducted four weeks after vaccination to measure the antibody titer. All subjects were observed for immediate adverse reactions for 30 min after vaccination. During the period of the visit for blood sampling and 2 weeks after blood sampling, the incidence of adverse reactions after vaccination was recorded through a diary card and telephone call.
The new Td vaccine used in dose group 1 was a GC1107-T5.0 vaccine containing tetanus toxoid 5.0 Lf and diphtheria toxoid 2.5 Lf. The new Td vaccine used in dose group 2 was a GC1107-T7.5 vaccine containing tetanus toxoid 7.5 Lf and diphtheria toxoid 2.5 Lf. The active control vaccine used in dose control group was a Td pure® (SK Chemical, Seongnam, Korea) containing tetanus toxoid 5.0 Lf and diphtheria toxoid 2.5 Lf. The diphtheria seed bacteria of the GC1107-T5.0 vaccine and GC1107-T7.5 vaccine was the Corynebacterium diphtheriae Park Williams #8 strain. The tetanus seed bacteria was the Clostridium tetani Harvard strain. The diphtheria seed bacteria of the control vaccine group was also the Corynebacterium diphtheriae Park Wiliams #8 strain, but the tetanus seed bacteria was the Clostridium tetani Massachusetts F1 strain. Both the newly developed Td vaccine and control vaccine included the adjuvant and alum salt, and were pre-filled vaccines with a dose of 0.5 mL. The colors were light yellow or white, which could not be identified visually, and the vaccines were preserved in a refrigerator at 2-8℃. The vaccine was injected in the deltoid muscle of the selected subjects, and any immediate hyperimmune reaction was observed carefully for thirty minutes after the injection.
Blood samples (3-5 mL) were collected before the injection and 4 weeks after the injection. Serum samples were kept at -70℃ until analysis. Two different types of enzymes linked immunosorbent assay kits (kit number RE56191 for diphtheria and RE56901 for tetanus) from the same company (IBL, Hamburg, Germany) were used to determine the serum antibody levels to diphtheria and tetanus according to the manufacturer's instructions. The antibody levels ≥ 0.1 U/mL against diphtheria or tetanus toxoid were considered indicative of seroprotection. A group comparison was also conducted by calculating the geometric mean titer (GMT) against diphtheria and tetanus toxoid before and after vaccination.
The subjects' parents were given diary cards and asked to record any solicited local adverse reactions or solicited systemic adverse reactions that occurred during the 4 week (Days 0-28) follow-up after vaccination. All subjects were monitored for an additional 2 week (Days 42-49) safety follow-up period for unscheduled hospital visits and serious unsolicited adverse events. The symptom intensity was graded on a scale of 0-3 with 'Grade 0' representing an absence of symptoms and 'Grade 3' representing a symptom that prevented normal activity, redness or swelling with a diameter ≥ 30 mm, or an axillary temperature ≥ 39.0℃. All unsolicited adverse events and serious adverse events that occurred during the 6 week study period were also monitored. The causal relationships between the adverse events and vaccination were evaluated. For all adverse reactions, it was followed up until it was resolved, the patient's state became stable or the relationship between the adverse reaction and vaccination was evaluated.
For the demographic status, the mean, median, standard deviation, minimum value and maximum values, were used to determine if there was a significant difference among the groups. The differences among the groups were indicated by a t-test. For immunogenicity analysis, the protective antibody titers of diphtheria and tetanus were evaluated after the clinical trial vaccination with the 95% confidence interval. Before and after vaccination, GMT was calculated with the 95% confidence interval. The ratios before vaccination to after vaccination were calculated with the 95% confidence interval. In safety surveillance, for Group GC1107-T5.0, Group GC1107-T7.5 and the control group, all solicited local and systemic adverse reactions observed up to seven days after vaccination and all unsolicited adverse reactions observed up to 42 days after vaccination were evaluated. The number of adverse reactions and the percentage among study subjects were calculated with the 95% confidence interval. A chi-square test or Fisher's Exact test were used to compare the adverse reactions of the three groups.
The protocol and associated documents were reviewed and approved by the institutional review board of each study hospital. The numbers of the approved documents of each hospital are listed as follows: Seoul St. Mary's Hospital (XC11MDMS0089K), Daejeon St. Mary's Hospital (XC11MDMS0089D), Incheon St. Mary's Hospital (XC11MDMS0089O), Bucheon St. Mary's Hospital (XC11MDMS0089H), St. Vincent's Hospital (XC11MDMS0089V), Wonju Christian Hospital (CR111020), Chonnam National University Hospital (CNUH-2011-122), Changwon Fatima Hospital (11-15), and Korea Cancer Center Hospital (K-1108-001-003), Keimyung University Dongsan Medical Center (11-155). This clinical trial was carried out according to Korean Good Clinical Practice (KGCP: Korea Food and Drug Administration Registration No. 2009-211, December 22, 2009) and ICH standard, and observed the principle of the Helsinki Declaration prioritizing the subjects' rights, benefits and safety. The principal investigator and people in charge received informed consent from the study participants or legal guardians after explanation of the attributes, scope, and expected result of this clinical trial.
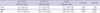
A total of 223 subjects were enrolled in this clinical trial. Among these subjects, a total of 77 subjects was eliminated during the screening process; 6 and 71 subjects withdrew voluntarily, or were exempted due to violation of selection criteria, respectively. A total of 146 subjects was randomized. Of the 146 (safety analyzed subjects) subjects who completed the trial, 15 were eliminated; 4 for violations of the selection and exclusion criteria, 10 for randomization errors, and 1 for clearing blindness. Overall, 130 (per protocol analyzed subjects) were included; 44 in the GC1107-T5.0 group, 42 in the GC1107-T7.5 group and 44 in the control group (Fig. 1). The safety analyzed subjects included 68 (46.58%) males and 78 (53.42%) females: 17 (34.69%) males and 32 (65.31%) females in Group GC1107-T5.0; 24 (48.98%) males and 25 (51.02%) females in Group GC1107-T7.5; and 27 (56.25%) males and 21 (43.75%) females in the control group. The gender ratio, age, height and weight were similar in the three groups (Table 1).
After the clinical trial vaccination according to the protocol, protective antibody to diphtheria was produced in 100% of the three groups. The GMT against diphtheria before the vaccination was 0.34 in Group GC1107-T5.0, 0.31 in Group GC1107-T7.5 and 0.31 in the control group. GMT increased in all three groups after the vaccination. The GMT was 6.53 in Group GC1107-T5.0, 6.11 in Group GC1107-T7.5 and 3.96 in the control group. The GMT was significantly higher in Group GC1107-T5.0 and GC1107-T7.5 than in the control group after the vaccination (Table 2).
Before the vaccination, the GMT against tetanus was 0.33 in Group GC1107-T5.0, 0.26 in Group GC1107-T7.5 and 0.30 in the control group. GMT level increased in all three groups after the vaccination. After the vaccination, it was 18.6 in Group GC1107-T5.0, 19.94 in Group GC1107-T7.5 and 19.01 in the control group.
The geometric mean titer ratio (GMR) of diphtheria before and after the vaccination was 19.45 in Group GC1107-T5.0, 19.83 in Group GC1107-T7.5 and 12.88 in the control group. The GMR of tetanus before and after the vaccination was 55.52 in Group GC1107-T5.0, 75.60 in Group GC1107-T7.5 and 62.34 in the control group. The GC1107-T5.0 group showed similar immunogenicity against tetanus when compared to the control group, but GMT level of anti-tetanus antibody in the GC1107-T5.0 group was significantly higher than that of the control group (Table 3).
Adverse reactions were observed in 122 cases in 36 subjects (73.5%, 36/49 people) in Group GC1107-T5.0, 103 cases in 33 subjects (67.4%, 33/49) in Group GC1107-T7.5, and 90 cases in 30 subjects (62.5%, 30/48) in the control vaccine group. The total number of adverse reactions was similar in the three groups. Solicited adverse reactions were observed in 110 cases in 34 subjects (69.4%, 34/49 people) in Group GC1107-T5.0, 85 cases in 30 subjects (61.2%, 30/49) in Group GC1107-T7.5 and 80 cases in 29 subjects (60.4%, 29/48) in the control group. No significant differences in the solicited adverse reactions were observed among the groups.
An analysis of the solicited local adverse reactions revealed the following. In Group GC1107-T5.0, 31 subjects experienced pain, (63.3%, 31 cases), 24 subjects experienced induration, (49.0%, 24 cases), 15 subjects experienced redness (30.6%, 15 cases) and 15 subjects experienced swelling, (30.6%, 15 cases). In Group GC1107-T7.5, 29 subjects experienced pain, (59.2%, 29 cases), 17 subjects experienced induration, (34.7%, 17 cases), 12 subjects experienced redness (24.5%, 12 cases) and 10 subjects experienced swelling (20.4%, 10 cases). In the control vaccine group, 29 subjects experienced pain, (60.4%, 29 cases), 20 subjects experienced induration, (41.7%, 20 cases), 14 subjects experienced redness, (29.2%, 14 cases) and 12 subjects experienced swelling, (25%, 12 cases). The adverse events in each group were all adverse drug events. For the solicited local adverse reactions over 'Grade 3', there were 3 subjects (6.1%) in Group GC1107-T5.0 (2 cases of 'pain' and 2 cases of 'redness'), 3 subjects (6.1%) in Group GC1107-T7.5 (1 case of 'redness' and 3 cases of 'swelling') and 3 subjects (6.3%) in the control group (2 cases of 'redness' and 1 case of 'swelling').
For solicited systemic adverse reactions, in Group GC1107-T5.0, 11 subjects experienced 'myalgia' (22.5%, 11 cases), 6 subjects experienced 'headache' (12.2%, 6 cases), 3 subjects experienced 'joint pain' (6.1%, 3 cases), 1 subject experienced 'rash' (2.0%, 1 case), 2 subjects experienced 'indigestion' (4.1%, 2 cases) and 1 subject experienced chill (2.0%, 1 case). In Group C1107-T7.5, 6 subjects experienced 'myalgia' (12.2%, 6 cases), 5 subjects experienced 'headache' (10.2%, 5 cases), 2 subjects experienced 'rash'(4.1%, 2 cases), 1 subject experienced 'indigestion'( 2.0%, 1 case), 1 subject experienced 'chill' (2.0%, 1 case), 1 subject experienced 'sweating' (2.0%, 1 case) and 1 subject experienced 'allergic reaction' (2.0%, 1 case). In the control group, 2 subjects experienced 'myalgia' (4.2%, 2 cases) and 3 subjects experienced 'headache' (6.3%, 3 cases). The adverse events presented in each group were all adverse drug events. For the solicited systemic adverse events over 'Grade 3', 1 subject (2.0%) in Group GC1107-T5.0 experienced a case of 'joint pain', 1 subject (2.0%) in Group GC1107-T7.5 experienced a case of 'indigestion', but there were no such events in the control vaccine group (Table 4).
An analysis of the unsolicited adverse events revealed 12 adverse reactions in 10 subjects (20.4%, 10/49 people) in Group GC1107-T5.0, 18 cases in 11 subjects (22.5%, 11/49 people) in Group GC1107-T7.5 and 10 cases in 9 subjects (18.8%, 9/48 people) in the control vaccine group.
No significant differences in the number of adverse reactions, prevalence and degree of severity of the solicited and unsolicited adverse reactions were observed among the 3 groups. In addition, there was no statistical significance in the rate of solicited adverse events over grade 3 among the three groups. All adverse reactions resolved within 3 days without the need for medical management.
Tetanus is an important infectious disease that still affects hundreds of thousands of people annually worldwide (2,8), and small number of tetanus cases continue to be reported in our country (9). Also, diphtheria occurs in regions where vaccinations are not performed routinely (1,10). Therefore, prevention of these diseases through vaccination is essential. In this aspect, tetanus and reduced diphtheria (Td) vaccine is provided for adolescents (11 to 12 yr of age) to maintain long-term immunity as an National Immunization Program (NIP) vaccine in Korea since 2005 (11).
As of 2012, only one Td vaccine, manufactured by SK Chemical, is currently available, and there is no manufacturer of concentrates of diphtheria and tetanus toxoid in Korea. To produce Td vaccine self-reliantly, the Korea Green Cross Corporation developed 'GC1107'. The completion of 'GC 1107' is expected to resolve the significant instability in vaccine supply and to allow the supply of raw material from domestic sources. Moreover, national competitiveness will be strengthened, which will contribute to better public welfare.
As a main objective finding of our study, the new Td vaccines (GC1107-T5.0 and GC1107-T7.5) showed marked boost responses against diphtheria and tetanus. In fact, the seroprotection rates of GC1107-T5.0 and GC1107-T7.5 against diphtheria and tetanus were 100%, which are the same as those of SK-Chemical Td pure® (100%) in studies conducted by Kang et al. (11) and Lee et al. (12). The anti-toxoid diphtheria and tetanus antibody levels after vaccination were more than 1.0 IU/mL in all subjects who received the new Td vaccines. The comparison vaccine group showed similar results.
The anti-diphtheria antibody levels after vaccinations were sharply elevated in all groups. However, the anti-diphtheria antibody levels of the new Td vaccine groups were significantly higher than the level of the active control group (Table 2). This result was not seen in previous phase I study which was conducted by Lee et al. (7). We hypothesize that this difference may be caused by the high titer of diphtheria toxoid in the new Td vaccines. The new Td vaccine was developed with an enhanced manufacturing method that consists of fermentation followed by a purification process containing gel filtration. Hence, the diphtheria toxoid titer per protein unit of the new Td vaccines is higher than that of the control vaccine. Also, anti-tetanus anti-body levels after vaccinations were markedly elevated in all groups. And the anti-tetanus antibody level of GC1107-T7.5 group was higher than the level of the control group (Table 3). This result was similar to a previous phase I study which was conducted by Lee et al. (7). As mentioned in the method of this study, the tetanus toxoid level of GC1107-T7.5 is higher than that of control vaccine. This result may be caused by the higher level of tetanus toxoid. There are few immunogenicity studies concerned with Td vaccines, with especially limited data in adolescents. However, variable booster immune responses to Td vaccines have been reported in previous studies (13-16). These investigators suggest that the extent of the antibody levels after Td vaccinations may show inter-individual variability depending on immune responses, different individual vaccination backgrounds, and different Td vaccines. Unfortunately, the number of study subjects in the current study was not sufficient to evaluate the causes of these differences. Also, this study has the same limitation, emphasizing the need to conduct large-scale clinical studies to confirm the causalities and differences in the future.
Generally, the Td vaccine is a safer vaccine with lower rates of adverse reactions than DTaP. The common local adverse reactions include pain in the injection site (55%) followed by swelling (13.9-19.8%) and redness (13.9-19.6%). Systemic adverse reactions include headache (30.9-37.5%), fatigue (30.9-37.5%), gastrointestinal problems (6.9-17.4%) and fever (5.4-5.6%) (13, 17-19). According to Lee et al. (12), the local adverse reaction rate and systemic adverse reaction rate in Korean children was 82.6% and 25%, respectively. The local adverse reactions included pain (69.7%), swelling (48.5%), redness (48.5%) and itching sensation (9.1%), whereas systemic adverse reactions included fatigue (12.9%), headache (6.1%), fever (3.8%), gastrointestinal problems (3%) and respiratory symptoms (3%).
In this study, the rates of local adverse reactions were 67.3% and 59.1% in GC1107-T5.0 and GC110-7.5, respectively, which were slightly lower than reported by Lee et al. (12). The rates of systemic adverse reactions were similar in groups GC1107-T5.0, GC110-7.5 and those reported by Lee et al. (12). The type of local adverse reactions in the 2 new Td vaccines included pain, induration and redness, which were similar to other studies. The type of systemic adverse reactions included myalgia and headache, which were similar to those reported in other studies (12). The rates and degree of solicited and unsolicited adverse reactions, as well as the rates of severe, solicited grade 3 adverse reactions were similar. All the adverse reactions resolved within 3 days of vaccination. There were no serious adverse reactions, such as Arthus reaction or anaphylaxis, requiring emergency management. Also there was no relationship between the extent of antibody increase and adverse reactions. We suggest that this result may be correlated with low antibody titers against diphtheria and tetanus in our study subjects before vaccination.
Recently, due to outbreaks of pertussis in adolescents and adults, a Tdap vaccination is recommended with a 5 yr minimum vaccination interval in epidemic areas. In this case, the vaccination interval is short and there is a concern that it can cause adverse vaccination effects after Td vaccination. Recently some investigators indicate that the risk of those adverse reactions varied by age and by prior receipt of tetanus and diphtheria containing vaccines, with short intervals less than 2 yr associated with an increased incidence of local injection site reactions (20-22). In this aspect, it is very important to avoid undesirable adverse effects of tetanus and diphtheria vaccines, and the development of more safe and immunogenic Td vaccines will be needed.
Both GC1107-T5.0 and GC1108-T7.5 vaccines showed 100% seroprotection rates against diphtheria and tetanus with high antibody titers. This result indicates that the new Td vaccines are effective for preventing diphtheria and tetanus. These vaccines showed similar low rates of adverse reactions when compared to SK-Chemical Td pure®. Thus, both the new Td vaccines appear to be safe and show good immunogenicity. Of the 2 vaccines, GC1107-T5.0, which contains relatively small amounts of tetanus toxoid, has been finally selected for a phase III clinical study on the basis of the results.
Figures and Tables
Table 2
GMT against diphtheria levels and ratio before and after vaccination in study groups and control group
ACKNOWLEDGMENTS
All of the authors declare no conflict of interest expect for the financial support of this clinical trial from the Green Cross Co. The support made no influence on the trial, analysis, and writing. Dong Ho Ahn, one of co-authors, is an employee of the Green Cross Co., but he was not involved in data acquisition, analysis, and writing.
References
1. Vitek CR, Wharton M. Plotkin SA, Orenstein WA, Offit PA, editors. Diphtheria toxoid. Vaccines. 2008. 5th ed. Philadelphia: WB Saunders;139–156.
2. Wassilak SGF, Roper MH, Kretsinger K, Orenstein WA. Plotkin SA, Orenstein WA, Offit PA, editors. Tetanus toxoid. Vaccines. 2008. 5th ed. Philadelphia: WB Saunders;805–840.
3. Kang JH, Hur JK, Kim JH, Lee KI, Park SE, Ma SH, Lee MS, Baek SY, Hong SH, Min HK. Age related seroepidemiological study of diphtheria among Koreans. Korean J Infect Dis. 2000. 32:1–7.
4. Kang JH, Hur JK, Kim JH, Lee KI, Park SE, Ma SH, Lee MS, Ban SJ, Hong SH, Cho DH, et al. Age related serosurvey of immunity to tetanus in Korean populations. Korean J Infect Dis. 2001. 33:104–111.
5. Lee SY, Kim JS, Ahn JH, Choi JH, Ma SH, Park JS, Kim HM, Kang JH. Immunoassay of diphtheria and tetanus according to ages. Infect Chemother. 2012. 44:62–66.
6. Kang JH. The need of Td vaccination according to the changes of tetanus and diphtheria immunity. J Korean Med Assoc. 2008. 51:127–136.
7. Lee S, Park WB, Shin KH, Ahn DH, Yoon SH, Cho JY, Shin SG, Jang IJ, Yu KS. Immunogenicity and safety of a single intramuscular dose of a diphtheria-tetanus toxoid (Td) vaccine (GC1107) in Korean adults. Vaccine. 2011. 29:7638–7643.
8. Centers for Disease Control and Prevention. Epidemiology and prevention of vaccine-preventable diseases. 2004. 8th ed. Atlanta: CDC;65–73.
9. Shin DH, Yu HS, Park JH, Shin JH, Kim SJ. Recently occurring adult tetanus in Korea: emphasis on immunization and awareness of tetanus. J Korean Med Sci. 2003. 18:11–16.
10. Pickering LK, Baker CJ, Kimberlin DW, Long SS. Diphtheria: Red Book: 2009 report of the Committee on Infectious Diseases. 2009. 28th ed. Elk Grove Village: American Academy of Pediatrics;280–283.
11. Kang JH, Lee SY, Kim HM, Park JS, Ma SH. The assessment of adult Td vaccine usefulness. KFDA. 2007. 32–33.
12. Lee SY, Kwak GY, Nam CH, Kim JH, Hur JK, Lee KY, Park JS, Kim HM, Kang JH. Immunogenicity and safety of diphtheria-tetanus vaccine in pre-adolescent and adolescent South Koreans. Vaccine. 2009. 27:3209–3212.
13. Choi JH, Choo EJ, Huh A, Choi SM, Eom JS, Lee JS, Park SH, Kang JH. Immunogenicity and safety of diphtheria-tetanus vaccine in adults. J Korean Med Sci. 2010. 25:1727–1732.
14. Gil A, Dal-Ré R, González A, Lasheras L, Aguilar L, del Rey J. Immunogenicity and safety of a tetanus-diphtheria vaccine (adult type): clinical trial in adults. Med Clin (Barc). 1995. 104:126–129.
15. Turnbull FM, Heath TC, Jalaludin BB, Burgess MA, Ramalho AC. A randomized trial of two acellular pertussis vaccines (dTpa and pa) and a licensed diphtheria-tetanus vaccine (Td) in adults. Vaccine. 2000. 19:628–636.
16. Bartels I, Jüngert J, Lugauer S, Stehr K, Heininger U. Immunogenicity and reactogenicity of a single dose of a diphtheria-tetanus: acellular pertussis component vaccine (DTaP) compared to a diphtheria: tetanus toxoid (Td) and a diphtheria toxoid vaccine (d) in adults. Vaccine. 2001. 19:3137–3145.
17. Mark A, Carlsson RM, Granström M. Subcutaneous versus intramuscular injection for booster DT vaccination of adolescents. Vaccine. 1999. 17:2067–2072.
18. Blennow M, Granström M, Strandell A. Adverse reactions after diphtheria-tetanus booster in 10-year-old schoolchildren in relation to the type of vaccine given for the primary vaccination. Vaccine. 1994. 12:427–430.
19. Southern J, Andrews N, Burrage M, Miller E. Immunogenicity and reactogenicity of combined acellular pertussis/tetanus/low dose diphtheria vaccines given as a booster to UK teenagers. Vaccine. 2005. 23:3829–3835.
20. Relyveld EH, Bizzini B, Gupta RK. Rational approaches to reduce adverse reactions in man to vaccines containing tetanus and diphtheria toxoids. Vaccine. 1998. 16:1016–1023.
21. Jackson LA, Yu O, Belongia EA, Hambidge SJ, Nelson J, Baxter R, Naleway A, Gay C, Nordin J, Baggs J, et al. Frequency of medically attended adverse events following tetanus and diphtheria toxoid vaccine in adolescents and young adults: a Vaccine Safety Datalink Study. BMC Infect Dis. 2009. 9:165.
22. Lodolce AE. Shortened interval between tetanus vaccines. Ann Pharmacother. 2012. 46:884–888.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download